-
PDF
- Split View
-
Views
-
Cite
Cite
Dai Kimura, Yusuke Miyagawa, Masafumi Miyao, Hideyasu Matumura, Shoichiro Koike, An adult right inguinal hernia and cryptorchidism treated simultaneously with laparoscopic transabdominal preperitoneal repair and laparoscopic orchiectomy: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae096, https://doi.org/10.1093/jscr/rjae096
Close - Share Icon Share
Abstract
Pediatric health checkups have been mandatory for all citizens since 1966 based on the Maternal and Child Health Law in Japan, and cryptorchidism or undescended testis in adult males are rare. We report a case of an adult right inguinal hernia and cryptorchidism treated simultaneously with laparoscopic transabdominal preperitoneal repair and laparoscopic orchiectomy. A 35-year-old man came to our department with a chief complaint of bulging in the right inguinal region for several months. He was diagnosed with a right inguinal hernia and was scheduled for transabdominal preperitoneal repair. During intraoperative intraperitoneal observation, a white 30-mm mass was found in the hernia orifice. A diagnosis of right cryptorchidism was made, and transabdominal preperitoneal repair and laparoscopic orchiectomy were performed. Laparoscopic simultaneous surgery could be safely performed in an adult patient with a hernia complicated by a cryptorchidism. It can be recommended as a surgical option in such cases.
Introduction
Cryptorchidism is the most common congenital anomaly in boys, but it is rarely noted in adults. To our knowledge, only 12 cases of simultaneous laparoscopic surgery of an adult cryptorchidism and inguinal hernia have been reported. In this report, we describe the simultaneous treatment of an adult right inguinal hernia and cryptorchidism by laparoscopic transabdominal preperitoneal repair (TAPP) and laparoscopic orchiectomy in a foreign worker patient.
Case report
A 35-year-old man, a foreign worker, came to our department with a chief complaint of bulging in the right inguinal region for several months. He was 175 cm tall, weighed 75 kg, and his vital signs were normal. His abdomen was flat and soft, and there was a bulge in the right inguinal region when standing. The inguinal bulge was insertable. Preoperative physical examination could not reveal undescended testis. There were no special findings in blood tests.
CT examination revealed an indirect inguinal hernia and protrusion of intra-abdominal fat (Fig. 1a). Based on these findings, the patient was diagnosed with a right inguinal hernia and was scheduled to undergo a laparoscopic hernia repair (TAPP). Intraoperative observation revealed a 30-mm white mass in the dorsal part of the hernia orifice (Fig. 2). Intraoperative physical examination of the patient revealed that the right testicle was not palpable, and the patient was diagnosed with intraperitoneal testis. The hernia was an indirect hernia ~2 cm in diameter at the hernia orifice. A review of the CT scan revealed a slightly hyperabsorbable mass near the internal inguinal ring, which was thought to be a right cryptorchidism (Fig. 1b). Since there were no relatives of the patient who could give consent for the surgery in Japan, the surgery was suspended. We explained the need for the orchiectomy to the patient and obtained his consent for the surgery. Simultaneous TAPP and laparoscopic orchiectomy were planned at a later date. Under general anesthesia, the operation was performed with three ports: one 12-mm port umbilical and two 5-mm ports bilateral abdominal. Bird® 3D Max L size mesh was used for the right port. The right testicle was removed from the umbilical port wound using an extraction bag after clipping the deferent duct, testicular vessels, and gubernaculum testis (Fig. 3a–c). The operation time was 150 minutes, and the blood loss was 0 ml.
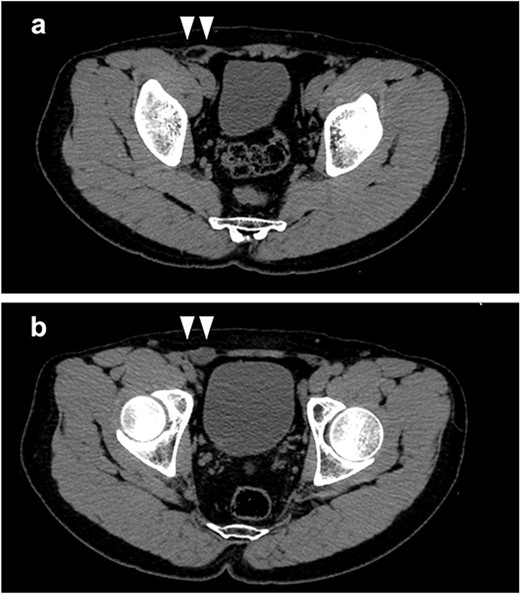
(a) Intra-abdominal fat was found to be prolapsed from the lateral side of the inferior epigastric vessels; (b) a low-density mass (white arrows) in the cranial side of the internal inguinal ring was detected, which was considered to be an intraperitoneal testis.
