-
PDF
- Split View
-
Views
-
Cite
Cite
Muhsin Mohammed Ahmed, Farman Uthman Shareef, Jeza Muhamad Abdul Aziz, San Khasraw Mohammed, Hawnaz Atta Karim, Mihraban Abdulrahman Maulud, Daro Hadi Fareeq, Dlivan Fattah Aziz, Muhammad Jabar Rashid, Unusual acute right abdominal pain. Distal ileum mesenteric cystic lymphangioma in adult, a rare case and literature review, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae322, https://doi.org/10.1093/jscr/rjae322
Close - Share Icon Share
Abstract
Lymphangiomas in the peritoneal cavity are rare in adults, with most cases occurring in children. We present the case of a 49-year-old woman who was admitted with severe lower abdominal pain. The diagnostic assessment revealed a multiloculated cystic structure in the mesentery of the distal ileum, suggesting a lymphangioma. The patient underwent laparotomy and resection, with successful removal of the mass. Histopathological examination confirmed the diagnosis of intestinal lymphangioma, a rare benign vascular neoplasm of the small bowel. Postoperatively, the patient experienced resolution of postoperative ileus and mild back and abdominal pain, with no complaints during follow-up. Awareness of this uncommon condition is crucial for accurate diagnosis and appropriate treatment. Surgical resection, supported by radiological and histopathological investigations, is the primary treatment modality for symptomatic lymphangioma. Regular follow-up with imaging may be necessary to monitor recurrence.
Introduction
In adults, lymphangiomas occurring in the peritoneal cavity are rare [1]. Cystic lymphangiomas in the abdomen are usually found in the mesenteric region rather than in the omentum, probably because of its rich lymphatic network [2]. Right-sided mesocolonic lesions are more common than left-sided lesions [3].
The clinical findings of cystic lymphangiomas vary from asymptomatic to acute abdominal pain [4]. The most useful tool for diagnosis is radiological examination, histopathology will confirm the case, and surgical resection is the treatment of this disease [2]. Mesenteric cystic lymphangioma is considered a rare benign tumor that mostly occurs mainly in children; and is theoretically localized in the axilla, neck, and head [5]. Sixty-five percent of Mesenteric cystic lymphangiomas are present at birth, 90% of all patients are diagnosed before the age of 2 years, and over 95% of lymphangiomas are found in the head, neck, and axillary regions. Isolated small bowel lesions are seen in <1% of cases but account for 70% of all intraperitoneal lymphangiomas [6]. Here, we present the case of an adult female with mesenteric lymphangioma. This work has been reported in line with the Surgical Case Report (SCARE) 2020 Criteria [7].
Case presentation
A 49-year-old woman with a history of severe lower abdominal pain was admitted to our hospital. The patient had no vomiting, normal bowel motion, history of weight loss, or fever. The pain gradually increased over time. She had hypertension and hypothyroidism and was treated with thyroxin and concor tablets. She did not have a drug allergy and was a smoker. Her pain was worse after eating, and she had acute pain in her right abdominal, flank, and back. The patient’s blood pressure was 160/90 mmHg, pulse rate was 90 bpm, spo2 was 97%, and blood sugar was 97 mg/dl. Physical examination revealed that the patient was well, with no palpable abdominal mass. The patient lay comfortably in bed, with no distended abdomen, no scars, and soft and normal bowel sounds.
The laboratory hematology results revealed abnormalities such as, WBC (11.93 × 103 /μl), platelet (417 × 103/μl), TSH (5.87 IU/ml), total T3 (1.58 nmol/l), and total T4 (66.03 nmol/l). Her blood urea level was (28 mg. dl) and her serum creatinine level was (0.67 mg. dl). Abdominal sonography showed a normal uterus size, clear cavity, mildly bulky myometrium heterogeneous texture adenomyosis 6 mm posterior mural fibroid, normal endometrium, thickness 2 mm, and no cervical mass. A separated tubular fluid-filled structure was seen in the pelvis superior to the uterus, mainly on the right side; no obvious peristalsis could be seen within it during the examination, and the hydrosalpinx dilated the small bowel loops (ileum) (Fig. 1). For further investigation and clearer vision, magnetic resonance imaging (MRI) or computed tomography (CT) with oral contrast is recommended.
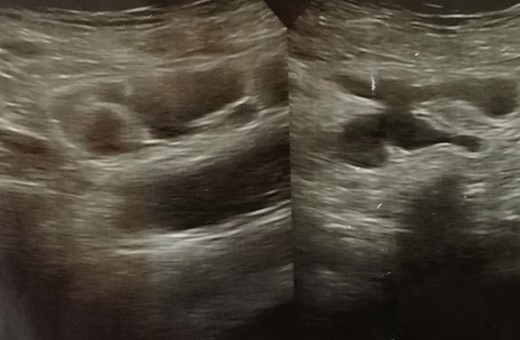
As recommended, Pelvic MRI with intravenous contrast was performed. The result showed evidence of tubular fluid-containing structures in continuity with bowel loops in the right lower abdomen anterior to the uterus. However, no abnormal enhancement or fluid levels were observed after IV contrast administration. The small bowel loops appeared non-dilated. The endometrial thickness was normal. There was an increase in the surrounding junctional zone, suggesting adenomyosis. Additionally, CT revealed a clearly defined multiloculated, hypodense (mostly cystic) structure in the mesentery of the distal ileum suspected to be a mesenteric lymphangioma of the distal ileum on the right side of the abdomen.
