-
PDF
- Split View
-
Views
-
Cite
Cite
Elena Zafirovikj, Andrej Nikolovski, Nikola Nane, Blagica Krsteska, Perianal endometrioma presented as perianal abscess: report of two cases, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae270, https://doi.org/10.1093/jscr/rjae270
Close - Share Icon Share
Abstract
Perianal endometriosis is a rare clinical presentation of the extrauterine appearance of endometrium reported in <1% of the cases. The condition is accompanied by perianal cyclic pain and a palpable mass. If diagnosed by physical examination only, the condition may be easily misinterpreted as a perianal abscess and treated improperly with incision, thus resulting in “abscess recurrence.” Additional diagnostic imaging such as endoanal ultrasonography and magnetic resonance imaging should be mandatory to provide an accurate diagnosis and proper treatment resulting in low recurrence rates. We present two cases of perianal endometriomas initially diagnosed and treated as perianal abscesses.
Introduction
Endometriosis is a well-known condition of the extrauterine presence of endometrium associated with local cyclical pain [1]. When the uterine gland tissue becomes cystic and achieves an enviable dimension, the term “endometrioma” is used to define it [2]. The peritoneum is the most common site of endometriosis occurrence followed by the ovaries, deep pelvic space, abdominal viscera, diaphragm, abdominal wall, nervous system, and pleura [3]. Perianal endometriosis is very rare and accounts for 0.2% of the reported cases [1]. Its clinical presentation is often misinterpreted as a perianal abscess, and treated improperly with incisions. This series presents two patients with perianal endometriomas clinically manifested as perianal abscesses initially treated as such and followed with “recurrence.”
Case series
Case 1
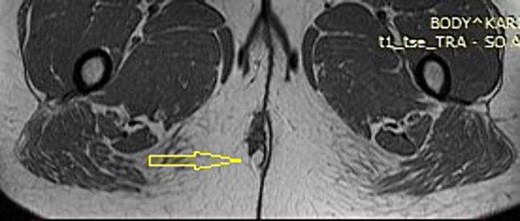
A 37-year-old female patient presented to the outpatient department with a palpable mass in the perianal region on the right side. The patient had two normal pregnancies with spontaneous deliveries 13 and 9 years ago, respectively. The medical history was remarkable for an operative treatment of perianal abscess 6 months before the examination. At the time of the surgery, the patient presented with pain and fluctuating swelling in the perianal region. An incision was performed with the evacuation of a small collection of dark fluid. After the procedure, a continuous experience with occasional pain and uncomfortable feeling in the perianal region was present. Magnetic resonance imaging (MRI) revealed a 4.5 × 2.5 cm perianal mass slightly towards the right side. It showed mixed intermediate and high signal intensity, attributed to the recurrent puss component. There was an associated diffusion restriction but no avid enhancement after intravenous contrast administration. The opacity of surrounding adipose tissue was noted. The nature of the mass was interpreted as recurrent abscess formation (Fig. 1).
A physical examination revealed a palpable perianal mass with a size of ~4 cm, slightly tender on palpation extending to the anal sphincter. A scar from a previous incision was noticed, but no fluctuation or suppuration was noted. The patient was scheduled for elective surgery performed under general anesthesia. The mass was excised and the defect was closed primarily. The patient was discharged the following day after surgery. The histology revealed ectopic endometrial tissue composed of endometrial gland and stroma between collagen bundles with areas of hemorrhage with some siderophages (Fig. 2A–C).
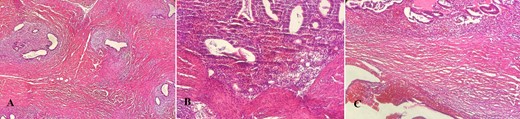
Histopathology report (hematoxylin–eosin stain). (A) Endometrial ectopic tissue. (B) Areas of hemorrhage in ectopic endometrial tissue. (C) Hemorrhage in endometrial tissue.
