-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Alyami, Ali Alothman, Faisal Balaraj, Mohanned Alomairi, Yahya Ghazwani, Nasser Albqami, Post-traumatic renal arteriovenous malformation failed endovascular embolization, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae302, https://doi.org/10.1093/jscr/rjae302
Close - Share Icon Share
Abstract
Renal arteriovenous malformations (AVMs) are abnormal connections between the renal arteries and venous system. Arteriovenous fistulas account for 70%–80% of renal arteriovenous abnormalities, often resulting from iatrogenic injuries. While most renal AVMs are asymptomatic, hematuria is a common symptom caused by AVM rupture into the renal calyces. Angiography is the gold standard for diagnosis, but noninvasive imaging techniques like ultrasound, computed tomography, or magnetic resonance imaging are commonly used for initial evaluation. Most renal AVMs are managed conservatively. Symptomatic patients typically undergo endovascular embolization, the preferred treatment, while surgery is reserved for unstable patients or those with complex vascular anatomy. We present a case of a 32-year-old man with renal AVMs following a motor vehicle accident. The patient initially received unsuccessful endovascular embolization but achieved successful treatment through open fistula ligation. This case highlights the challenges in managing renal AVMs and the importance of considering alternative interventions when initial treatments prove ineffective.
Introduction
Renal arteriovenous malformations (AVMs) are characterized by an abnormal vascular pathway between the renal arteries and the venous system [1]. They occur in <1% of the general population, with the highest incidence observed in patients aged 30–40 years [2–4]. Renal AVMs can be classified into two categories: congenital renal AVMs and acquired renal AVMs [5]. Acquired renal AVMs, also known as arteriovenous fistulas (AVFs), account for ~70%–80% of renal arteriovenous abnormalities [5]. They are often associated with iatrogenic injuries, such as surgical procedures, renal biopsies, penetrating or blunt traumas, and malignant renal tumors [5]. On the other hand, congenital renal AVMs can be further divided into cirsoid, angiomatous, and aneurysmal types [6]. Most cases of renal AVMs are asymptomatic, although hematuria, resulting from the rupture of AVMs into the renal calyces, is the most common presentation [7]. Patients may also experience flank pain due to blood clots obstructing the urinary system [7]. Other clinical manifestations, such as an abdominal mass, perinephric hematoma, high output heart failure, and unexplained hypertension, are also frequently associated with renal AVMs [8]. While angiography is considered the gold standard for diagnosing renal AVMs, noninvasive imaging techniques such as ultrasound (US), computed tomography scans (CT), or magnetic resonance imaging (MRI) are commonly used as initial diagnostic methods due to their quick and highly accurate nature [9]. The majority of renal AVMs are managed conservatively [5]. In symptomatic patients, endovascular therapy with embolization is the preferred treatment method, while surgical interventions are reserved for unstable patients or those with complex vascular anatomy [5]. In this report, we present a case of a 32-year-old man with renal AVMs following a motor vehicle accident. Despite failed endovascular embolization, the patient was ultimately successfully treated with open fistula ligation.
Case presentation
A 32-year-old male with no known chronic illnesses had a history of a motor vehicle accident five years ago, resulting in multiple bilateral rib fractures. An abdominal and pelvic CT scan conducted at the time did not reveal any other findings. The patient was admitted under the care of thoracic surgery for observation and pain management. After four years from the accident, the patient experienced intermittent right flank pain and made multiple visits to the emergency room. A CT scan of the kidneys, ureters, and bladder (CT KUB) was performed to rule out urolithiasis. The CT KUB showed multiple prominent structures with communication between the arterial and venous systems at the right renal hilum, suggestive of an intrarenal AVM with no apparent complications (Fig. 1). A CT run-off study confirmed the presence of an intrarenal AVM in the upper pole, measuring 2.9 cm (Fig. 2). The patient underwent angioembolization; however, multiple attempts at coil embolization failed due to the high risk of distal embolization. Subsequently, the patient underwent exploratory laparotomy for right AVF ligation. During the procedure, three AVF tracts were identified and ligated using clips. Prior to ligation, a thrill was palpable, but it was absent after the ligation. On the second postoperative day, a Doppler renal US was performed, which revealed patent right intrarenal arteries with normal resistive indices and normal peak systolic velocity in the right main renal arteries.
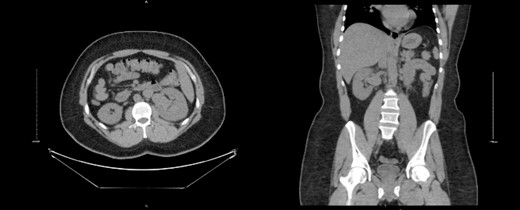
CT KUB showed multiple prominent structures with communication between the arterial and venous systems at the right renal hilum, suggestive of an intrarenal arteriovenous malformation (AVM).
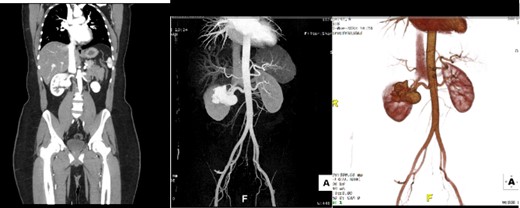
Run-off computed tomography angiography (CTA) showed right kidney hilum tortuous vascular arteriovenous communication of the arterial and venous system represents intrarenal AVM towards the upper pole measuring 2.9 cm.
