-
PDF
- Split View
-
Views
-
Cite
Cite
Sebastian Radmer, Julian Ramin Andresen, Carpal tunnel syndrome, spinal canal stenosis, cardiomyopathy, renal insufficiency, enteropathy, and diffuse myopathy as an expression of systemic ATTR amyloidosis - diagnostics and therapy, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae183, https://doi.org/10.1093/jscr/rjae183
Close - Share Icon Share
Abstract
Systemic amyloidosis is an incurable multisystem disease, caused by fibrillar protein deposits with resulting dysfunction of affected organ systems. It mostly affects patients > 60 years. Diagnosis is often delayed because the symptoms are nonspecific and highly variable. We report on an elderly patient with multi-organ involvement with proven wild-type transthyretin amyloidosis. The initial manifestation involved bilateral carpal tunnel syndrome and lumbar spinal canal stenosis. The occurrence of ligament and tendon disorders, unexplained muscle pain and polyneuropathy in elderly patients should be considered as a possible first manifestation of systemic amyloidosis.
Introduction
Amyloidoses are a group of rare diseases in which misfolded proteins, the amyloid fibrils, accumulate in the extracellular space of various organs [1]. This leads to progressive functional disorders, with a significant reduction in the quality of life. Among the amyloidoses, transthyretin amyloidosis (ATTR amyloidosis) occupies a special position, as it can be both inherited and occur due to age. In the hereditary form, a mutation is responsible for the disease; the non-hereditary form is called wild-type ATTR amyloidosis. So far, no valid epidemiological data are available for Germany. Age-related wild-type transthyretin (ATTR) amyloidosis is being diagnosed increasingly frequently: 25% of patients over 80 years of age and 13% of patients >60 years of age with heart failure with preserved left ventricular ejection fraction are thought to be affected [2]; accordingly, the prevalence has been underestimated up to now.
A typical course of the disease is described in an elderly patient with progressive multiple complaints in the musculoskeletal system over several years, which were demonstrably caused by a systemic ATTR amyloidosis.
Patient and results
We report on an 84-year-old patient with a progressive course of wild-type ATTR amyloidosis, with a case history going back to onset of the disease 7 years previously.
Clinically, the patient was initially diagnosed with a bilateral carpal tunnel syndrome confirmed by electromyogram (EMG)/nerve conduction velocity (NCV) (Fig. 1), which was treated surgically in the typical manner and led to freedom from symptoms. Over the further course, diffuse pain occurred in both legs, and the pain-free walking distance decreased over time. Colour coded duplex sonography (CCDS) did not reveal any evidence of peripheral arterial occlusive disease. Diabetes mellitus could be excluded by laboratory tests. In the imaging diagnostics carried out by means of magnetic resonance imaging (MRI) of the axial skeleton, an absolute spinal canal stenosis at the level of vertebral bodies L4–L5 due to a marked hypertrophy of the ligamenta flava with additional deforming spondylosis could be confirmed (Fig. 2).
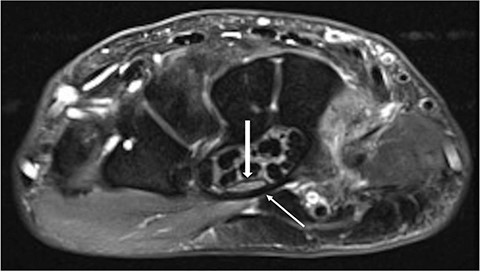
Axial MRI slice showing the carpal tunnel. A thickened transverse carpal ligament (thin arrow) with a clear indentation of the median nerve (thick arrow) is shown.
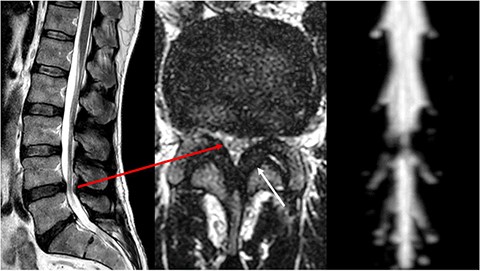
MRI of the lumbar spine. Left sagittal slice with a stenosis of vertebral bodies L4/L5, in the axial slice (centre) corresponding stenosis (long arrow) with clear thickening of the ligamenta flava (short arrow). On the right, there is a clear cerebrospinal fluid blockage in the area of the stenosis.
