-
PDF
- Split View
-
Views
-
Cite
Cite
Jennifer Turco, Synchronous intussusception with primary neuroendocrine tumour in an adult, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae128, https://doi.org/10.1093/jscr/rjae128
Close - Share Icon Share
Abstract
Intussusception in adults is rare. There are only a few cases in the literature that report two lead points resulting in double or synchronous intussusception. We present a case of synchronous intussusception in a 45 year old man with neuroendocrine tumour of the ileocaecal valve and lipomatous polyp of the jejunum.
Introduction
Intussusception occurs when one segment of bowel telescopes into an adjacent bowel segment, causing intestinal obstruction, ischemia, perforation and sepsis [1, 2]. It commonly presents in children but is rare in adults. Adult intussusception accounts for 1% of all bowel obstructions, 5% of all intussusceptions, and 0.003%–0.02% of all hospital admissions [3]. The aetiology of intussusception in adults is almost always pathological. In >90% of cases, there is an intraluminal lesion which acts as a lead point and in 50% of cases the lesion is malignant and therefore surgical resection is recommended [3]. Case series of double intussusception with two lead points have been reported in children but there only two cases reported in adults [4–6].
We present a rare case of synchronous ileocaecal and jejunal intussusception in a 45 year old male.
Case report
A 45 year old male presented to the emergency department with epigastric pain and history of treated helicobacter pylori gastritis. He was discharged with a diagnosis of gastritis but re-presented 24 hours later with worsening severe, crampy abdominal pain, nausea and vomiting, and abdominal bloating. The abdominal pain was worse in the epigastrium and right upper quadrant and exacerbated by movement and eating. The patients bowels had not opened for three days and the patient had poor oral intake due to nausea and vomiting. The patient had no previous abdominal surgery.
On examination, the patient was in significant discomfort and required opioid analgesia. Vital signs were within normal limits with heart rate of 50 beats per minute (bpm) and blood pressure of 150/70 mmHg and afebrile. His abdomen was tender with guarding in the epigastrium, right upper quadrant and lower abdomen, and there was a palpable mass in the right lower quadrant.
Haematological investigations revealed raised inflammatory markers with white cell count of 21 ×109 g/L with neutrophilia 19.5 × 109 g/L (ref range and C-reactive protein of 5.1 mg/L (ref range < 3.0). Haemoglobin level was high-normal 171 g/L (ref range 125–175) likely due to hypovolemia from vomiting and poor oral intake. The urine, electrolytes and creatine, liver function tests and lipase were all within normal limits.
Computer-tomography (CT) demonstrated two points of synchronous intussusception. First, a relatively long segment ileocolic intussusception (Fig. 1) with dilated distal ileum containing faeculent matter, indicative of bowel obstruction. Second, a short segment small bowel intussusception involving jejunal loops (Fig. 2).
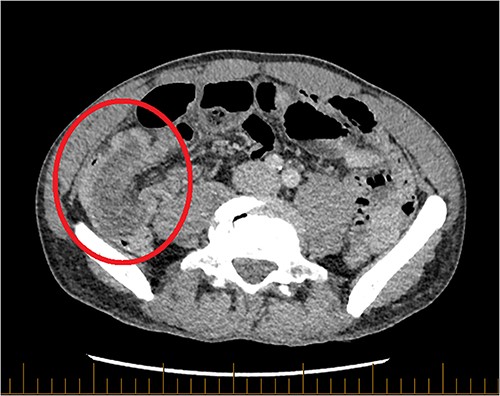
Axial CT of the abdomen and pelvis with portal venous contrast. Long segment of ileocolic intussusception shown (red circle).
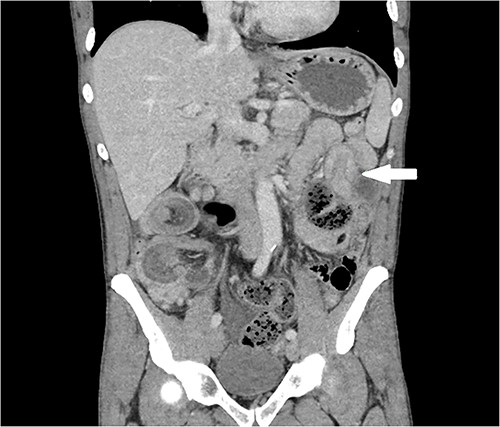
Coronal CT for abdomen and pelvis with portal venous contrast. Jejunal intussusception in left upper quadrant (white arrow).
In the emergency department, intravenous fluid resuscitation was commenced and nasogastric tube was inserted for decompression. The patient proceeded emergently to theatre and underwent laparotomy. The long segment of intussusception involving the right colon and terminal ileum was bulky and oedematous. Reduction was not attempted due to risk of iatrogenic perforation. A right hemicolectomy was performed. The second point of intussusception in the jejunum spontaneously reduced but a palpable polyp was detected. A jejunal enterotomy was performed and a lipomatous polyp underwent mucosal resection.
The patient recovered well and was discharged on Day 8 post operatively. The right hemicolectomy specimen showed a 140 mm length of intussusception of ileum through the ileocaecal valve. Histopathology revealed a well differentiated (KI67 2%, grade 1) neuroendocrine tumour (NET) in the region of the ileocaecal valve measuring 15 mm. Of the 32 lymph nodes harvested, two were positive for metastatic well differentiated NET. Surgical margins were negative (pT2N1Mx). The jejunal polyp histopathology showed a submucosal lipoma. Staging work up including chest CT and liver ultrasound, liver magnetic resonance image (MRI) and Octreotide positron emission tomography (PET) showed no metastasis. Non hormonal biological marker, Chromogranin A, was tested three months post resection and was low, 74μg/L (ref -range < 102).
The case was discussed at the NET multi-disciplinary team meeting and ten year surgical follow up was recommended.
Discussion
Intussusception is rare in adults and evidence is limited to several single institution, retrospective case series and expert opinion. Due to the high likelihood of intraluminal lesion as a lead point and associated risk of malignancy the literature recommends surgical resection rather than reduction [2, 7–10]. However, in some cases when the cause is idiopathic non-operative management and observation may be appropriate [11].
Children with intussusception typically present with a triad of symptoms including abdominal pain, red currant jelly stools and palpable mass [2]. In contrast, the presentation of adult intussusception is usually atypical with non-specific abdominal pain that can be intermittent and chronic [7]. Diagnosis is often missed or delayed. This patient presented to the emergency department with epigastric pain and a history of gastritis and therefore was treated with intravenous proton-pump inhibitors. The pain resolved during the period of observation and he was discharged. His re-presentation with worsening pain prompted surgical review and intussusception was only diagnosed on CT scan after surgical review noted the palpable mass and guarding. Although rare, intussusception should be considered as a cause for recurrent abdominal pain with signs of subacute bowel obstruction and CT scan can help to confirm the diagnosis and identify the cause.
This is a rare case of synchronous adult intussusception with the lead point a rare primary NET of the ileocaecal valve. Due to the low incidence of adult intussusception there is a paucity of high quality evidence to support management decision. This case supports the recommendation for surgical resection as it identified a grade 1 well differentiated NET and the patient had a favourable outcome.
Conflict of interest statement
None declared.
Funding
None declared.