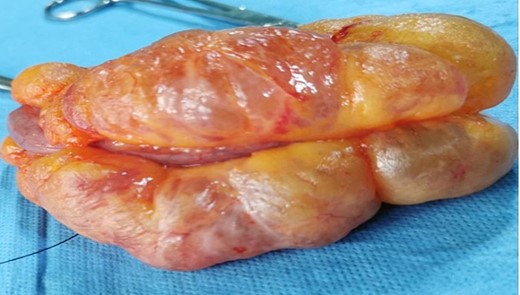
As the best therapeutic option, laparotomy and resection were performed. The lymphatic tissue-appearing cystic mass was immediately visible during surgery in the mesentery and antimesenteric border located in the distal ileum, ~12 cm in length (Fig. 2), and a vessel-sealing device separated the mass from its surroundings. The right ileocolic artery and vein were cleared of the lymphangioma, whereas the rest of the bowel and other organs were normal. Resection of the affected part of the small bowel and end-to-end anastomosis were performed (Fig. 3). The specimens were then sent for histopathological examination. The patient received Amoxicillin clavulanic acid (1 g every 8 h), Flagyl bottle (every 8 h for 3 days), ceftriaxone (1 mg every 12 h), paracetamol bottle (every 12 h for 3 days), and Lasix ampule (1 per day).
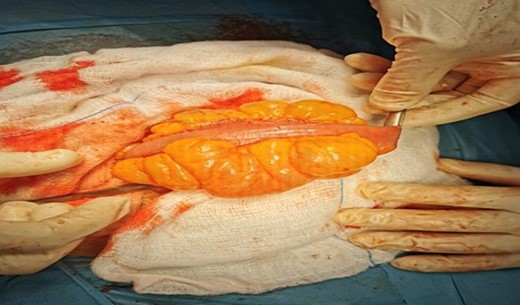
Intraoperative view of multiloculated cystic lesion found in the mesentery at the distal part of the ileum.
Microscopically, the section showed small bowel mucosa and submucosa with multiple small dilated vascular spaces lined by a single layer of benign-looking endothelial lining, with small foci of muscle bundles in the wall, and some lymphoid aggregates attached to them. Additionally, the same dilated lymphatic spaces were present in the fat and near the mesenteric lining of the bowel, suggesting intestinal lymphangioma, which is a rare benign vascular neoplasm of the small bowel (Fig. 4).
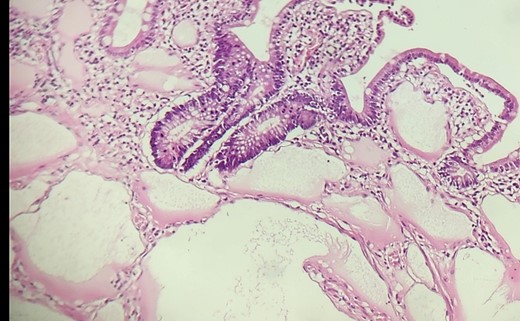
Histological results showed that small bowel mucosa and submucosa with multiple small dilated vascular spaces lined by endothelial lining.
A postoperative ileus that resolved within 3 days, and mild back and abdominal pain that was well-controlled with oral medication made up the majority of the postoperative recovery. The patient was discharged from the hospital after 4 days. Two weeks later, she was clinically healthy, with typical eating and bowel habits, and no complaints.
Discussion
Lymphangiomas are typically multilocular tumors of vascular and lymphatic origin and may contain serous, serosanguinous, or chylous fluid [8]. Approximately 70% of cases observed intraperitoneally are located in the mesentery of the small intestine. More than 80% of cases of mesenteric lymphangioma are discovered in children, and males are more commonly affected than females [9]. It is considered to be genetic and is caused by abnormal development of the embryonic lymphatic system, abdominal trauma, inflammatory processes, obstruction of the lymphatic system, surgery, and radiation therapy [5]. Furthermore, abdominal lymphangiomas in adult patients usually occur in middle-aged women and remain asymptomatic [10]. The present case involved a 49-year-old woman with mesenteric lymphangioma in the distal ileum. The patient presented with abdominal pain, distension, nausea, vomiting, acute bowel obstruction, or signs of peritonitis. If necessary, surgical distention with partial bowel resection should be performed [9]. In adult patients, like the present patient with abdominal pain, the diagnosis of intestinal lymphangioma can be challenging. Sonography is often the initial imaging modality of choice, revealing fluid-filled structures and associated findings, such as dilated loops of the small bowel or hydrosalpinx. The final diagnosis is usually made using MRI or CT scans, which can provide detailed information about the extent, location, and characteristics of the lesion [9, 11]. In this case, a combination of imaging and histopathological studies confirmed the diagnosis of the tumor.
Surgical resection when symptomatic is extremely rare, with most previously reported cases involving open laparotomy and only a few recent cases involving multiport laparoscopy [12]. When symptomatic lesions or complications occur, complete excision is the preferred approach to prevent recurrence and potential complications. In this case study, the mass was successfully resected, and the patient recovered well postoperatively [13].
Conclusion
Adults with intestinal lymphangiomas may present with nonspecific symptoms. Diagnosis is made based on clinical, radiologic, and histologic findings. Surgical resection is usually considered effective. Awareness of this uncommon condition aids in its diagnosis and treatment. Abdominal ultrasonography, CT, or MRI may be required if recurrence occurs.
Conflict of interest statement
None declared.
Funding
None declared.
Ethical approval
The authors confirm that this study was prepared according to the COPE rules and regulations. This study was approved by the ethical committee of the Baxshin Research Center (BRC 180723), dated 12 June 2023.
Consent
Informed consent was obtained from the patient before the preparation of the case report for publication (including clinical photographs), and the author/s endeavored to ensure anonymity.



