-
PDF
- Split View
-
Views
-
Cite
Cite
Gabriel A Molina, Carolina Ludeña, Alberto C Arcia, Diana E Parrales, Andrea E Heredia, Karen D Nuñez, Nicole Berenice Narvaez, When a gastrostomy tube goes missing, acute bowel obstruction due to a migrated Foley catheter, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae233, https://doi.org/10.1093/jscr/rjae233
Close - Share Icon Share
Abstract
A gastrostomy is a common procedure for patients with swallowing problems or inability to maintain regular oral nutrition. These gastrostomy tubes need special attention, as complications can occur if the tubes are left unattended. In rare scenarios, these tubes can migrate and cause severe life-threatening difficulties such as bowel obstruction and pancreatitis. We present the case of a 76-year-old quadriplegic woman who had a gastrostomy tube. Suddenly, the tube was missing, and after urgent medical care, the gastrostomy tube was found within her bowel. After successful surgery, she recovered from this incident.
Introduction
A feeding tube is a procedure that allows the medical team to provide nutrition, hydration, and medication to patients with dysphagia or those who need long-term enteral nutritional support [1]. Most of the complications associated with a gastrostomy tube are inconsequential, but few have the potential to cause significant morbidity if not recognized and treated correctly [1, 2]. We present the case of a 76-year-old quadriplegic woman who had a gastrostomy tube due to a spinal stroke. Suddenly, the tube went missing, and her nurse couldn’t find it. After careful evaluation, the gastrostomy tube was found within her bowel. After successful surgery, she recovered from this incident.
Case report
The patient is a 76-year-old woman with a past medical history of spinal cord stroke, which made her quadriplegic for 6 years. She had little interaction with the environment and was entirely dependent on her caregivers, as she was unable to swallow and had had multiple hospital admissions for aspiration pneumonia. As a result, a gastrostomy was performed at that time so that she could feed herself using a 24-fr Foley catheter. However, she had been doing poorly over the past three years; as the insurance stopped covering her expenses, she had to be admitted to a publicly funded care center. In that center, she did not receive personalized attention, they did not have any special diet designed for her, and overall, they did not have adequate medical staff, so she gradually lost weight, and her condition deteriorated. Twelve hours prior to admission, as the nurse was about to give her the diet through the gastrostomy tube, she found that the gastrostomy tube was missing, along with the gauze that covered the wound. The nurse looked everywhere, and since she couldn’t find anything, the patient was brought immediately to the emergency room.
On clinical examination, a severely malnourished patient was encountered. She had complete paralysis on her limbs and had severe muscle atrophy. She was conscious. However, she was not very responsive to questions during the examination, as she was severely depressed. Upon examining her abdomen, a 2 × 3 cm wound in her upper abdomen was found; the wound had visible gastric mucosa, but the gastrostomy tube was not found.
With these findings, an upper endoscopy revealed two gauzes in the antrum; however, the gastrostomy tube was nowhere to be found (Fig. 1). Due to this, an abdominal computed tomography was needed, revealing that within the small bowel, the 24-fr Foley catheter with the inflated balloon was found near the ileocecal valve (Fig. 2).

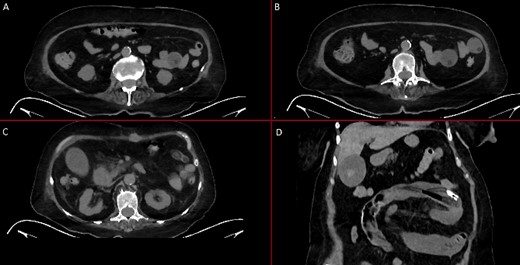
Abdominal CT. (A) An inflated balloon of the Foley catheter is seen in the bowel. (B) An inflated balloon of the Foley catheter is seen in the bowel causing obstruction. (C) The Foley catheter is seen inside bowel loops. (D) Foley catheter inside the bowel.
Surgical assessment was needed, and laparotomy was decided.
