-
PDF
- Split View
-
Views
-
Cite
Cite
Franciele S Bernardo, Francisco Dada Neto, Ewerton B D S Lima, Paulo H S Lara, Alberto D C Pochini, Carlos V Andreoli, Paulo S Belangero, Benno Ejnisman, Distal rupture of the biceps brachii tendon in a female mixed martial arts athlete: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae147, https://doi.org/10.1093/jscr/rjae147
Close - Share Icon Share
Abstract
The distal rupture of the biceps brachii muscle tendon (DBT) accounts for 3% of biceps ruptures. Diagnosis typically relies on high clinical suspicion and complementary imaging studies, with >90% of cases documented in males between the fourth and sixth decades of life. Reports of DBT ruptures in females are scarce, mostly involving partial and degenerative injuries. Here, we present an unprecedented case of a 28-year-old female professional mixed martial arts athlete with a total traumatic DBT rupture. The athlete underwent surgical repair using anchor reattachment technique. No complications were observed, and the athlete showed satisfactory outcomes, being cleared for physiotherapy after 2 weeks and returning to sports after a 3-month postoperative period.
Introduction
Distal biceps tendon (DBT) ruptures are relatively rare, accounting for 3% of all biceps brachii injuries. However, the incidence of this injury has increased from 1.2 in 2002 to 2.55 per 100 000 patients/year in 2015, with an annual increment of 2.5% [1, 2].
These injuries typically occur in men during the fourh– to sixth decades of life [1–3]. In men, the primary mechanism of injury described is resisted extension with a flexed elbow [4]. Key risk factors include the abusive use of anabolic steroids [4], overweight/obesity (BMI > 30 [4, 5] and smoking. Smokers have a 7.5 times higher risk of distal biceps tendon ruptures [2, 4, 5].
In contrast to documented cases in males, distal biceps tendon (DBT) injuries in women are rare. There is a scarcity of literature on DBT ruptures in women. In our research, we identified two case series detailing both partial and total ruptures [2, 6], along with only six published case reports of complete ruptures of the DBT [3, 7–12].
Case report
A 28-year-old right-handed female, a professional mixed martial arts (MMA) athlete for ~8 years, training ~5.5 hours per day, six times a week, presented with sudden pain and deformity in the anterior region of her left arm 5 weeks ago. This occurred following a cross punch during a match. The patient denied any prior pain complaints in the injured area or in the contralateral arm. She had no comorbidities, tobacco use, anabolic steroids, or corticosteroid usage.
On physical examination (Fig. 1), the patient exhibited a visible deformity of the arm (inverted Popeye sign), a positive Hook test for distal biceps injury, symmetric elbow flexion strength, slightly decreased supination strength with pain, but with a complete range of motion for passive and active pronation-supination and flexion-extension. Ultrasonography and magnetic resonance imaging revealed a complete rupture of the distal biceps tendon (Figs 2–4).



Sagittal MRI Image revealing discontinuity of the DBT and edema in the insertion region.

Axial MRI image showing absence of the biceps tendon in the region of the radial tuberosity and edema in the area.
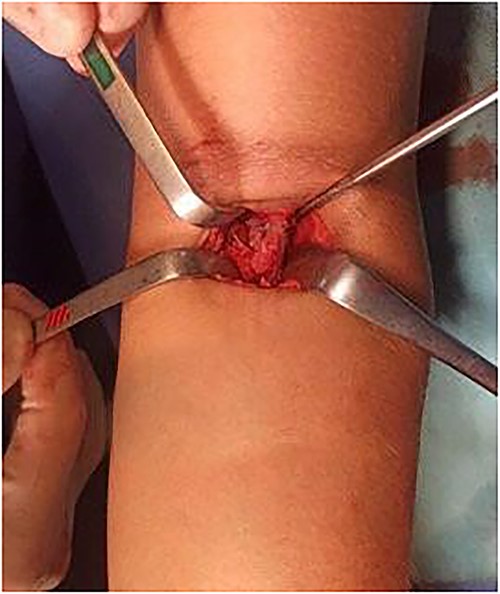
Given this clinical presentation, surgical treatment was recommended for tendon repair. A single-incision technique with fixation using two suture anchors was employed (Figs 5 and 6), following the method described by Maciel et al. [13]: An ~5 cm access incision was made in the anterior region of the proximal third of the forearm in a transverse plane. With the forearm in complete supination and at a 10-degree elbow flexion, two suture anchors were positioned, loaded with high-strength threads, into the radial tuberosity. Fixation of the distal anchor repair was performed first to establish tendon length, followed by fixation of the proximal anchor repair to maximize the tendon-to-bone contact area. Intradermal skin suturing performed.

