-
PDF
- Split View
-
Views
-
Cite
Cite
Yeon Soo Kim, Uniportal video-assisted thoracoscopic surgery in the prone position for esophageal bronchogenic cyst, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae186, https://doi.org/10.1093/jscr/rjae186
Close - Share Icon Share
Abstract
Esophageal bronchogenic cysts are very rare. A bronchogenic cyst is a congenital malformation resulting from abnormal sprouting of primitive bronchi because of a foregut bronchopulmonary malformation. An 18-year-old patient with a cystic tumor in the left posterior mediastinum was identified. The mediastinal tumor was removed by uniportal video-assisted thoracoscopic surgery. The operation was performed in the prone position through a single 4-cm incision on the lateral scapular line in the left ninth intercostal space. After tumor resection, the dissected esophageal muscle and mediastinal pleura were sutured with two continuous barbed sutures. The operation took 80 min. A biopsy confirmed the diagnosis of esophageal bronchial cyst. Diet was started on the evening of the operation. The chest tube was removed on the 1st postoperative day, and the patient was discharged without any problems on the 2nd postoperative day.
Introduction
Bronchogenic cysts are congenital anomalies that result from abnormal budding of the primitive tracheobronchial tube because of a bronchopulmonary malformation of the foregut. They are located most commonly in the middle and upper mediastinum [1]. Benign cysts are rare in the esophagus, accounting for only about 20% of benign esophageal tumors [2]. Esophageal bronchogenic cysts are a very rare condition. Although there is no consensus on the treatment of bronchial cysts, most surgeons prefer early removal, as they carry a risk of complications, including worsening or malignant transformation, and can put pressure on surrounding organs [3]. Thoracoscopic resection of benign esophageal tumors is a safe and feasible procedure. This is a case of successful removal of an esophageal bronchogenic cyst by single-incision thoracoscopic surgery in the prone position.
Case report
An 18-year-old male patient presented to the emergency department with right-side chest pain of 1-day duration. A plain chest x-ray confirmed a right pneumothorax. A tumor in the left lower paravertebral area was suspected (Fig. 1a). A CT of the chest was performed and showed a 6-cm large, well-defined, probable cystic mass in the left posterior mediastinum, adjacent to the esophagus. Esophageal duplication or bronchogenic or neurenteric cyst was suspected (Fig. 1b and c). The patient was discharged after pneumothorax had improved. Two months later, he was readmitted for surgery to remove the cystic tumor. Single-incision video-assisted thoracoscopic surgery (VATS) was performed to treat the posterior mediastinal tumor. The patient was placed in the prone position. An incision of 4 cm in length was made in the left ninth intercostal space at the lateral line of the scapula. A 5-mm thoracoscope with a 30-degree view was used. A cyst was identified in the posterior mediastinum (Fig. 2a), and a longitudinal incision was made in the mediastinal pleura. The left vagus nerve was placed beside the tumor. The lower half of the cystic mass was embedded in the muscular layer of the esophagus (Fig. 2b) and was in contact with the esophageal mucosa. The cyst was dissected carefully from the surrounding tissue. During dissection, the cyst ruptured, discharging an ivory mucoid creamy fluid. The cyst was completely removed with no injury to the esophageal mucosa. The esophageal mucosa, which was in close contact with the cyst, was stretched and protruding. To cover the exposed esophageal mucosa, the dissected esophageal muscle and periesophageal tissue were approximated with a continuous suture using a barbed suture (V-Loc™ 90, Medtronic) (Fig. 2c). Another barbed suture was used to repair the mediastinal pleura. A 24-Fr chest drain tube was placed through the same port (Fig. 2d). The operation took 80 min. The patient’s diet was started on the evening of the surgery. The chest drain was removed on the 1st postoperative day, and the patient was discharged from the hospital on the 2nd postoperative day without problems. Histopathological examination revealed a bronchogenic cyst. A CT scan of the chest carried out 2 years 7 months after the operation and confirmed that the patient had healed without any complications (Fig. 3).
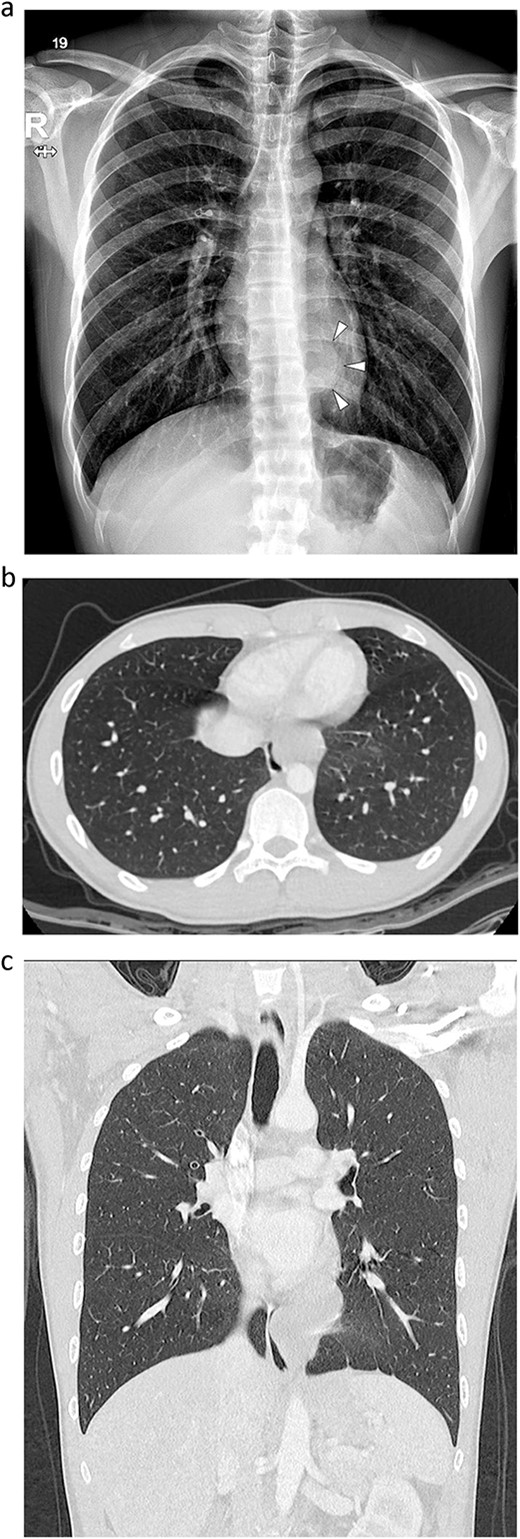
Radiographs of an 18-year-old man. (a) Simple radiograph shows a tumor in the left lower paravertebral area (arrow head). (b, c) A contrast-enhanced computed tomography scan. A 60 × 36 mm well-defined lobulated cystic mass in the left posterior mediastinum, abutting the esophagus.