Discussion
AVMs are characterized by abnormal communication between the renal arterial and venous systems [1]. The peak incidence of AVMs is observed in patients aged 30–40 years [2–4]. Typically, the malformation is located in the collecting system rather than the renal parenchyma, with the majority of cases occurring in the upper pole of the kidney (45%). However, it can also be found in the mid-point or lower pole of the kidney in equal proportions [2]. AVMs are more commonly seen in the left kidney, and women are affected twice as often as men [2–4]. Renal AVMs can be classified into two categories: congenital renal AVMs and acquired renal AVMs [5]. Acquired renal AVMs, also known as AVFs, account for ~70%–80% of renal arteriovenous abnormalities [3, 5]. They are frequently associated with iatrogenic injuries, such as surgery, renal biopsy, penetrating or blunt trauma, malignant renal tumors or inflammation [3, 5]. The diagnostic approach for renal AVMs depends on the patient’s clinical presentation [9, 10]. In patients presenting with flank pain and hematuria, the initial evaluation typically involves ruling out renal colic and urological malignancy. If there is suspicion of renal AVMs, targeted vascular imaging should be performed. The diagnosis and management of renal AVMs require a multidisciplinary approach involving urologists, radiologists, and interventional vascular radiologists. From the literature, we found a reported case of post-traumatic renal AVMs in Pakistan [9, 10]. We conducted a comparison between that case and our case based on factors such as age, presentation, diagnostic methods, treatment, and outcomes (Table 1). Historically, surgical interventions were used for the treatment of vascular abnormalities, but they have been largely replaced by endovascular embolization, which is less invasive, more effective, and associated with lower recurrence rates. Endovascular embolization also allows for the preservation of normal renal parenchyma [3, 10]. Surgical interventions, such as partial or complete nephrectomy and renal artery ligation, are less commonly employed due to the risks of graft or significant renal parenchymal loss [3]. Various embolic agents can be used for the treatment of renal AVMs, including polyvinyl alcohol particles, gelatin sponge particles, coils, vascular plugs, detachable balloons, absolute ethanol, N-butyl-2-cyanoacrylate, and ethylene vinyl alcohol copolymer [2, 10]. The choice of embolic materials depends on the type of renal AVM, as well as the size and flow characteristics of the lesion [2]. The risk of recanalization or incomplete occlusion after inadequate or incomplete embolization in transcatheter arterial embolization is influenced by the type of embolic material used and the size of the lesion [2].
| . | Age . | Presentation . | Type of Trauma . | Diagnostic Method . | Treatment . | Outcome . |
|---|---|---|---|---|---|---|
| Our | 32 | Flank pain | MVA | CT renal angiogram | Failed embolization 2 times Exploratory laparotomy and right AV fistula ligation | Uneventful |
| [9] | 20 | Flank pain and gross hematuria | Blunt abdominal trauma | CT renal angiogram | Angio-embolization | Uneventful |
| . | Age . | Presentation . | Type of Trauma . | Diagnostic Method . | Treatment . | Outcome . |
|---|---|---|---|---|---|---|
| Our | 32 | Flank pain | MVA | CT renal angiogram | Failed embolization 2 times Exploratory laparotomy and right AV fistula ligation | Uneventful |
| [9] | 20 | Flank pain and gross hematuria | Blunt abdominal trauma | CT renal angiogram | Angio-embolization | Uneventful |
| . | Age . | Presentation . | Type of Trauma . | Diagnostic Method . | Treatment . | Outcome . |
|---|---|---|---|---|---|---|
| Our | 32 | Flank pain | MVA | CT renal angiogram | Failed embolization 2 times Exploratory laparotomy and right AV fistula ligation | Uneventful |
| [9] | 20 | Flank pain and gross hematuria | Blunt abdominal trauma | CT renal angiogram | Angio-embolization | Uneventful |
| . | Age . | Presentation . | Type of Trauma . | Diagnostic Method . | Treatment . | Outcome . |
|---|---|---|---|---|---|---|
| Our | 32 | Flank pain | MVA | CT renal angiogram | Failed embolization 2 times Exploratory laparotomy and right AV fistula ligation | Uneventful |
| [9] | 20 | Flank pain and gross hematuria | Blunt abdominal trauma | CT renal angiogram | Angio-embolization | Uneventful |
Conclusion
Renal AVMs are uncommon conditions that often manifest with symptoms such as hematuria and back pain, which can be similar to urinary tract tumors or stones. The preferred initial diagnostic tests for renal AVMs are US or CT, and angiography should be performed to confirm the diagnosis. Treating post-traumatic renal AVMs can be challenging, and endovascular management is a safe option that allows for organ preservation. However, it is important to note that failure of endovascular embolization may occur. Therefore, regular long-term follow-up is recommended to monitor the patient for any signs of recurrence.
Conflict of interest statement
None declared.
Funding
None declared.
References
- angiogram
- congenital arteriovenous malformation
- magnetic resonance imaging
- arteriovenous fistula
- ultrasonography
- computed tomography
- renal artery
- patient evaluation
- pathologic fistula
- traffic accidents
- calyx
- ligation
- rupture
- surgical procedures, operative
- diagnosis
- diagnostic imaging
- kidney
- arteriography, renal
- renal arteriovenous malformation
- endovascular embolization
- iatrogenic injuries
- gold standard