Following the surgery, the patient was immobilized with a Velpeau sling, maintaining the elbow at 90°. Immobilization was discontinued at 2 weeks, and daily passive physiotherapy was initiated for range of motion improvement until the fourth week. Strengthening exercises began at six weeks postoperatively. No complications arose during clinical follow-up, and the patient returned to sports, engaging in strength training and martial arts activities three months after the surgery. At the 6-month postoperative mark, she participated in a professional competition, demonstrating commendable athletic performance. At the 2-year follow-up, the patient had fully returned to sports without any complaints, expressing satisfaction with the treatment and showcasing excellent esthetic aspects of the incision (Fig. 7).

Clinical image of scar appearance 2 years after surgical procedure.
Discussion
We present a case of a female professional MMA athlete who experienced a DBT rupture during combat. Opting for treatment based on conventional references for male patients, we achieved a highly satisfactory clinical outcome. Consequently, we believe that this case report will facilitate decision-making for colleagues who may encounter similar cases in the future.
In our review, we encountered only two case series on DBT ruptures (both partial and total) in women, one from 2010 [2] with 15 patients and another from 2021 with 26 patients [6]. Regarding case reports of complete ruptures in this gender, we found only six publications (one involving two cases) [3, 7–12].
Predominantly, DBT ruptures occur in men, accounting for ~ 95.7%. In >50% of cases among females, symptoms were reported to have an insidious and non-traumatic onset [4, 5]. In Jockel’s case series from 2015, 87% of the cases involved partial lesions, while in 2021, Rao et al reported 46.2% complete lesions [2, 6]. Notably, sports-related trauma in the largest case series involving women constituted only 7.6% of cases (two cases) [6].
In the published case reports of complete dDBT ruptures in women, comprising a total of seven patients, five experienced traumatic injuries, with only one occurring in a professional sports activity. One patient suffered bilateral injuries due to trauma from softball, treated chronically with reconstruction using allograft. Another patient, aged 72, sustained a traumatic injury during recreational tennis and opted for conservative treatment. There was also a case involving a two-level injury of the DBT after a fall, which was managed with acute repair using suture anchors [3, 7–12].
The remaining four patients with complete DBT ruptures at a single level had diverse traumatic incidents: one during a hockey game, another while professionally ice skating, a third following a non-sports-related fall, and the last one during a robbery. All four cases were treated with acute repair. Among the five patients undergoing acute repair, three had DBT reattachment performed using suture anchors, one through endobutton technique, and the final case did not specify the reattachment method. The patient treated conservatively resumed previous activities ~4 weeks after those managed surgically [3, 7–12].
The increasing involvement of women in sports activities in recent years has contributed to a rise in the incidence of orthopedic injuries [8]. Toczylowki et al. [3] point out that with the growing activity levels and female participation in sports, the frequency of distal biceps tendon ruptures is likely to increase in women.
We present the first case of a complete traumatic rupture of the DBT in a female combat athlete during sports practice. This case demonstrates the potential of surgical treatment through a single-incision approach and reattachment with anchors in high-performance female athletes, leading to the complete recovery of traumatic DBT injuries with an excellent esthetic outcome.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding
This study received no financial support from public, commercial, or non-profit sources.



