-
PDF
- Split View
-
Views
-
Cite
Cite
Eddy P Lincango, Luis F Serrano, Sebastian Vallejo, Paola Solis-Pazmino, Andrea Garcia-Bautista, William Acosta, Oscar J Ponce, Jorge Salazar-Vega, Cristhian Garcia, Diffuse large B-cell lymphoma associated with papillary thyroid carcinoma: a case report and systematic review on management and outcomes, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjad658, https://doi.org/10.1093/jscr/rjad658
Close - Share Icon Share
Abstract
Primary thyroid lymphoma is a rare thyroid cancer, comprising ˂5% of thyroid neoplasms. Most cases are diffuse large B-cell lymphoma (DLBCL). Coexistence with papillary thyroid cancer (PTC) is extremely rare. This study presents a case of a 55-year-old woman with DLBCL and micropapillary thyroid cancer who underwent lobectomy, chemotherapy, and radiotherapy. Additionally, we performed a systematic review of 10 cases, including the reported case. The risk of bias in case reports varied. DLBCL diagnoses were mainly made after surgery, with total thyroidectomy being the most common surgical procedure. Chemotherapy was administered in most cases, and radiotherapy was used in some cases. Long-term outcomes indicated a low recurrence rate. While some debate the role of surgery in thyroid lymphoma, this study suggests that surgery should be considered in selected cases. Further research is needed to determine optimal treatment strategies for DLBCL with PTC.
Introduction
Papillary thyroid cancer (PTC) is the most frequent thyroid neoplasm (90%). It tends to be slow growing and associated with a favorable prognosis [1]. On the other hand, primary thyroid lymphoma (PTL) is an unusual endocrine malignancy comprising ˂5% of thyroid neoplasms [2]. PTL usually presents with a rapidly enlarging painless thyroid mass that can cause obstructive symptoms like dyspnea, dysphagia, stridor, and hoarseness and most commonly affects women in the seventh decade [3]. Histologically, non-Hodgkin’s lymphoma represents 98% of all PTL and two-thirds of rare diffuse large B-cell lymphoma (DLBCL). A prompt cancer diagnosis is critical as early recognition greatly increases the probability of curative outcomes and is even more important in neoplasms. Some authors only recommend medical treatment for DLBCL, even in patients with severe airway compromise, due to the rapid effect of the treatment, and thus avoid the need for surgery [4–6]. However, other authors have suggested that surgical resection and chemotherapy combined with radiotherapy may improve the prognosis of these patients [3, 7–10].
The coexistence of these tumors (DLBCL with PTC) is extremely rare, with only a few cases reported [11–14]. Evidence-based guidance regarding the optimal management of such an association is scant in the literature and its outcomes. Herein we report a rare coexistence case of DLBCL with PTC and conduct a systematic review of cases of DLBCL with PTC to describe the results after these patients were intervened with thyroidectomy, chemotherapy, and radiotherapy.
Materials and methods
The narrative information of this clinical case was reported by using the CARE guideline checklist [15] and the systematic review by following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [16].
Eligibility criteria
For this systematic review, we included case reports and case series with the following criteria: (i) patients with a histologically confirmed diagnosis of diffuse large B-cell lymphoma and papillary thyroid carcinoma, (ii) any treatment used, and (iii) manuscripts written in English and Spanish. We excluded studies in which the diagnosis was lymphoid tissue associated with the mucosa because the management of these entities is different.
Data sources and searches
We applied a search strategy developed by an experienced librarian to find potentially eligible studies in Ovid MEDLINE(R), Epub Ahead of Print, In-Process & Other Non-Indexed Citations, and Daily, Ovid EMBASE, and Scopus from each database’s inception until 23 April 2020. Reference lists of selected studies and literature reviews were searched to identify missing articles.
Study selection
Search results were uploaded into a systematic review software program (DistillerSR, Ottawa, ON, Canada) [17]. Reviewers (E.L-N, P.S-P), working independently and in duplicate, screened abstracts and titles for eligibility using standardized instructions. Before initiating the abstract screening phase, a pilot was performed with ten articles to assess the clarity of the eligibility criteria among reviewers, and modifications were done accordingly. For abstract screening, articles included by at least one reviewer were considered for full-text screening. A pilot was performed with five articles before starting the full-text screening. At this stage, only articles included by both reviewers were deemed eligible for this systematic review, and in case of disagreements, these were resolved by consensus between the reviewers. Full-text screening agreement using Cohen’s kappa was substantial (k = 0.90) (Fig. 1).
