-
PDF
- Split View
-
Views
-
Cite
Cite
Pierre Guarino, Paolo Tesauro, Leone Giordano, Claudio Donadio Caporale, Livio Presutti, Francesco Mattioli, Surgical and radiological perspectives for the spinal accessory nerve passing through a fenestrated internal jugular vein: case series and literature review, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae099, https://doi.org/10.1093/jscr/rjae099
Close - Share Icon Share
Abstract
The preservation of the spinal accessory nerve represents a key goal in head and neck oncologic surgery during selective neck dissection. This study aims to illustrate the anatomical variants of the XI cranial nerve, delving into the relationship between the spinal nerve and the internal jugular vein, as well as the surgical implications. Two cases of patients who underwent oncologic surgery with neck dissection are described. Both cases found the spinal accessory nerve passing through the fenestration of the internal jugular vein. Alongside this case series, an independent literature review was conducted using the Medline and PubMed databases. In the majority of cases (67% – 96%), the spinal accessory nerve traces a lateral course to the internal jugular vein. Less frequently, the XI cranial nerve courses medial to the internal jugular vein. More rarely, as described in this case series, the nerve crosses through the fenestration of the vein (0.48% – 3.3%).
Introduction
During neck dissection, the spinal accessory nerve (SAN) is encountered on Level II at the level of the posterior belly of the digastric muscle where it crosses laterally and anterior the internal jugular vein (IJV). A medial course of the nerve is reported in literature with an incidence that varies from work to work. Rarely, the SAN can pass through a fenestration of the IJV or can split around the IJV [1, 2]. Nowadays, preservation of the SAN is the standard of care even though iatrogenic injury to the SAN and to the IJV still occurs. In order to reduce the risk of iatrogenic injury a detailed study of the radiological anatomy together with an extensive knowledge of the anatomical variants of the SAN and of the IJV represent the surgeon’s most important tools [3–6].
Case series
Patient 1
A 78-year-old man with a follow-up PET for a Type B mantle cell lymphoma finding of uptake in in the epiglottis and left laterocervical region is reported here. The patient was diagnosed with squamous cell carcinoma (SCC) after fine needle aspiration of an adenopathy at Level II. His workup included an MRI of the neck with contrast enhancement, which revealed laterocervical lymphadenopathy (bilateral level IIa and left Level III with the biggest adenopathy with maximum diameter of 12 × 12 mm) and thickening of the epiglottis extended at the floor of the left vallecula. No mention was made of an IJV abnormality in the report even though it was noticed during the preoperative evaluation by the surgeon (Fig. 1). The fibroendoscopic evaluation of the neck showed an asymmetry of the epiglottis with the presence of vegetating tissue at the level of the left lingual border of the epiglottis, preserved motility of the vocal cords, and normal breathing space. The patient’s clinical stadiation was cT2 N2c M0. The multidisciplinary meeting indicated an endoscopic partial laryngectomy and bilateral laterocervical dissection. The cervical lymph node dissection on the left side discovered a duplication of the IJV which resulted dilated in comparison to the IJV on the right side. The SAN passed medially to the anterior vein and laterally to the posterior vein. Both the IJV and the SAN were preserved during the procedure (Fig. 2).
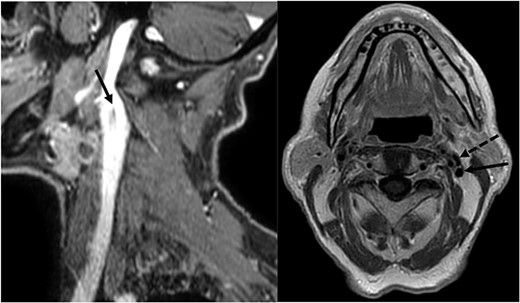
MRI showing the fenestration of the IJV; left image: sagittal section showing the fenestration (arrowhead) of the left IJV; right image: axial section showing the anterior (dotted arrowhead) and the posterior (arrowhead) part of the fenestrated IJV.
