-
PDF
- Split View
-
Views
-
Cite
Cite
Satoshi Miyamoto, Shin Sasaki, Hiroyuki Kojin, Ken Okazaki, Total knee arthroplasty for knee osteoarthritis associated with abnormal patellar tendon deformity: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae102, https://doi.org/10.1093/jscr/rjae102
Close - Share Icon Share
Abstract
There have been no earlier reports of knee osteoarthritis with valgus knee deformity in which the patellar tendon infiltrates the tibial bone marrow instead of attaching to the tibial tubercle. This case report describes a total knee arthroplasty (TKA) performed for the treatment of a primary knee osteoarthritis resulting from a valgus knee joint position attributed to an abnormality of the patellar ligament attachment. During a TKA, the tendon tissue in the tibial medullary canal interfered with the reamer used to prepare for the stem extensions needed to improve the fixation of the component on the tibia, which had a cortical defect. The arthroplasty succeeded, and good clinical results have been maintained over the 3 years since the surgery. Surgeons should consider careful preoperative examinations by magnetic resonance imaging or CT when an abnormal bone defect is observed at the tibial tubercle on plain X-ray images.
Introduction
The patellar tendon attachment extends to the nonarticular part of the patella surface, up to the distal edge of the patellar articular surface, and to the distal attachment to the tibial tubercle [1]. Patellar tendonitis is caused by the dissection of the attachment located between the patella and patellar tendon [2]. To the best of our knowledge, there have been no earlier reports of knee osteoarthritis with valgus knee deformity in which the patellar tendon infiltrates the tibial bone marrow instead of attaching to the tibial tubercle.
This case report describes a total knee arthroplasty (TKA) performed for the treatment of a primary knee osteoarthritis resulting from a valgus knee joint position attributed to an abnormality of the patellar ligament attachment.
Case report
A 73-year-old Asian woman had been undergoing conservative treatment, but the pain gradually worsened, and she was referred to our hospital for TKA.
The patient had no specific history of trauma to the knee but had undergone a surgery for gastric cancer 3 years before.
On physical examination, the patient extension and flexion were − 20° and 130°. A defect of the tibial tubercle was observed. The Knee Society (KS) score was 44 points, and the Knee Society function (KS-F) score was 70 points. A plain radiography showed valgus knee osteoarthritis assessed as Kellgren–Lawrence grade 4. In addition, a well-defined translucent image of bone appeared near the central part of the proximal tibia and no tibial tubercle could be observed (Fig. 1). Magnetic resonance imaging (MRI) of the right knee joint showed the patellar tendon appeared from the attachment on the patella with continuity to the tibial bone marrow in T1- and T2-weighted imaging (Fig. 2).
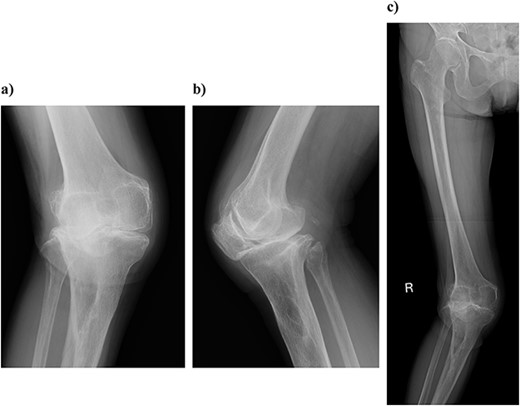
Plain radiography at the patient’s first visit: (a) standing front, (b) lateral side and (c) thigh, standing, front, full length. Valgus knee osteoarthritis and well-defined osteoporosis near the central part of the proximal tibia can be seen, and the rough surface of the tibia has been worn away.
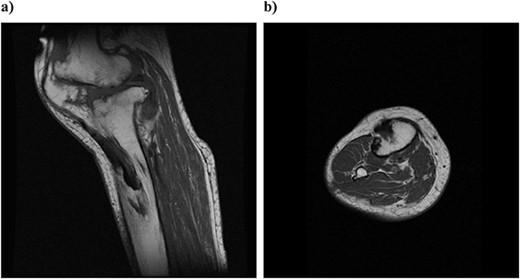
Preoperative simple magnetic resonance imaging: (a) lateral side and (b) axial morphism. T1- and T2-weighted images continuous from the patellar tendon attached to the patella both show continuity from the low signal area to the inside of the tibial bone marrow.
TKA was selected as the treatment to improve her symptoms.
Surgery was performed under general anesthesia, the surgical limb position was supine, and no tourniquet was used. A midline incision of about 20 cm was made, and the joint was reached by the parapatellar approach.
The knee was replaced with a Scorpio NRG PS type system (Stryker Orthopedics, Mahwah, New Jersey). The distal femur was cut with an intramedullary rod guided at 6° valgus. The tibia was cut with an extra medullary rod 10 mm from the medial joint surface, and a cutting guide was installed at a posterior inclination of 0°. The tibia was reamed, once a depth of about 30 mm was reached, the reamer could not be easily advanced. Once the tip of the reamer was confirmed, the tendon fiber was wrapped around the remar (Fig. 3). When palpated from the anterior lateral side of the tibia, the invasion of the patellar tendon into the bone marrow was confirmed. The patella was cut 8 mm from the articular surface. In addition, poor tracking of the patella caused lateral release. All of the prostheses were fixed using bone cement. Slight dilation of the medial joint space was observed at the time of closure, and the fascial was sutured with an overlapping stitch (Fig. 4). The operation time was 190 minutes and the amount of intraoperative bleeding was 238 ml.