Case 2
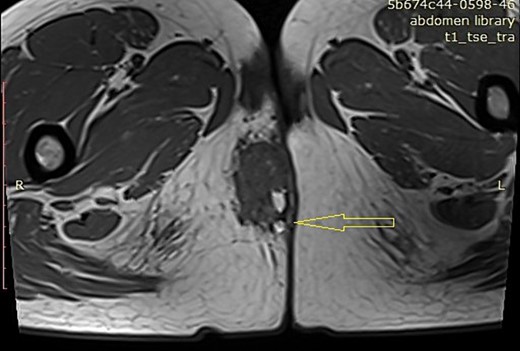
A 33-year-old female patient presented to the emergency department with pain and swelling in the perianal region. The patient was previously treated (a few months ago) for a perianal abscess. MRI revealed a 3.5 × 2 cm mass in the right perianal region pressing on and indenting the right aspect of the distal external sphincter. This mass showed mixed intermediate and high signal intensity. There was an associated diffusion restriction but no avid enhancement after intravenous contrast administration. No fatty components were observed. The exact nature of this mass was indeterminate. (Fig. 3). The patient had two spontaneous parturitions 6 and 3 years precedent, with a placenta defect noted on the second delivery that required manual revision of the uterine cavity.
A physical examination revealed a palpable tender perianal mass extending to the anal sphincter at the 11 o’clock position slightly fluctuating without skin redness.
The patient was counseled to undergo surgical excision of the mass under general anesthesia. Examination of the anal canal in a prone position showed no abnormalities. Attention was given to the perianal area, in which a cyst was found on the right side of the perianal region. An elliptical incision was made that was very close to the external anal sphincter with careful dissection. The mass was completely excised with an intact capsule with a <1 cm margin. (Fig. 4). Hospital discharge followed later the same day. The histology report confirmed perianal endometriosis presence.

Discussion
The first case of perineal endometriosis was published in 1923 by Schickete [4], followed by case reports and small case series publications [2, 5–8]. The etiology of this condition is explained by the endometriotic cells implantation in the perineum during vaginal delivery. Coelomic metaplasia and transplantation of the exfoliated endometrium is the second possible mechanism of perianal endometriosis event [1]. The reports of perianal endometriosis are various in terms of whether the perianal skin area (episiotomy scar) or the anal sphincter is involved [6–8]. In the cases where none of these “criteria” were “fulfilled,” the patients were initially misdiagnosed to have a perianal abscess and treated with repetitive incisions thus resulting in “abscess recurrence” [7, 9, 10]. In both of the cases in this report, the patients were also treated as having perianal abscesses resulting in unfavorable scenarios due to the improper diagnosis.
The conducted literature research with the use of the keywords “perianal,” “endometriosis,” “endometrioma,” and “abscess,” revealed eight cases initially treated as perianal abscesses (Table 1).
Literature review of known cases of perianal endometrioma presented as a perianal abscess.