The Foley catheter was found 25 cm from the ileocecal valve within the small bowel. To remove it, a 1 cm enterotomy was done in the antimesenteric border to remove the catheter; then, the balloon was deflated, and the gastrostomy tube was removed entirely (Fig. 3). Afterward, attention was placed on the gastrocutaneous fistula. Using two green 60 mm Staplers (ETHICON - Johnson & Johnson®), the fistula was removed, and the staple line on the stomach was reinforced with a 2–0 polyproline suture in a one-layer fashion.

A feeding jejunostomy was done afterward, and the procedure was completed without complications. The patient fully recovered; a liquid diet was initiated through the jejunostomy on the first postoperative day, without complications. She was discharged to the same patient care center after no issues with the diet and a short course of antibiotics on her fifth postoperative day.
She was on regular follow-ups after this incident and doing well 3 months after surgery; nonetheless, she developed a respiratory infection that led to respiratory failure, septic shock, and, ultimately, death.
Discussion
Stroke is a significant cause of death and morbidity, not only because of its immediate effects but because after the initial injury, more than half of all survivors will become highly dependent on their caregivers [1]. The degree of disability after a stroke will depend on the location of ischemia and associated damage [1, 2]. Due to this, the patient’s disability will vary from the inability to eat and drink, problems with posture and mobility, communication difficulties, exhaustion, unhappiness, and depression, up to visual deficiencies [1, 3]. All of these complications will affect in some way the patient’s nutrition, especially those patients who will present with dysphagia after the stroke [2, 3]. Regretfully, up to 78% of patients with stroke will experience some way of dysphagia, and up to 15% of all stroke patients will have long-term issues associated with dysphagia, such as dehydration, malnutrition, and aspiration pneumonia [1, 3]. As our patient experienced.
When these events happen, a feeding tube will allow the medical team to provide nutrition and hydration and give the patients their essential medications [4]. When patients need long-term (4 weeks) feeding tube use, a gastrostomy or jejunostomy should be performed through laparoscopic or endoscopic approaches [1, 4]. Complications due to the use of a feeding tube include infection of the insertion site, leakage of gastric or intestinal fluid around the stoma, and ulceration of the mucosa [5]. Rare complications (<1%), such as peritonitis and perforation, have also been described [1, 5].
Gastrostomy tubes should be changed every 6 months [5, 6]. Nonetheless, if there is no availability, a Foley catheter can be used to maintain the patency of the gastrostomy tract and, at the same time, be used as a feeding tube [6]. Nonetheless, a Foley catheter is not a gastrostomy tube, and it can develop even rarer complications such as migration, intestinal obstruction, and even pancreatitis [6, 7]. These complications appear because these catheters do not have the external bumper to secure the tube to the abdominal skin, and they don’t have any marks that will help us measure the depth of the balloon [1, 2, 6]. Due to this, it’s recommended that Foley catheters only be used as temporary replacements when proper catheters are unavailable [7].
In resource-limited countries like ours, gastrostomy tubes are not widely available; although we know they’re not the best option, a Foley was used in our patient.
Migration is extremely rare and has been described in a few case reports in the English literature [7–9]. It is believed to happen due to the regular wear and tear caused to the external anchors, which makes them loose, allowing the catheter to migrate [8]. Therefore, regular check-ups and appropriate nurse training are needed to prevent this complication [9]. If migration happens, prompt medical attention is required as the tube can cause serious adverse events, such as gastric outlet obstruction, acute pancreatitis, obstructive jaundice, and small bowel obstruction with perforation [7, 8]. Endoscopic treatment should be performed if the catheter is still in the stomach; however, surgery will be needed if severe complications appear [10]. In our case, the nurse quickly detected the migration of the catheter, and the patient was brought immediately to the emergency room. Even though endoscopy was tried as a first step, surgery was ultimately needed.
It’s essential to be careful of these rare and life-threatening complications; patients with gastrostomy need our help more than others. They depend on us; we cannot let an element of care be something that potentially affects their life. This preventable complication proves we cannot tolerate poor management in the patient who needs us most.
Conclusion
Poverty and lack of resources should not affect healthcare. This subgroup of patients needs additional care to prevent this rare complication, especially when resources are limited. This case demonstrates the need for regular inspections and awareness for all caregivers of patients with feeding tubes, as this complication can be fatal.
Conflict of interest statement
None declared.
Funding
None declared.