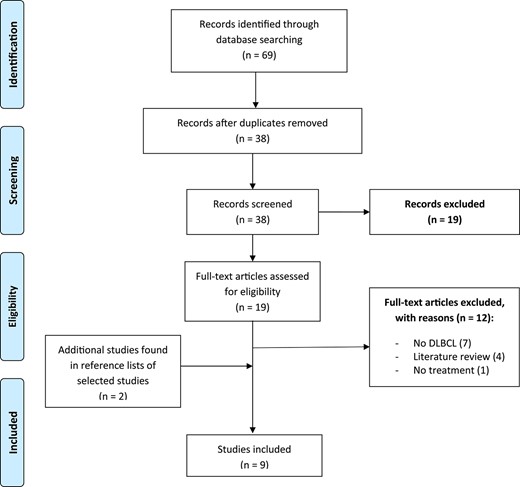
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram of the studies selection process.
Data collection and management
For all included articles, one reviewer (E.L-N) extracted study data into a spreadsheet sheet form, and a second reviewer (P.S-P) randomly checked 30% of the data extracted for accuracy and completeness. Variables extracted were: general characteristics of included studies (author, date of publication, country, study design), participant characteristics (age, sex, thyroid cancer histological type, Hashimoto thyroiditis, lymphoma preoperative diagnosis, Ann Arbor stage), management characteristics (type of surgery, type of chemotherapy, radiotherapy, radioiodine therapy), outcomes (the condition [recurrence or not] of the patient at last follow-up), and risk of bias indicators (Table 1).
| Author . | Country . | Age at presentation (years) . | Sex . | Clinical presentation . | Thyroid cancer type . | Hashimoto Thyroiditis . | DLBCL preoperative diagnosis . | Ann Arbor stage . | Treatment modalities . | Last follow-up outcome . | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | . | . | . | . | . | First used . | Second used . | Third used . | . |
| Lincango, 2020 | Ecuador | 56 | F | Rapidly growing neck lump causing dyspnea, dysphagia to liquids, cough and vomiting for 15 days | Micropapillary thyroid cancer | Yes | No | IE | Lobectomy + isthmectomy + tracheostomy | R-CHOP | Radiotherapy | 2 years: no recurrence or metastasis |
| Chen, 2019 [13] | China | 37 | F | Dyspnea and swallowing difficulties caused by a rapidly expanding mass in her neck over the previous 4 weeks | Papillary thyroid cancer | No | No | NR | Lobectomy | CHOP | .. | 1 year: no recurrence or metastasis |
| Kir, 2018 [14] | Turkey | 77 | F | Progressively enlarging thyroid gland for 24 months | Papillary thyroid cancer (1.3 × 1 cm) | No | Yes | NR | Total thyroidectomy | CHOPa | Radioiodine | 2 years: no recurrence or metastasis |
| Wu, 2016 [22] | China | 53 | F | Progressive enlargement of the neck mass | Papillary thyroid cancer | Yes | No | IE | Lobectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Trovato, 2015 [11] | Italy | 66 | F | Painless enlargement in the right anterior side of the neck, complaining of mild and intermittent dysphagia to solid and liquid foods. | Micropapillary thyroid cancer | Yes | No | NR | Total thyroidectomy | Chemotherapy | .. | 2 years: no recurrence or metastasis |
| Rella, 2015 [21] | Argentina | 70 | F | Dyspnea, dysphagia and stridor of a thyroid nodule | Two micropapillary thyroid cancers | Yes | No | NR | Thyroidectomy + tracheostomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Hosiriluck, 2014 [23] | NM | 79 | M | Enlarging neck mass | Papillary thyroid cancer | Yes | No | IIIE | Subtotal thyroidectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Xie, 2014 [12] | China | 41 | M | Thyroid enlargement for 2 months and a cervical mass for half a month | Papillary thyroid cancer | No | No | NR | Lobectomy + isthmectomy | CHOP | Radiotherapy | 2 months: no recurrence or metastasis |
| Cakir, 2013 [19] | Turkey | 50 | F | Dyspnea, difficulty swallowing, and a rapidly growing mass in the neck | Micropapillary thyroid cancer | NR | No | IE | Total thyroidectomy | .. | .. | 2 years: any problem |