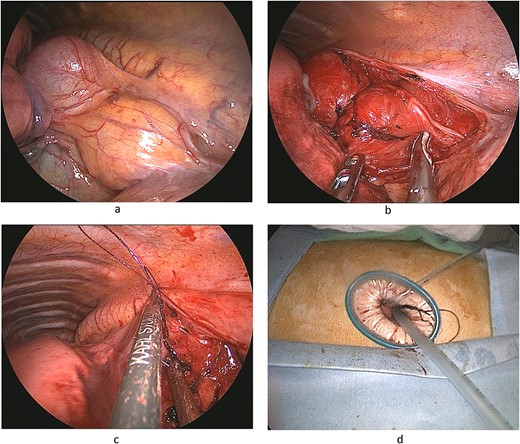
Operative findings. (a) Cystic tumor covered by mediastinal pleura located posterior mediastinum. (b) Distal half of the tumor was buried in muscular layer of esophagus. Left vagus nerve was placed beside the lower part of the tumor. (c) Continuous suturing of the esophageal muscular layer and periesophageal tissue using a barbed suture (V-Loc™ 90, Medtronic). (d) A 24 Fr drainage tube is inserted through 4-cm single port.
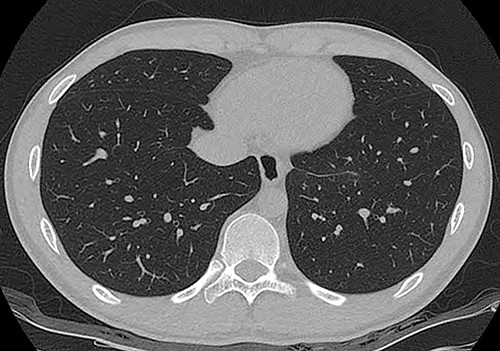
A computed tomography scan at 2 years 7 months after surgery. There was no evidence of tumor recurrence.
Discussion
A bronchogenic cyst is a congenital anomaly. The primitive foregut is divided into two parts at the 5th week of embryonic development, the tracheal bus in the ventral part and the esophagus in the dorsal part. A bronchogenic cyst forms because of abnormal germination and abnormal division of the primitive foregut [3].
Most surgeons agree on early surgical treatment because the risk of surgery increases with time, and complete removal becomes more difficult if complications occur [3, 4]. Jung et al. [3] stated that minimally invasive surgery using thoracoscopy is safe and effective and can be used to remove cysts regardless of size or location and should be considered as a primary therapeutic option in the resection of bronchogenic cysts. Fiever et al. [4] compared the results of surgical treatment of bronchogenic cysts in children and adults. Early surgical resection of bronchogenic cysts provides better preservation of lung parenchyma, a lower incidence of inflammatory lesions, and a lower rate of complications.
The uniport is used in thoracoscopic surgery to reduce invasiveness. Cheng et al. [5] reported that uniport thoracoscopic surgery was associated with less bleeding, shorter duration of postoperative drainage, shorter length of hospital stay, and lower visual analog pain scores on Days 1 and 3 postoperatively compared with the use of two or more ports.
The prone position has been introduced to perform minimally invasive esophageal resection. It used to be performed in the lateral decubitus position, but the esophagus is the most dependent part is such a situation, so a small amount of blood can overlie the lung and obscure the view. In the prone position, exposure occurs by gravity. The lung falls away, allowing minimal handling, and the esophagus is clearly visible, making dissection easy [6]. Resection of an esophageal bronchogenic cyst involves exposure of the esophagus and separation of the cyst from the esophageal wall. Therefore, the prone position, which facilitates exposure of the esophagus, was useful for performing the surgery.
A magnified view with a thoracoscope confirmed that there was no damage to the esophageal mucosa. The esophageal mucosa in contact with the bronchogenic cyst is stretched. It is common to suture the esophageal muscle and surrounding tissues to prevent the mucosa from protruding after surgery. The author sutured the barbed suture continuously in two rows. Operational time was reduced by not tying the suture. Hafermann et al. [7] stated that barbed sutures can save endoscopic surgery time by eliminating knot tying and avoid problems such as granulation tissue formation associated with surgical knots. Tension is distributed evenly along the suture line, reducing stress on the wound and improving healing.
In conclusion, a single-incision VATS was performed in the prone position for a patient with an esophageal bronchogenic cyst. The magnified view of the thoracoscope confirmed that there was no esophageal mucosal damage. The patient was able to resume his diet on the day of surgery and made a rapid recovery.
Conflict of interest statement
None declared.
Funding
None declared.



