-
PDF
- Split View
-
Views
-
Cite
Cite
Christian I Gordon, Gabriel A Molina, Johann S Diaz, Maria B Mancero, Andrea E Heredia, Diana E Parrales, Jesus N Larco, An unusual case of gallstone ileus 35 years post-cholecystectomy masked by an incisional hernia, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae307, https://doi.org/10.1093/jscr/rjae307
Close - Share Icon Share
Abstract
Gallstone ileus is an uncommon cause of mechanical bowel obstruction in patients with cholecystitis and gallstones who develop a fistula over time. In the post-cholecystectomy patient, the presence of gallstone ileus is extremely rare; these patients have different pathophysiological pathways, such as a spilled gallstone that subsequently erodes into the bowel, subtotal cholecystectomies, and diverticulae that can hold a gallstone for hidden several years. In these patients, the clinical presentations are unique because of their rarity and because the gallbladder had been previously removed. A high index of suspicion by the medical team is needed for diagnosis. We present the case of an 85-year-old male who had a history of cholecystectomy 35 years ago. He presented to the emergency department with intestinal obstruction. Since he had a hernia, it was thought to be the cause of the obstruction; however, during surgery, we were surprised to find a gallstone ileus. After surgery, he fully recovered.
Introduction
Gallstone ileus is an infrequent disease associated with high mortality that is typically caused by the passage of a stone through a cholecystoenteric fistula, causing bowel obstruction [1, 2]. It’s even rarer for patients to have gallstone ileus years post-cholecystectomy [3, 4].
We present the case of an elderly patient who presented to the emergency department with intestinal obstruction. Since he had a hernia, it was thought to be the cause of the obstruction; however, during surgery, we were surprised to find a gallstone ileus.
Gallstone ileus 35 years post-cholecystectomy masked by an incisional hernia was the final diagnosis.
Case report
The patient is an 85-year-old male and has a history of hypertension, acute myocardial infarction, and cholecystectomy. The gallbladder was removed through an open approach with Kocher incision 35 years ago, and two years after that, he developed an incisional hernia at that site. He did not receive treatment for it, mainly due to the patient’s fear of surgery.
Suddenly, he presented with abdominal pain. At first, it was mild and was accompanied by nausea and vomits. After a few hours, the pain became severe. He did not pass any gas or stool, and his abdomen became distended. Due to this, he was brought to the emergency room by his family.
On clinical evaluation, a dehydrated patient was encountered. He was tachycardic but not hypotensive; on his abdomen, a 15 × 20 cm abdominal hernia was discovered; the hernia was irreducible, and he had pain on palpation with tenderness.
His bowel sounds were diminished, and his abdomen was distended. Due to this, complementary exams were needed, revealing leukocytosis (13.5 k/μl) with an elevated C-reactive protein (23 mg/dl). pH was 7.35 but had a mildly elevated lactate of 3.3 mmol/L.
With these results, an abdominal CT revealed diffuse bowel obstruction; most of the small bowel was dilated (measuring > 4 cm in diameter), and there were loops of the bowel within the hernia that were enlarged with multiple air-fluid levels. We didn’t detect any mass on the liver or complications with the previous cholecystectomy. Bowel obstruction due to an incarcerated hernia was suspected Fig. 1A–C. With this, surgical consultation was needed, and surgery was decided.
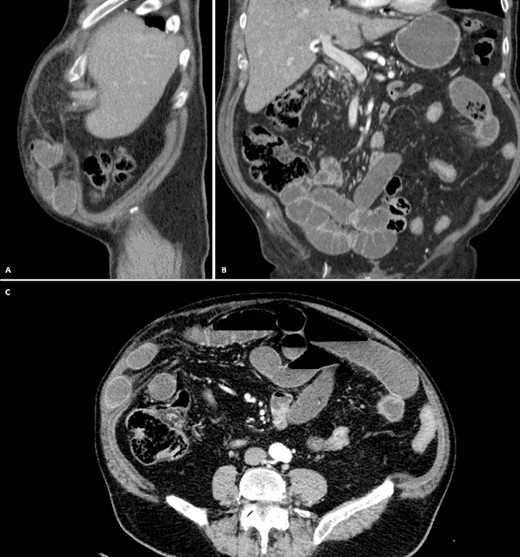
A: CT, Multiple dilated bowel loops within the hernia. B: CT, No Pneumobilia is seen. C: CT, Diffuse dilation with multiple air-fluid levels.
At laparotomy, the hernia sac was easily reduced, and the bowel within was released from few adhesions using an ultrasonic energy device (Harmonic, Ethicon, NJ). Nonetheless, there was no clear sign of obstruction at that place, so the whole small bowel was exposed. On the terminal ileum, 60 cm away from the ileocecal valve, a 30 cm segment of the bowel was enlarged, the bowel wall seemed fibrous, and its mesentery inflamed. Within its lumen, a 2.5 × 3 cm impacted stone-like structure was discovered; due to this, this segment of the bowel was resected entirely using mechanical staplers (Echelon, Ethicon, NJ), and the enterotomy was closed using a 2–0 monofilament suture in a two-layer fashion. Since there was no contamination on the abdomen, the abdominal wall defect was corrected with a collagen-coated mesh, and the procedure was completed without complication.