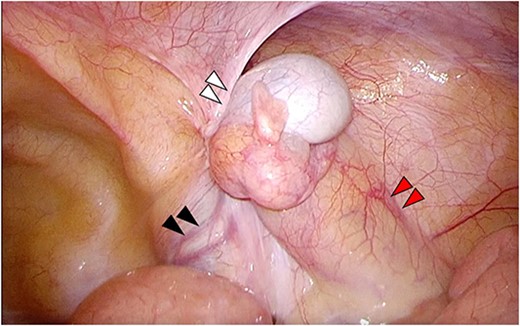
Laparoscopy reveals a white mass (white arrows) dorsal part of the hernia orifice; the deferent duct (black arrows) and testicular vessels (red arrows) were observed.
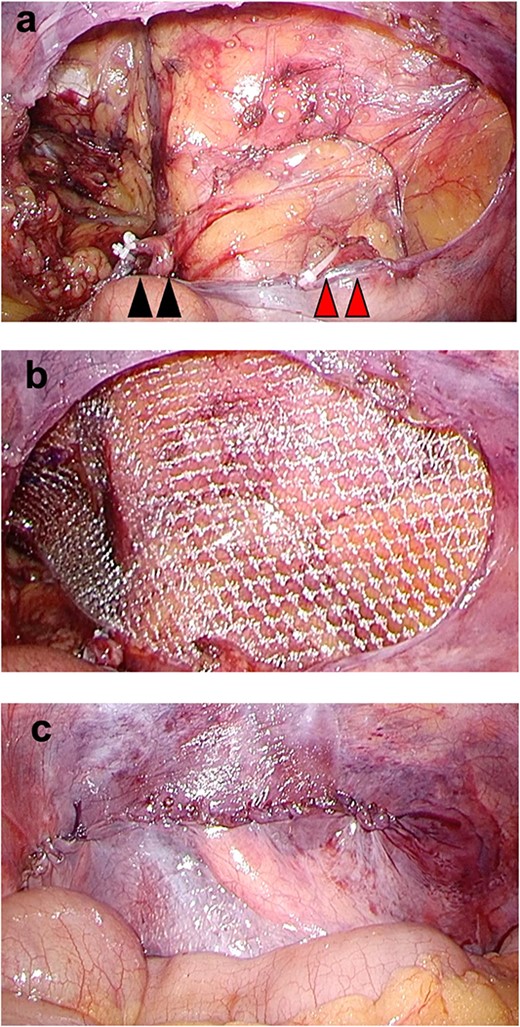
(a) The deferent duct (black arrows) and testicular vessels (red arrows) were divided after clipping; (b) a mesh was inserted leaving the ductus deferens and arteriovenous vein of the testis on the peritoneal side; (c) suture closure was done and the testis was removed and hernia repair was completed.
Macroscopically, right testis was a grossly atrophic testis, 30 mm in size (Fig. 4). Histopathological examination revealed an extensive hyalinization of the seminiferous tubule and aggregation of Leydig cells associated with an undescended testis. Few testicular sperm were observed. There were no malignant findings (Fig. 5a and b).

The resected right testis was a atrophic testis grossly and was 30 mm in size.