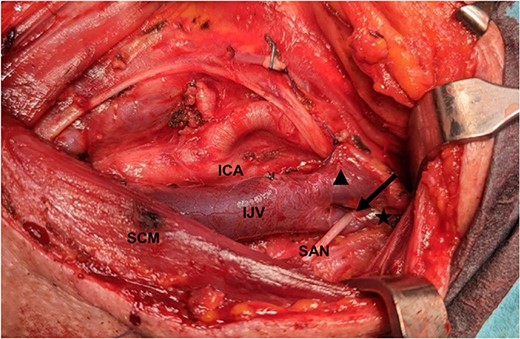
SAN passes through medially to the anterior part (filled triangle) and laterally to the posterior part (star) of the fenestrated IJV (arrowhead); ICA: internal carotid artery; SCM: sternocleidomastoid muscle.
Patient 2
A 72-year-old woman underwent total laryngectomy + thyroid isthmectomy + bilateral (II–IV) laterocervical dissection for a G3 SCC of the right hemilarynx (involving the right true and false vocal cord and extending to the anterior commissure and left vocal cord). The preoperative radiology report did not mention any IJV variations. Nonetheless, a left IJV fenestration was observed in the preoperative study, raising the suspect of a possible SAN variant (Fig. 3). Pathological stadiation of the patient was pT4a (infiltration of thyroid cartilage and prethyroid soft tissue) pN2c, cM0. Intraoperatively, the fenestration of the left IJV, that was noticed during the CT, was confirmed. As for the first patient presented, the SAN nerve passed medially to the anterior vein and laterally to the posterior vein (Fig. 4).
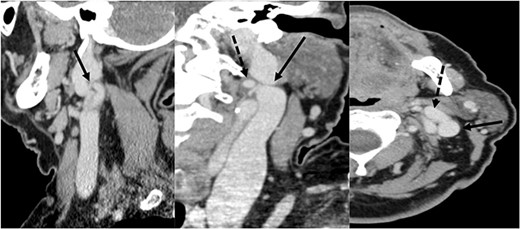
CT scan showing the fenestration of the IJV; left image: sagittal section showing the fenestration (arrowhead) of the left IJV; central image: coronal section showing the anterior (dotted arrowhead) and the posterior (arrowhead) part of the fenestrated IJV; right image: axial section showing the anterior (dotted arrowhead) and the posterior (arrowhead) part of the fenestrated IJV.
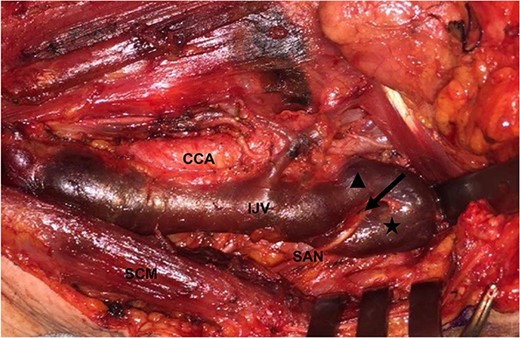
SAN passes through medially to the anterior part (filled triangle) and laterally to the posterior part (star) of the fenestrated IJV (arrowhead); CCA: common carotid artery.
Discussion
An in-depth understanding of the anatomy of the lateral neck is essential to avoid injury to the IJV during SAN dissection. A literature review of the anatomic relationship of the SAN to the IJV is presented in Table 1.