| Anda-Gozalez, 2009 [20] | Mexico | 55 | F | Dysphagia to liquids, dyspnea, dysphonia for 4 months | Papillary thyroid cancer | Yes | No | NR | Thyroidectomy | Chemotherapy | .. | With recurrence and metastasis. Time no mentioned |
| Author . | Country . | Age at presentation (years) . | Sex . | Clinical presentation . | Thyroid cancer type . | Hashimoto Thyroiditis . | DLBCL preoperative diagnosis . | Ann Arbor stage . | Treatment modalities . | Last follow-up outcome . | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | . | . | . | . | . | First used . | Second used . | Third used . | . |
| Lincango, 2020 | Ecuador | 56 | F | Rapidly growing neck lump causing dyspnea, dysphagia to liquids, cough and vomiting for 15 days | Micropapillary thyroid cancer | Yes | No | IE | Lobectomy + isthmectomy + tracheostomy | R-CHOP | Radiotherapy | 2 years: no recurrence or metastasis |
| Chen, 2019 [13] | China | 37 | F | Dyspnea and swallowing difficulties caused by a rapidly expanding mass in her neck over the previous 4 weeks | Papillary thyroid cancer | No | No | NR | Lobectomy | CHOP | .. | 1 year: no recurrence or metastasis |
| Kir, 2018 [14] | Turkey | 77 | F | Progressively enlarging thyroid gland for 24 months | Papillary thyroid cancer (1.3 × 1 cm) | No | Yes | NR | Total thyroidectomy | CHOPa | Radioiodine | 2 years: no recurrence or metastasis |
| Wu, 2016 [22] | China | 53 | F | Progressive enlargement of the neck mass | Papillary thyroid cancer | Yes | No | IE | Lobectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Trovato, 2015 [11] | Italy | 66 | F | Painless enlargement in the right anterior side of the neck, complaining of mild and intermittent dysphagia to solid and liquid foods. | Micropapillary thyroid cancer | Yes | No | NR | Total thyroidectomy | Chemotherapy | .. | 2 years: no recurrence or metastasis |
| Rella, 2015 [21] | Argentina | 70 | F | Dyspnea, dysphagia and stridor of a thyroid nodule | Two micropapillary thyroid cancers | Yes | No | NR | Thyroidectomy + tracheostomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Hosiriluck, 2014 [23] | NM | 79 | M | Enlarging neck mass | Papillary thyroid cancer | Yes | No | IIIE | Subtotal thyroidectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Xie, 2014 [12] | China | 41 | M | Thyroid enlargement for 2 months and a cervical mass for half a month | Papillary thyroid cancer | No | No | NR | Lobectomy + isthmectomy | CHOP | Radiotherapy | 2 months: no recurrence or metastasis |
| Cakir, 2013 [19] | Turkey | 50 | F | Dyspnea, difficulty swallowing, and a rapidly growing mass in the neck | Micropapillary thyroid cancer | NR | No | IE | Total thyroidectomy | .. | .. | 2 years: any problem |
| Anda-Gozalez, 2009 [20] | Mexico | 55 | F | Dysphagia to liquids, dyspnea, dysphonia for 4 months | Papillary thyroid cancer | Yes | No | NR | Thyroidectomy | Chemotherapy | .. | With recurrence and metastasis. Time no mentioned |
DLBCL: diffuse large B cell lymphoma; R-CHOP: Rituximab, Cyclophosphamide, Doxorubicin, Vincristine, Prednisone; CHOP: Cyclophosphamide, Doxorubicin, Vincristine, Prednisone; F: female, M: male; NR: no reported.
aCyclophosphamide, Daunorubicin, Vincristine, Prednisone.