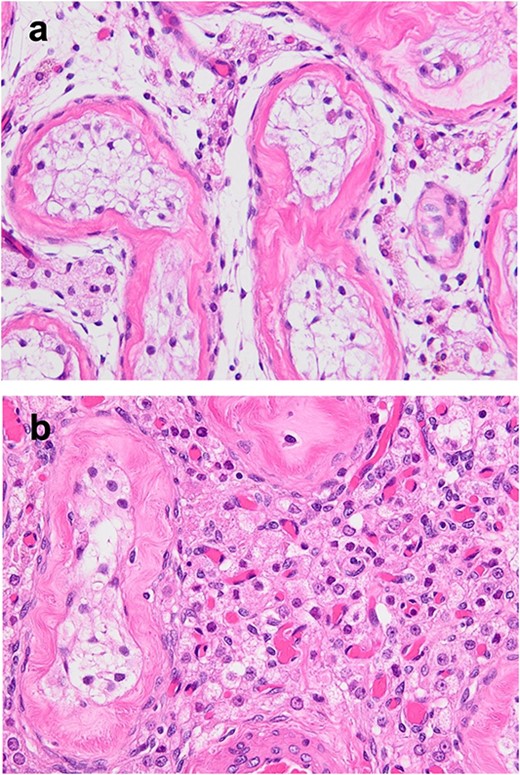
(a, b) HE staining; extensive hyalinization of seminiferous tubules and accumulation of Leydig cells associated with undescended testis were observed; almost no semen formation was observed in the seminiferous tubules; there were no malignant findings.
There were no postoperative complications, and the patient was discharged on the second postoperative day.
Discussion
Cryptorchidism or undescended testis is one of the most common congenital anomalies in males. The incidence of cryptorchidism ranges between 2% and 5% in full-term boys and 30% in premature boys [1]. It is presumed to be related to hormone secretion, heredity, and environmental factors, but the exact cause is unknown. The incidence decreases to ~1% at 3 months of age because spontaneous descent from the testes into the seminal vesicle occurs due to endogenous testosterone secretion by 3 months of age. Since spontaneous descent is unlikely after 6 months of age, guidelines for the treatment of undescended testis recommend orchidopexy from around 1 to 2 years of age [2].
The most common occasion for diagnosis of cryptorchidism is pediatric checkups. In Japan, pediatric checkups and maternal and child health guidance have been mandatory for all citizens since 1966 based on the Maternal and Child Health Law, so it is rare for an adult to be diagnosed with cryptorchidism. On the other hand, there are some overseas countries that do not have a pediatric health examination system at all. One of the reasons why this case was not diagnosed as having cryptorchidism until adulthood could be due to the fact that cryptorchidism screening was not performed sufficiently during childhood.
In the treatment of cryptorchidism, it is necessary to consider treatment from the two viewpoints of spermatogenesis and malignant transformation. It has been reported that atrophy of the seminiferous tubules, decrease in the number of spermatogonial cells, and hyperplasia of the interstitium progress in cryptorchidism after the age of 1.5 years [2]. It is also known that untreated cryptorchidisms have an increased risk of developing testicular tumors after the age of 10 years [3], and the restoration of fertility by orchidopexy after adulthood is not clear [4]. For these reasons, unilateral cryptorchidism in adults is an indication of an orchiectomy. In the present case, the patient had a unilateral undescended testicle, and we judged that fertility could be secured by preserving the healthy side after removal, and we performed an orchiectomy. Histopathological examination revealed no malignant findings, but an extensive hyalinization and atrophy of the seminiferous tubules, and few spermatocytes could be identified. It was considered to be an atrophic change of the testis in a long-standing cryptorchidism.
It has been reported that when the testis does not descend from the abdominal cavity, the perineal sheath process remains open, causing an inguinal hernia. Previous studies have shown that cryptorchidism are potentially associated with ~90% of inguinal hernias [5]. However, since most cryptorchidisms are diagnosed and treated in childhood, the incidence of cryptorchidism in adult patients with inguinal hernias in Japan is rare.
Laparoscopic hernia repair is one of the standard procedures for inguinal hernia surgery, which is classified into TAPP and totally extraperitoneal repair. Both procedures allow a detailed anatomical visualization of the inguinal structures, and these are also applicable for repairing all types of inguinal hernias. The TAPP technique allows a direct visualization of intra-abdominal structures that could not be visualized by CT. There have been only 12 reports of laparoscopic hernia repair for inguinal hernias with cryptorchidism in adults, including this case, and 10 reports of TAPP, including this case [6–14]. The most common reason for detection of cryptorchidism was the inability to palpate the testicles, suggesting the importance of a detailed physical examination of inguinal hernia patients, including palpation of the testicles. In the previous studies, all of the laparoscopic vasectomies and TAPP could be performed without laparotomy or conversion to an anterior approach. All patients were discharged without major complications. Simultaneous laparoscopic orchiectomy and TAPP were useful in adult patients with inguinal hernias and cryptorchidism.
Conflict of interest statement
None declared.
Funding
None declared.