Pathology revealed gallstone ileus; there was one 3 × 2 × 1 cm gallstone impacted in the bowel wall, causing severe inflammation. There were also numerous inflammation folds with chronic inflammatory changes causing an area of stenosis that obstructed 40% of the bowel lumen. (Fig. 2).

Pathology, bowel segment occupied by fragments of mixed calculi of 3 × 2 x 1 cm, The gallstone was impacted in an area of stenosis that obstructs 40% of its lumen.
The patient’s postoperative course was unremarkable; liquids were initiated on postoperative day one, and he was discharged after a short course of antibiotics. On follow-ups, the patient is doing well; his hernia has resolved, and he has not encountered any issues.
Discussion
Gallstone ileus is a rare complication of cholelithiasis in which a gallstone migrates into the gastrointestinal tract (GI) through a fistula, causing mechanical intestinal obstruction [1]. Since Thomas Bartholin et al. first described this condition in 1654, gallstone ileus appears in up to 0.5% of patients with cholelithiasis, and it causes < 5% of all cases of abdominal obstruction [1, 2]. Gallstone ileus tends to occur in elderly and female patients because of the predominance of cholelithiasis in women [2]. This disease appears due to the constant inflammation and pressure effect of a gallstone towards the gallbladder wall [2]. This causes erosion, leading to fistula formation between the gallbladder and any adjacent portion of the GI, allowing the gallstone to pass [1, 3]. On rare occasions, the spillage of calculi after a cholecystectomy can cause the gallstone to lie free in the abdomen; while some may cause an intraabdominal abscess, others can ulcerate the intestinal wall and gain entrance to the bowel lumen [3, 4]. This fistula formation frequently occurs in the duodenum due to its proximity; however, any part of the GI can be affected [4]. Once the gallbladder is free, it usually contracts to a small fibrous remnant [1, 4].
When the gallstone is within the intestinal lumen, it usually proceeds distally and may pass spontaneously through the rectum completely asymptomatic, or it may become impacted and cause obstruction [5]. On rare occasions, the gallstone can also be vomited [1, 5]. The gallstone’s size, the fistula’s location, and the bowel lumen’s diameter will be vital in determining whether or not an obstruction occurs [1, 6]. Gallstones smaller than 2.5 cm may pass spontaneously [2, 4]. However, obstruction can appear in any part of the GI, more frequently if there are diverticula, neoplasms, or intestinal strictures, which may cause the gallstone to impact [2]. This impaction can cause inflammation, necrosis, and even perforation [1, 2]. Gallstone ileus in the absence of a gallbladder is extremely rare, with <20 cases described in the literature [7, 8]. In these patients, the presence of a gallstone within the bowel could be explained by subtotal cholecystectomies in which a gallstone was left behind, a gallstone that remained within the GI tract for years, and other even rarer explanations such as the formation of calculi inside the bowel in places where there is stasis or diverticulae [1, 7, 8] (diverticular disease, small bowel stricture, Crohn’s disease, or side-to-side anastomosis).
We believe that our patient must have had the gallstone inside his bowel since the time of his first surgery, which would explain the chronic inflammation and strictures he had on his bowel; another explanation would be that a gallstone that was inadvertently left free in the abdominal cavity during his cholecystectomy that ulcerated that part of the bowel and then became impacted. Diagnosis will be challenging since it can easily be missed, and the medical team will need a high index of clinical suspicion [1, 8]. The history and physical examination are non-specific and will resemble intestinal obstruction. Laboratory investigations will not be very helpful either [6, 7].
Radiological studies will be vital in establishing a diagnosis; Rigler’s triad, which is pathognomic, includes pneumobilia (if there is a fistula), an ectopic stone, and signs of bowel obstruction [8]. X-rays and CT will be diagnostic; however, CT is considered the gold standard as it can better identify these signs [1, 9]. Unfortunately, smaller and less calcified stones may still be missed by CT [9].
In our case, the diagnosis was complicated due to the patient’s hernia, which confused us and made us think that it was the cause of the obstruction. Although the CT did not show the typical triad, the hernia blinded us. Sometimes, diagnoses that seem easy are not what they seem. The treatment of this condition will be the same as other gallstone ileus and is the surgical removal of the gallstone causing the obstruction, with or without excision of the underlying biliary-enteric fistula, during the same procedure [1, 7, 8]. Open and laparoscopic approaches have been described and will depend on the medical condition of the patient and the availability of resources [8, 9].
Knowledge of other pathologies prevents these apparent common cases from overshadowing other diagnoses, preventing delayed diagnosis or even misdiagnosis and consequent adverse outcomes for our patients: ‘In a time of horses, don’t forget about the zebras.’
Conclusion
Although postcholecystectomy, gallstone ileus is extremely rare. All surgeons should be aware of its existence, especially in high-incidence areas such as ours; since diagnosis requires a very high index of suspicion, it can be easily missed, leading to severe complications. Also, in a unique way, this case proves that apparently easy diagnoses can hide many pathologies; it is our duty as surgeons to remember all details that could help improve the prognosis of our patients.
Conflict of interest statement
None declared.
Funding
None declared.