| Author . | Country . | Age at presentation (years) . | Sex . | Clinical presentation . | Thyroid cancer type . | Hashimoto Thyroiditis . | DLBCL preoperative diagnosis . | Ann Arbor stage . | Treatment modalities . | Last follow-up outcome . | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | . | . | . | . | . | First used . | Second used . | Third used . | . |
| Lincango, 2020 | Ecuador | 56 | F | Rapidly growing neck lump causing dyspnea, dysphagia to liquids, cough and vomiting for 15 days | Micropapillary thyroid cancer | Yes | No | IE | Lobectomy + isthmectomy + tracheostomy | R-CHOP | Radiotherapy | 2 years: no recurrence or metastasis |
| Chen, 2019 [13] | China | 37 | F | Dyspnea and swallowing difficulties caused by a rapidly expanding mass in her neck over the previous 4 weeks | Papillary thyroid cancer | No | No | NR | Lobectomy | CHOP | .. | 1 year: no recurrence or metastasis |
| Kir, 2018 [14] | Turkey | 77 | F | Progressively enlarging thyroid gland for 24 months | Papillary thyroid cancer (1.3 × 1 cm) | No | Yes | NR | Total thyroidectomy | CHOPa | Radioiodine | 2 years: no recurrence or metastasis |
| Wu, 2016 [22] | China | 53 | F | Progressive enlargement of the neck mass | Papillary thyroid cancer | Yes | No | IE | Lobectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Trovato, 2015 [11] | Italy | 66 | F | Painless enlargement in the right anterior side of the neck, complaining of mild and intermittent dysphagia to solid and liquid foods. | Micropapillary thyroid cancer | Yes | No | NR | Total thyroidectomy | Chemotherapy | .. | 2 years: no recurrence or metastasis |
| Rella, 2015 [21] | Argentina | 70 | F | Dyspnea, dysphagia and stridor of a thyroid nodule | Two micropapillary thyroid cancers | Yes | No | NR | Thyroidectomy + tracheostomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Hosiriluck, 2014 [23] | NM | 79 | M | Enlarging neck mass | Papillary thyroid cancer | Yes | No | IIIE | Subtotal thyroidectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Xie, 2014 [12] | China | 41 | M | Thyroid enlargement for 2 months and a cervical mass for half a month | Papillary thyroid cancer | No | No | NR | Lobectomy + isthmectomy | CHOP | Radiotherapy | 2 months: no recurrence or metastasis |
| Cakir, 2013 [19] | Turkey | 50 | F | Dyspnea, difficulty swallowing, and a rapidly growing mass in the neck | Micropapillary thyroid cancer | NR | No | IE | Total thyroidectomy | .. | .. | 2 years: any problem |
| Anda-Gozalez, 2009 [20] | Mexico | 55 | F | Dysphagia to liquids, dyspnea, dysphonia for 4 months | Papillary thyroid cancer | Yes | No | NR | Thyroidectomy | Chemotherapy | .. | With recurrence and metastasis. Time no mentioned |
| Author . | Country . | Age at presentation (years) . | Sex . | Clinical presentation . | Thyroid cancer type . | Hashimoto Thyroiditis . | DLBCL preoperative diagnosis . | Ann Arbor stage . | Treatment modalities . | Last follow-up outcome . | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | . | . | . | . | . | . | . | . | First used . | Second used . | Third used . | . |
| Lincango, 2020 | Ecuador | 56 | F | Rapidly growing neck lump causing dyspnea, dysphagia to liquids, cough and vomiting for 15 days | Micropapillary thyroid cancer | Yes | No | IE | Lobectomy + isthmectomy + tracheostomy | R-CHOP | Radiotherapy | 2 years: no recurrence or metastasis |
| Chen, 2019 [13] | China | 37 | F | Dyspnea and swallowing difficulties caused by a rapidly expanding mass in her neck over the previous 4 weeks | Papillary thyroid cancer | No | No | NR | Lobectomy | CHOP | .. | 1 year: no recurrence or metastasis |
| Kir, 2018 [14] | Turkey | 77 | F | Progressively enlarging thyroid gland for 24 months | Papillary thyroid cancer (1.3 × 1 cm) | No | Yes | NR | Total thyroidectomy | CHOPa | Radioiodine | 2 years: no recurrence or metastasis |
| Wu, 2016 [22] | China | 53 | F | Progressive enlargement of the neck mass | Papillary thyroid cancer | Yes | No | IE | Lobectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Trovato, 2015 [11] | Italy | 66 | F | Painless enlargement in the right anterior side of the neck, complaining of mild and intermittent dysphagia to solid and liquid foods. | Micropapillary thyroid cancer | Yes | No | NR | Total thyroidectomy | Chemotherapy | .. | 2 years: no recurrence or metastasis |