| Author . | Published . | Cadaveric (C)—in vivo (V) . | Neck dissection . | Lateral crossing . | Medial crossing . | Through IJV . | Around IJV . |
|---|---|---|---|---|---|---|---|
| Soo | 1986 | C | 23 | 56.0% | 44.0% | — | — |
| Krause | 1991 | C | 94 | 72.5% | 26.4% | 1.1% | — |
| Kierner | 2000 | C | 92 | 56.0% | 44.0% | — | — |
| Saman | 2011 | C | 84 | 79.8% | 19.0% | 1.2% | — |
| Lee | 2009 | V | 181 | 39.8% | 57.4% | 2.8% | — |
| Hashimoto | 2011 | V | 192 | — | — | 2.1% | — |
| Contrera | 2016 | V | 295 | — | — | 1.0% | — |
| Taylor | 2013 | V | 207 | 95.7% | 2.8% | 0.9% | 0.48% |
| Hinsley | 2010 | V | 116 | 96.6% | 2.6% | 0.8% | — |
| Prades | 2002 | V | 1000 | — | 0.4% | — | — |
| Levy | 2001 | V | 128* | 99.25% | 0.75% | — | — |
| Author . | Published . | Cadaveric (C)—in vivo (V) . | Neck dissection . | Lateral crossing . | Medial crossing . | Through IJV . | Around IJV . |
|---|---|---|---|---|---|---|---|
| Soo | 1986 | C | 23 | 56.0% | 44.0% | — | — |
| Krause | 1991 | C | 94 | 72.5% | 26.4% | 1.1% | — |
| Kierner | 2000 | C | 92 | 56.0% | 44.0% | — | — |
| Saman | 2011 | C | 84 | 79.8% | 19.0% | 1.2% | — |
| Lee | 2009 | V | 181 | 39.8% | 57.4% | 2.8% | — |
| Hashimoto | 2011 | V | 192 | — | — | 2.1% | — |
| Contrera | 2016 | V | 295 | — | — | 1.0% | — |
| Taylor | 2013 | V | 207 | 95.7% | 2.8% | 0.9% | 0.48% |
| Hinsley | 2010 | V | 116 | 96.6% | 2.6% | 0.8% | — |
| Prades | 2002 | V | 1000 | — | 0.4% | — | — |
| Levy | 2001 | V | 128* | 99.25% | 0.75% | — | — |
| Author . | Published . | Cadaveric (C)—in vivo (V) . | Neck dissection . | Lateral crossing . | Medial crossing . | Through IJV . | Around IJV . |
|---|---|---|---|---|---|---|---|
| Soo | 1986 | C | 23 | 56.0% | 44.0% | — | — |
| Krause | 1991 | C | 94 | 72.5% | 26.4% | 1.1% | — |
| Kierner | 2000 | C | 92 | 56.0% | 44.0% | — | — |
| Saman | 2011 | C | 84 | 79.8% | 19.0% | 1.2% | — |
| Lee | 2009 | V | 181 | 39.8% | 57.4% | 2.8% | — |
| Hashimoto | 2011 | V | 192 | — | — | 2.1% | — |
| Contrera | 2016 | V | 295 | — | — | 1.0% | — |
| Taylor | 2013 | V | 207 | 95.7% | 2.8% | 0.9% | 0.48% |
| Hinsley | 2010 | V | 116 | 96.6% | 2.6% | 0.8% | — |
| Prades | 2002 | V | 1000 | — | 0.4% | — | — |
| Levy | 2001 | V | 128* | 99.25% | 0.75% | — | — |
| Author . | Published . | Cadaveric (C)—in vivo (V) . | Neck dissection . | Lateral crossing . | Medial crossing . | Through IJV . | Around IJV . |
|---|---|---|---|---|---|---|---|
| Soo | 1986 | C | 23 | 56.0% | 44.0% | — | — |
| Krause | 1991 | C | 94 | 72.5% | 26.4% | 1.1% | — |
| Kierner | 2000 | C | 92 | 56.0% | 44.0% | — | — |
| Saman | 2011 | C | 84 | 79.8% | 19.0% | 1.2% | — |
| Lee | 2009 | V | 181 | 39.8% | 57.4% | 2.8% | — |
| Hashimoto | 2011 | V | 192 | — | — | 2.1% | — |
| Contrera | 2016 | V | 295 | — | — | 1.0% | — |
| Taylor | 2013 | V | 207 | 95.7% | 2.8% | 0.9% | 0.48% |
| Hinsley | 2010 | V | 116 | 96.6% | 2.6% | 0.8% | — |
| Prades | 2002 | V | 1000 | — | 0.4% | — | — |
| Levy | 2001 | V | 128* | 99.25% | 0.75% | — | — |
As shown, Krause, Soo, and Kierner conducted cadaveric studies [7–9]. Soo and Kierner reported an equal frequency of the lateral (56%) and medial (44%) position of the nerve compared to the IJV, while Krause reported an incidence of 72.5% of the nerve crossing lateral to the IJV. Krause also observed one case of SAN “fenestrating” through the IJV. Saman’s cadaveric study supported Krause’s data, reporting a 79.8% of SAN coursing lateral to the IJV, 19% of SAN medial to the IJV, and 1.2% of SAN “fenestrating” through the IJV [10].