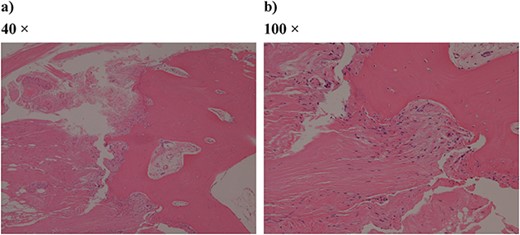
Pathologic specimen from surgery (hematoxylin–eosin staining): (a) 40 times and (b) 100 times. Bone tissue and fibrous tissue are both conspicuous, and ligament-like tissue is partially observed.
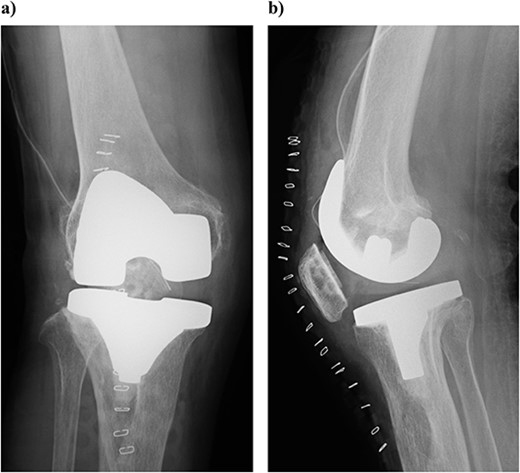
Plain radiography immediately after the surgery: (a) front and (b) lateral side. A slight dilation of the medial joint space is observed.
On postoperative Day 1, the knee joint was fixed with a hinged knee brace and rehabilitation was started. The continuous passive motion (CPM) was started twice daily. The hinged knee brace was removed on Day 33 and the practice of climbing stairs was started on Day 36.
At 3 years postoperatively, the patient could walk independently. Her extension and flexion were − 5° and 120°, respectively, her KS score was 83 points, and her KS-F score was 90 points. Radiography showed a slight valgus position, with some lateral subluxation of the patella, but the patient reported no problems with her activities of daily living (Fig. 5).
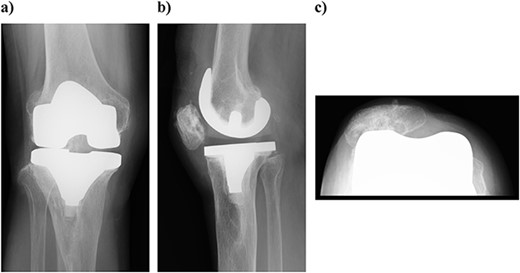
Outcome at 3 years after surgery on plain radiography: (a) standing front and (b) side. The patella is laterally subluxated in a slight valgus position.
Discussion
No reports in the literature before now have described invasions of the patellar tendon into the tibial bone marrow.
In this TKA of the valgus knee, we planned to lengthen the stem of the tibia because the balance between the medial and lateral sides could not be achieved, and because the patellar tendon entered the tibial bone marrow. As the patellar tendon was found to be involved at that depth, the extension of the stem was abandoned. If we had taken a CT to predict the occupation rate of the patellar tendon in the medullary cavity, we might have had the option of changing the direction of the reaming or taking some other countermeasure.
Many reports have described the length of the patellar tendon. Gloria et al. [3] reported that the patellar tendon was clearly shorter on the left in many individuals, and that no sex differences were evident.
Guijin et al. [4] reported that the lateral approach was useful for valgus knee. We believe that the lateral approach should be considered when the medial approach does not provide a sufficient field of view.
TKA of the valgus knee is considered to be prone to patellar subluxation. Kawaguchi et al. [5] suggested that the condition be prevented by considering differences in postoperative rotational kinematics when selecting the implant and planning the surgical technique. Detailed preoperative planning, careful selection of the mechanical implants and the engagement of an experienced surgeon may be useful in preventing postoperative patellar subluxation.
Cheng et al. [6] reported that primary repair of an MCL injury during TKA could provide an excellent clinical outcome with good stability. By sufficiently evaluating the MCL during the operation we report here, we expected the medial laxity observed intraoperatively would improve.
If a defect is found at the tibial tubercle on X-ray examination, the surgeon should consider evaluating the soft tissue on MRI when planning the surgery. If anatomical abnormalities in bone morphology are found, the shape of the bone must also be evaluated on CT. Based on the image evaluations, it was necessary to plan for options, in preparation for the TKA.
In conclusion, we performed a TKA for a case valgus knee osteoarthritis thought to have been caused by an abnormality in the attachment of the patellar ligament. Surgeons should consider careful preoperative examinations.
Acknowledgements
We would like to thank the late Dr. Masahide Kosugi for supervising the paper and Dr. Masahiko Kuroda, a pathologist, for providing the pathologic specimen.
Author contributions
Satoshi Miyamoto: This report, performed the surgery, and supervised the preparation of the manuscript. Shin Sasaki: Edited the manuscript. Hiroyuki Kojin: Comprehensively supervised and edited the manuscript. Ken Okazaki: Edited the manuscript.
All of the authors have read and approved the final version of the manuscript.
Conflict of interest statement
None declared.
Funding
This research did not receive any external funding.
Data availability
The data presented in this study are available from the corresponding author, when requested for reasonable purposes.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Kosei Chuo General Hospital. Informed consent for publication was obtained from the family of the patient.