| Rella, 2015 [21] | Argentina | 70 | F | Dyspnea, dysphagia and stridor of a thyroid nodule | Two micropapillary thyroid cancers | Yes | No | NR | Thyroidectomy + tracheostomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Hosiriluck, 2014 [23] | NM | 79 | M | Enlarging neck mass | Papillary thyroid cancer | Yes | No | IIIE | Subtotal thyroidectomy | R-CHOP | .. | No recurrence and metastasis. Time no mentioned |
| Xie, 2014 [12] | China | 41 | M | Thyroid enlargement for 2 months and a cervical mass for half a month | Papillary thyroid cancer | No | No | NR | Lobectomy + isthmectomy | CHOP | Radiotherapy | 2 months: no recurrence or metastasis |
| Cakir, 2013 [19] | Turkey | 50 | F | Dyspnea, difficulty swallowing, and a rapidly growing mass in the neck | Micropapillary thyroid cancer | NR | No | IE | Total thyroidectomy | .. | .. | 2 years: any problem |
| Anda-Gozalez, 2009 [20] | Mexico | 55 | F | Dysphagia to liquids, dyspnea, dysphonia for 4 months | Papillary thyroid cancer | Yes | No | NR | Thyroidectomy | Chemotherapy | .. | With recurrence and metastasis. Time no mentioned |
DLBCL: diffuse large B cell lymphoma; R-CHOP: Rituximab, Cyclophosphamide, Doxorubicin, Vincristine, Prednisone; CHOP: Cyclophosphamide, Doxorubicin, Vincristine, Prednisone; F: female, M: male; NR: no reported.
aCyclophosphamide, Daunorubicin, Vincristine, Prednisone.
Risk of bias in individual studies
The study risk of bias was assessed by two independent reviewers based on Murad et al. tool [18] using eight questions assessing four domains: selection, ascertainment, causality, and reporting. Each question can have a yes or no answer. If the response to a question was yes, we summed 1 point. On the contrary, if the response was no, we rested 1 point. (E.L-N., P.S-P.). The studies that received a score of seven or more were judged to be at low risk of bias; studies that scored five or six were considered at unclear risk, and those that scored four or less were considered at high risk of bias. (Table S1, Supplementary material).
Results
Case report
A 55-year-old woman presented to the emergency department with symptoms of asthenia and a rapidly growing lump in her neck, persisting for 2 months in 2018. The neck lump was causing various issues like dyspnea, dysphagia, cough, and vomiting. Her medical history revealed a previous diagnosis of a benign thyroid nodule (3.4 cm) on the right upper thyroid lobe, without any cervical lymph node involvement, 7 weeks prior. The patient denied any history of cervical irradiation or a family history of thyroid cancer.
Upon physical examination, a hard, painless, and immobile mass measuring 10 × 10 cm was detected in the anterior neck. Neck tomography confirmed the presence of a thyroid mass originating from the right lobe, measuring 8.8 × 6.8 × 6.4 cm, with infiltration into the endoluminal trachea (Fig. 2a). Given the rapidly progressing obstructive symptoms, the suspicion was high for either anaplastic thyroid carcinoma or thyroid lymphoma. Before surgery, flexible bronchoscopy and laryngoscopy were conducted to assess vocal cords and airway involvement. These examinations revealed mobile vocal folds, blastic inflammation of the entire mucosa, and a hypervascularized exophytic lesion suggestive of invasion causing 70% obstruction between the first and second tracheal rings. The patient underwent immediate surgery aiming for total thyroidectomy and tangential tumor shaving for the tracheal invasion. However, debulking left lobectomy and left lateral tracheotomy at the fourth tracheal ring were performed as the surgeon deemed the remaining thyroid tissue unresectable due to tracheal invasion. The specimen and the right lobe biopsy were sent for histopathological examination, while the patient received methylprednisolone to reduce tumor size. Subsequently, she received prednisone until chemotherapy could be initiated.