In vivo studies reported a higher frequencies of the nerve crossing lateral to the IJV. Levy et al. [11], Hinsley et al. [12] and Taylor et al. [13] showed the SAN lateral to the IJV in 99.25%, 96.6%, 95.7% and the SAN medial to the IJV in 0.75%, 2.6% and 2.8%. Taylor and Hinsley also reported <1% of cases of SAN “fenestrating” to the IJV; moreover, Taylor described a new anatomical variant of the SAN in which the nerve divides and travels both medial and lateral to the IJV.
The higher incidence of the nerve crossing lateral to the IJV in in vivo studies compared to cadaveric is explained by Hinsley and Taylor as follows. The IJV of cadavers can collapse, determining a higher incidence of the medial position of the nerve in relation to the IJV. Moreover, in vivo studies which are conducted on oncological patients focus on the relation between the nerve and IJV at the level of the posterior belly of the digastric muscle, while cadaveric studies do not always keep the same reference points.
In 2009, Lee published an in vivo study in which he found a surprising 57.4% incidence of SAN medial to the IJV. However, these results have not been confirmed by other studies [14].
In his in vivo study, Lee pointed out that the variation of the course of the SAN correlates with a variation in the number of lymph node of the Levels IIa and IIb. Therefore, a lateral course of the SAN increases the Level IIb area, and subsequently, the number of lymph nodes.
Regarding the rarer anatomic variants of the SAN, Table 1 shows an incidence of the SAN “fenestrating” the IJV ranging from 0.8% to 2.2% [15–17]. Taylor also describes a new anatomical variant of the spinal nerve splitting around the IJV. However, there are no other reports of this variant of the SAN and no iconographic material results available.
So what tools can a surgeon use to uncover a rare anatomical variant of the SAN? In 2012, Hashimoto published a case report where they were able to identify the fenestration of the IJV with a contrast-enhanced CT. However, Ozturk warns us that even though the fenestration of the IJV is strongly associated with the SAN traveling through the fenestration, this is not to be taken for granted as it can also travel medial or lateral to the fenestration [18].
In both cases presented in this article, the surgeon noticed the fenestration of the IJV during the preoperative imaging which was not indicated in the radiologist report. As the radiologist priority concerns the extension of the tumor and lymph nodal spread, it falls to the surgeon to enquire about potential anatomical variants of the IJV during the scan.
Conclusion
The literature review conducted in this study confirms that the SAN crosses lateral to the IJV in the majority of cases. However, incidental finding of variants of the SAN, as presented in the case reports, can occur intraoperatively, resulting in iatrogenic lesion of the SAN or of the IJV. Therefore, an upfront radiological study together with a deep knowledge of the possible variants of the SAN are the surgeon’s keystones to reduce the cases of damage to the SAN or to the IJV. The authors also hope that this study could be a starting point for further investigations about the relationship between radiological and surgical anatomy.
Author contributions
All authors conceptualized the study. P.T. wrote the manuscript and prepared the original draft. PG reviewed and edited the manuscript. F.M., L.G., C.D.C., and L.P. supervised the study. P.T., P.G., and L.G. confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Conflict of interest statement
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
All data generated or analyzed during this study are included in this published article.
Consent to publish
The patients have provided written informed consent for the publication of any associated data and accompanying images.