| Reference number . | Author/Year . | Presentation . | Initial treatment (N) . | Definitive treatment . |
|---|---|---|---|---|
| [11] | Swerdlow/1975 | Perianal abscess | Perianal incision (2) | Abdominal HTA with BSO followed by local excision (3 months later) |
| [12] | Andreson, Tuckson/1988 | Supralevator abscess | Trans rectal incision (6) | Emergency laparotomy with HTA, BSO, colostomy, and appendectomy |
| [9] | Iqbal et al./2009 | Perianal abscess | Perianal incision (2) | Perianal excision |
| [10] | Rodrigues et al./2015 | Perianal abscess | Fistulotomy (1) | Episiotomy excision with enucleation |
| [3] | McComb et al./ 2023 | Perianal abscess | Perianal incision (1) | Incomplete excision + non-surgical management |
| [13] | Yogini et al./2019 | Perianal abscess | Perianal incision (1) | Perianal excision + GnRH analog |
| [14] | Liang et al./2021 | Perianal abscess | Perianal puncture and drainage (1) | Perianal excision |
| [15] | Andrei et al./2019 | Perianal abscess | Incision, evacuation of the abscess, fistulotomy (1) | The patient refused hormonal inhibitor treatment |
| This series | Zafirovikj et al./2024 | Perianal abscess (in both cases) | Incision in both cases (1 per each) | Perianal excision (in both cases) |
| Reference number . | Author/Year . | Presentation . | Initial treatment (N) . | Definitive treatment . |
|---|---|---|---|---|
| [11] | Swerdlow/1975 | Perianal abscess | Perianal incision (2) | Abdominal HTA with BSO followed by local excision (3 months later) |
| [12] | Andreson, Tuckson/1988 | Supralevator abscess | Trans rectal incision (6) | Emergency laparotomy with HTA, BSO, colostomy, and appendectomy |
| [9] | Iqbal et al./2009 | Perianal abscess | Perianal incision (2) | Perianal excision |
| [10] | Rodrigues et al./2015 | Perianal abscess | Fistulotomy (1) | Episiotomy excision with enucleation |
| [3] | McComb et al./ 2023 | Perianal abscess | Perianal incision (1) | Incomplete excision + non-surgical management |
| [13] | Yogini et al./2019 | Perianal abscess | Perianal incision (1) | Perianal excision + GnRH analog |
| [14] | Liang et al./2021 | Perianal abscess | Perianal puncture and drainage (1) | Perianal excision |
| [15] | Andrei et al./2019 | Perianal abscess | Incision, evacuation of the abscess, fistulotomy (1) | The patient refused hormonal inhibitor treatment |
| This series | Zafirovikj et al./2024 | Perianal abscess (in both cases) | Incision in both cases (1 per each) | Perianal excision (in both cases) |
HTA: hysterectomy; BSO: bilateral salpingo-oophorectomy; GnRH: gonadotropin-releasing Hormone.
Literature review of known cases of perianal endometrioma presented as a perianal abscess.
| Reference number . | Author/Year . | Presentation . | Initial treatment (N) . | Definitive treatment . |
|---|---|---|---|---|
| [11] | Swerdlow/1975 | Perianal abscess | Perianal incision (2) | Abdominal HTA with BSO followed by local excision (3 months later) |
| [12] | Andreson, Tuckson/1988 | Supralevator abscess | Trans rectal incision (6) | Emergency laparotomy with HTA, BSO, colostomy, and appendectomy |
| [9] | Iqbal et al./2009 | Perianal abscess | Perianal incision (2) | Perianal excision |
| [10] | Rodrigues et al./2015 | Perianal abscess | Fistulotomy (1) | Episiotomy excision with enucleation |
| [3] | McComb et al./ 2023 | Perianal abscess | Perianal incision (1) | Incomplete excision + non-surgical management |
| [13] | Yogini et al./2019 | Perianal abscess | Perianal incision (1) | Perianal excision + GnRH analog |
| [14] | Liang et al./2021 | Perianal abscess | Perianal puncture and drainage (1) | Perianal excision |
| [15] | Andrei et al./2019 | Perianal abscess | Incision, evacuation of the abscess, fistulotomy (1) | The patient refused hormonal inhibitor treatment |
| This series | Zafirovikj et al./2024 | Perianal abscess (in both cases) | Incision in both cases (1 per each) | Perianal excision (in both cases) |
| Reference number . | Author/Year . | Presentation . | Initial treatment (N) . | Definitive treatment . |
|---|---|---|---|---|
| [11] | Swerdlow/1975 | Perianal abscess | Perianal incision (2) | Abdominal HTA with BSO followed by local excision (3 months later) |
| [12] | Andreson, Tuckson/1988 | Supralevator abscess | Trans rectal incision (6) | Emergency laparotomy with HTA, BSO, colostomy, and appendectomy |
| [9] | Iqbal et al./2009 | Perianal abscess | Perianal incision (2) | Perianal excision |
| [10] | Rodrigues et al./2015 | Perianal abscess | Fistulotomy (1) | Episiotomy excision with enucleation |
| [3] | McComb et al./ 2023 | Perianal abscess | Perianal incision (1) | Incomplete excision + non-surgical management |
| [13] | Yogini et al./2019 | Perianal abscess | Perianal incision (1) | Perianal excision + GnRH analog |
| [14] | Liang et al./2021 | Perianal abscess | Perianal puncture and drainage (1) | Perianal excision |
| [15] | Andrei et al./2019 | Perianal abscess | Incision, evacuation of the abscess, fistulotomy (1) | The patient refused hormonal inhibitor treatment |
| This series | Zafirovikj et al./2024 | Perianal abscess (in both cases) | Incision in both cases (1 per each) | Perianal excision (in both cases) |
HTA: hysterectomy; BSO: bilateral salpingo-oophorectomy; GnRH: gonadotropin-releasing Hormone.