A subsequent operation with decompression via interlaminar fenestration led to clinical improvement without complete resolution of the symptoms. The histology obtained showed increased amyloid deposition in the ligamenta flava. In parallel, an increasing cardiomyopathy developed, with left ventricular hypertrophy and reduced contractility confirmed by ultrasound and cardiac MRI (Fig. 3). Additional 2,3-dicarboxypropane-1, 1-diphosphonate (DPD) scintigraphy led to a pathognomonic storage in the area of the heart muscle (Fig. 4) and the thigh muscles. Over the course of the disease, the patient experienced significant weight loss and recurrent, sometimes bloody diarrhoea. Colonoscopy with sampling of the rectum confirmed the presence of an amyloid-associated enteropathy. The patient also developed stage 2 renal insufficiency.
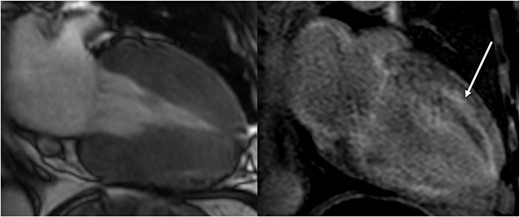
Cardiac MRI (2-chamber view) shows marked hypertrophy of the ventricular musculature on the left in the onset of systole. On the right, there is a clear late enhancement after administration of gadolinium diethylenetriaminepentaacetic acid (DTPA) (arrow).
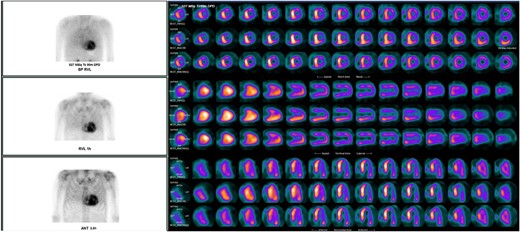
Scintigraphy with single photon emission computed tomography (SPECT) shows markedly increased tracer uptake in the area of both atria and ventricles with septal emphasis.
A subsequent drug therapy to slow down the progression with tafamidis 61 mg/day (Vyndaqel®, Pfizer) [3] for 10 months until the patient’s death, brought a general relief of symptoms with reduction of muscle pain, without the occurrence of side effects.
Discussion
The clinical symptoms of amyloidosis are extremely varied and can affect different organs and body functions [4]. Complaints in the musculoskeletal system are not uncommon and are often not considered appropriately at the onset of the disease. Thus, as in our case, the occurrence of carpal tunnel syndrome can be the first indicator for the presence of systemic amyloidosis [5, 6]. Hahn et al. [5] assume a prevalence of ~12% for the occurrence of carpal tunnel syndrome in patients >50 years of age, so that a histological sample should be taken from the transverse carpal ligament in the case of surgical treatment.
Spinal canal stenosis with hypertrophy of the ligamenta flava is also a frequent clinical picture in patients >60 years of age with systemic amyloidosis. Godara et al. [7] were able to demonstrate ATTR amyloidosis histologically in 13% of their patient population, whereby no patient was younger than 61 years, and men were affected more frequently than women (61% vs 39%).
Klarskov et al. [8] found spontaneous tendon ruptures at different locations in patients with proven amyloidosis in addition to carpal tunnel syndromes and spinal canal stenoses. These were an additional prognostic factor for hospitalization and worsening of cardiomyopathy.
Cardiac involvement with left ventricular hypertrophy is a decisive factor in patient mortality. Early initiation of therapy is crucial for improving quality of life and prolonged survival [9]. Drugs that are now available [4], such as the tafamidis used in our patient, achieve stabilization of the transthyretin tetramer, which slows the progression of the disease [10, 11].
Conclusion
The occurrence of carpal tunnel syndrome, spinal canal stenosis or unclear, diffuse muscle pain as well as cardiac insufficiency may be indications for the presence of amyloidosis.
Early histological clarification is desirable in these cases in order to initiate appropriate therapy.
Due to the complexity of the disease with frequent multi-organ involvement, patients should be treated at a specialized, interdisciplinary centre.
Conflict of interest statement
The authors declare that they have no conflicts of interest.
Funding
None declared.
Data availability
Data supporting this research article are available from the corresponding author on reasonable request.
Consent
Full consent from the patient was obtained for publishing this article and images.