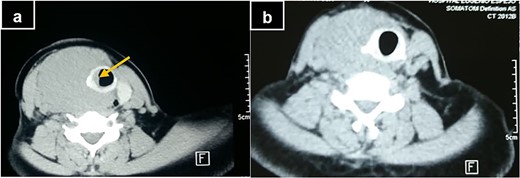
(a) Computerized tomography of the neck at diagnosis, showing tracheal invasion and deviation (yellow arrow). (b) Computerized tomography of the neck after the 4th R-CHOP cycle.
Histopathology results of the resected left lobe revealed a unifocal tall-cell variant micropapillary thyroid cancer measuring 0.4 cm without gross extrathyroidal extension (T1aN0M0). Additionally, evidence of Hashimoto’s thyroiditis and lymphocytic proliferation, suggestive of lymphoma, was observed but remained inconclusive for starting treatment (Fig. 3). Immunohistochemistry confirmed the diffuse large B-cell lymphoma diagnosis, with the specimen showing CD20 and BCL2 positivity and CD10 and CD30 negativity. Whole-body tomography was performed to determine the Ann Arbor lymphoma stage, which was classified as stage IE (localized involvement of a single extralymphatic organ in the absence of any lymph node involvement).
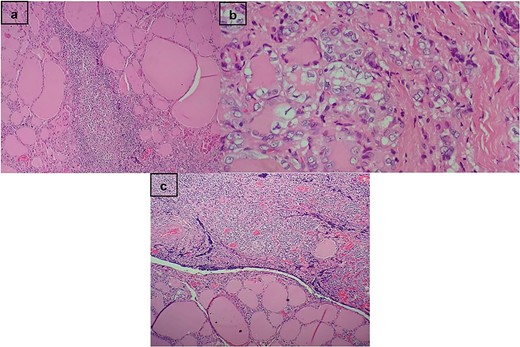
(a) Hashimoto’s thyroiditis. In the stroma, the presence of lymphoid follicles with germinal centers. (b) Follicular pattern papillary carcinoma. Empty nuclei, cleaved with bars and intranuclear inclusions. (c) Transition between the thyroid gland and dense proliferation of lymphocytes.
The patient subsequently received eight cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) chemotherapy, lasting roughly 6 moths, which yielded positive results and led to an improvement in tracheal invasion (Fig. 2b). A follow-up laryngoscopy showed left vocal cord paresis but no visible mass. Before initiating radiotherapy, the patient underwent a completion thyroidectomy due to the aggressive nature of the microcarcinoma. Decannulation was also planned. Right lobe measuring 2.3 × 3.3 × 3.2 cm was extracted. Recurrent laryngeal nerve was preserved. Subsequently, she received 20 sessions of consolidation radiotherapy on the neck with a dosage of 40 GY. Combined modality treatment with chemotherapy and radiotherapy is preferred for limited-stage DLBCL as it is associated with a higher 5-year failure-free survival rate. The patient experienced an episode of stomatitis following the radiotherapy, but it resolved with nystatin treatment. The patient remains healthy 4 years postoperatively without local recurrence or distant metastasis in repeat computer tomography (CT) scans.
Systematic review
Figure 1 describes the results of our search. Nine case reports were included [11–14, 19–23] reporting patients with diffuse large B cell lymphoma coexisting with papillary thyroid cancer. Overall, the risk of bias in case reports was unclear (3) [13, 14, 19] and high (6) [11, 12, 20–23] (Table S1). There were nine patients, reaching a total of 10 patients with our case. Age ranged from 37 to 79 years old, and most were female (80%) (Table 1).
The most common clinical presentation was dyspnea (50%) and dysphagia (50%) for a rapidly growing mass in the neck. In addition to lymphoma, 60% of patients had Hashimoto’s thyroiditis, and 40% had micropapillary thyroid cancer (Table 1).