In the systematic review of Maillard et al. [16], in 92.9% of the cases of vulva–perineal endometriosis, some previous vulva–perineal lesion precluded the occurrence of the endometriosis and in only 4.3% it was spontaneous. Perianal endometriomas mostly present with perianal cyclical pain with redness and swelling, and palpable perianal mass (not always) which grows during the menstrual period [1, 3, 16]. A cyclic character of the pain is reported to be present in only 44% of the patients. In 41.1% of the patients, a growth of the nodule during menstruation was reported. Much less frequent symptoms (incidence below 6%) are pelvic pain, dyspareunia, dysmenorrhea, tenesmus, pruritus, and infertility. Other rare and non-characteristic symptoms that can occur are abdominal pain, dysuria, and changes in bowel habits [10].
Zhu et al. [17] proposed the use of a triad of symptoms which includes a history of past perianal injury (e.g. episiotomy) during vaginal delivery, palpable perianal mass or nodule, and progressive cyclical pain and swelling during the menstrual period.
The diagnosis of perianal endometriosis consists of thorough history taking, proper perianal examination, and the use of diagnostic tests and imaging. Measuring the level of serum cancer antigen 125 (CA 125) did not prove its diagnostic efficacy [16]. Endoanal ultrasonography (EUS) is one of the diagnostic tools reported to be effective in the diagnosis of perianal endometriosis thus excluding other perianal conditions (abscess, anal cancer) [7]. At the same time, it allows the assessment of anal sphincter involvement in the process of preoperative strategy making [6]. MRI with a sensitivity of 90–92% and specificity of 91–98% for perianal endometriosis is currently the diagnostic tool of choice. It has been recommended that both EUS and MRI should be performed in patients with suspicion of perianal endometrioma [16]. Biopsy of the lesion or fine needle aspiration can help in the final diagnosis establishment. However, due to the chronic painful nature of the lesion, a surgeon would prefer an excisional biopsy for the final diagnosis.
The treatment of perianal endometriosis consists of complete surgical excision of the lesion with or without hormonal suppression with gonadotropin-releasing hormone, oral contraceptives, and progestin [16]. In cases where the anal sphincter is involved, the partial excision of the muscle should be followed with an additional primary anal sphincter repair [8].
In the recent large study on perianal endometriosis by Zhou et al., it has been shown that multiple perianal lesions and anal sphincter involvement represent independent risk factors associated with recurrence. The recurrence rate was 15.4%. In 31.2% of them, repeated excision was performed. One patient ended with intravaginal radiotherapy due to no response to hormone therapy. The remaining patients (56.3%) were treated successfully with long-term medical treatment because they refused the offered additional surgery [18].
Perianal endometrioma can be easily misinterpreted as a perianal abscess in female patients within the reproductive age presented with localized pain. Its cyclic character should alert the clinician to conduct additional diagnostic imaging tests to avoid unnecessary perianal incisions and conduct a proper treatment.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
None declared.