Regarding the time of DLBCL diagnosis, it was detected after surgery in 90% of patients. DLBCL was suspected after core needle biopsy of the affected lobe in only one case. All patients underwent surgery, and the most common types of surgery were total thyroidectomy (30%), followed by lobectomy (20%). The surgeries were complemented with chemotherapy (90%), radiotherapy (20%,) and radioiodine therapy (10%). Regarding the time of treatment modalities, all patients underwent surgery followed by chemotherapy. Only four studies reported the Ann Arbor stage; 75% had stage IE.
Five studies reported long-term outcomes (>2 years). At the last follow-up, 90% of patients had no recurrence or metastasis (Table 1).
Discussion
Whereas PTC and PTL have well-studied distinct management approaches, combining these two tumors in a single case presents a management challenge. Based on our reported case and literature review, surgery combined with chemotherapy and radiotherapy may be practical. The prognosis does not seem to be worsened by the coexistence of the two diseases but is more likely affected by the one having a more advanced presentation stage [11, 12]. The therapeutic strategy chosen should mainly be based on the subtype and stage of PTL because it has a worse prognosis, even in the early stages [24].
However, the optimal therapeutic approach in DLBCL is controversial. Some authors recommend no surgery, even palliative surgery, for airway symptom control [4–6], but others suggest surgery as a part of the treatment [3, 7–10]. A study [6] showed that combining total thyroidectomy with adjuvant radiotherapy did not demonstrate increased survival compared to radiotherapy alone in stages IE or IIE. Moreover, Walsh et al. [4] reported that because of chemotherapy’s rapid effect in controlling obstructive symptoms, patients with severe airway compromise due to tracheal compression could be safely and successfully managed medically, avoiding the need for tracheostomy or thyroidectomy. On the other hand, Meyer-Rochow et al. [9] suggested that in patients with obstructive symptoms, radiotherapy and chemotherapy can exacerbate symptoms because of tissue edema, and therefore palliative surgery aimed at reducing this before adjuvant treatment should be considered. Likewise, Sippel et al. [10] showed that palliative resection before chemotherapy and radiotherapy has good results when performed by experts, with an improvement of obstructive symptoms in all of them. More recent publications showed that thyroid lobectomy and near-total/total thyroidectomy were associated with better prognosis in DLBCL patients [3, 8]. Under these circumstances, surgery should be performed by a specialized surgeon to reduce the associated morbidity. In this case report, the patient underwent left salvage lobectomy and left lateral tracheotomy as compressive symptoms interfered decisively with her quality of life.
When a lymphoma diagnosis is made after surgical removal of the thyroid (with preoperative misdiagnosis of benign disease or neoplasm), adjuvant chemotherapy and radiotherapy will be necessary in most cases to avoid the recurrence of the disease [25]. It is not questionable that this combined modality to treat limited-stage DLBCL is recommended [4, 26]. The r-CHOP scheme is commonly preferred [3].
No guidelines exist for the proper management of DLBCL cases complicated by a significant defect in the trachea. It is preferable to protect the airway instead of instituting immediate elaborate operative methods [10, 27]. We opted for expectant management after the debulking lobectomy and tracheostomy to secure airway patency. Finally, because our patient had micropapillary PTC, no radioiodine therapy was needed, as per the ATA and NCCN guidelines [28, 29].
Conclusions
Treatment must prioritize the tumor with the worst prognosis at diagnosis and may vary by histopathological subtype. Our patient with DLBCL and PTC responded well to debulking surgery followed by chemotherapy and radiotherapy, consistent with other cases in the literature. Experienced surgeons should keep the differential of lymphoma in rapidly enlarging thyroid mass on presentation.
Conflict of interest statement
None declared.
Funding
None declared.
Ethics approval and consent to participate
All data were collected from the patient’s medical records after obtaining written informed consent. All data were anonymized, and all identifiable information and biological samples were stored according to the local guidelines.
Data availability
To support reproducible research, we have made all our files available online, Figshare [30]. Supplementary material and extra information (tables, figures) are available on this site: https://figshare.com/s/95382af97b3b0b603a34.



