-
PDF
- Split View
-
Views
-
Cite
Cite
Leshae A Cenac, Maria Cacciotti, Tracy Griffith, First-trimester uterine rupture in a twin gestation after a motor vehicle collision: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae081, https://doi.org/10.1093/jscr/rjae081
Close - Share Icon Share
Abstract
Uterine rupture following trauma in pregnancy is rare, especially in earlier gestational ages. The diagnosis can be challenging, and treatment may be delayed when patients present with nonspecific findings. Therefore, a high index of suspicion must be maintained. Once diagnosed, the treatment involves surgical exploration. We present a case report of a first-trimester uterine rupture of a twin pregnancy following a motor vehicle collision in a patient with prior cesarean sections.
Introduction
Uterine rupture is a fatal obstetric complication and is associated with high rates of fetal and maternal morbidity and mortality [1]. The maternal mortality rate related to uterine rupture is ~10%, whereas the fetal mortality rate can be as high as 100% if the rupture occurs in the trauma setting. A complete uterine rupture occurs when all the layers of the uterine wall including the serosa are disrupted. In contrast, an incomplete uterine rupture spares the serosa and is mostly discovered as uterine dehiscence at the time of cesarean section [1, 2]. Once uterine rupture is suspected, exploratory laparotomy should be quickly performed because pregnant patients have an increased tolerance to hemorrhage because of increased maternal plasma volume. Additionally, clinical signs of hemorrhage like tachycardia and hypotension can be absent until 20% of the total blood volume is lost [3, 4].
We present a case of a complete uterine rupture in the first trimester after a motor vehicle collision (MVC) in a patient with a history of four cesarean sections. In a subsequent pregnancy after the MVC, three areas of uterine dehiscence were incidentally noted in the lower uterine segment during a repeat cesarean section. This case report emphasizes the need for high clinical suspicion of uterine rupture after obstetric trauma in patients with risk factors, regardless of gestational age, and guides optimal delivery timing in subsequent pregnancies.
Case report
A 24-year-old female G6P3114 at 11 weeks 6 days gestational age with a twin pregnancy and a history of four cesarean sections presented to the emergency department (ED) as a restrained driver following an MVC. The patient ran a red light and collided head-on at 60 mph. There was significant front-end damage to the vehicle requiring extrication. In the ED, the patient complained of diffuse abdominal pain. She denied any vaginal bleeding.
The patient’s initial hemoglobin was 12.2 g/dL, and her platelet count was 297 k/uL. A Focused Assessment with Sonography in Trauma (FAST) exam was performed and negative. No fetal architecture was noted within the uterine cavity during the FAST exam. Computerized tomography scan of the abdomen and pelvis showed a gravid uterus with mild scattered intraperitoneal free fluid and scattered increased density greatest ventral to the uterus, suggesting a hemoperitoneum with possible associated uterine rupture. Transvaginal ultrasound revealed no evidence of an intrauterine gestation and free fluid was noted within the cul-de-sac (Fig. 1). Given the high suspicion of uterine rupture based on the clinical presentation and imaging, an exploratory laparotomy was performed.
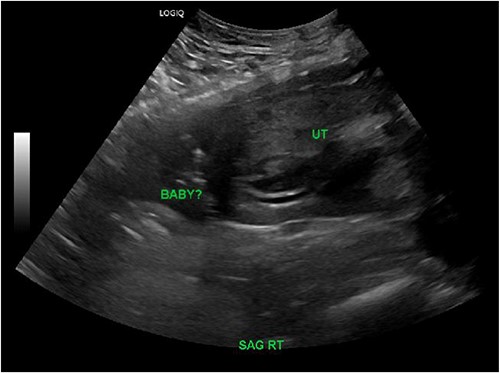
Right sagittal view on transvaginal ultrasound showing an empty uterine cavity with possible fetus outside of the uterus.
Upon abdominal entry, hemoperitoneum was identified and 200 mL of blood was evacuated. Both fetuses were noted to be free-floating in the abdomen (Fig. 2). A 2-cm uterine rupture was identified likely along the prior hysterotomy site (Fig. 3). An ~3 × 3 cm non-expanding hematoma was noted just under the serosa in the midline of the lower uterine body. The placental tissue and clots within the uterus were removed with sharp curettage through the 2-cm uterine rupture site. The hysterotomy was then closed with 2-0 Vicryl in a running-locked fashion. The fascia, subcutaneous tissues, and skin were closed in standard fashion.
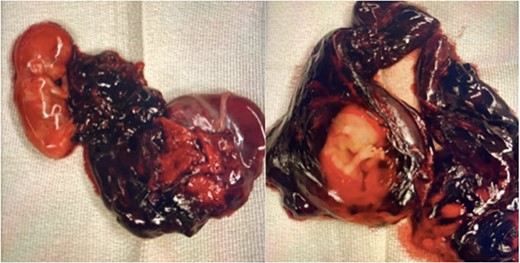
Fetus A (left) with grossly normal phenotype with attachment to the placenta. Fetus B (right) with grossly normal phenotype and intact amniotic membranes.
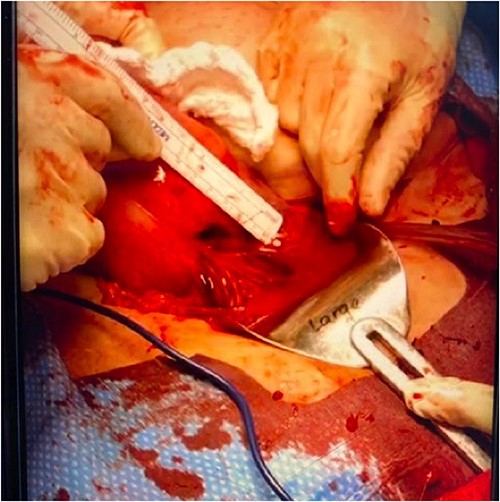
Two-centimeter complete uterine rupture site on the anterior lower uterine segment, likely at the site of prior hysterotomy.
The patient achieved another pregnancy a little over a year after the MVC and was delivered by repeat cesarean section at 37 weeks and 2 days gestational age after presenting to an outside facility with painful uterine contractions. According to the operative report, three areas of uterine dehiscence were identified in the lower uterine segment, each measuring 2–3 cm with intact serosa.
Discussion
Uterine ruptures during the first trimester mainly occur on a scarred uterus [5]. Patients with a history of uterine rupture are at an increased risk of spontaneous uterine rupture before the onset of labor in subsequent pregnancies. After obstetric trauma, the FAST exam is a handy assessment tool for pregnant patients. Obstetric ultrasounds can also efficiently assess fetal heart tones [3].
Over 50% of uterine rupture cases require surgical exploration to confirm diagnosis and laparotomy is the most commonly employed surgical approach. According to Perdue et al. [6], laparotomy was used to repair 54 out of 61 cases of first-trimester uterine rupture. In the case of our patient, laparotomy proved to be an efficient method for promptly closing the primary uterine defect, as well as facilitating hemostasis in scenarios where the surgeon is less confident in laparoscopic suturing techniques. Direct visualization and access to the uterine cavity through the defect were valuable in our case. This enabled us to ensure the complete removal of all products of conception by direct curettage. Consequently, there was no need for subsequent dilation and curettage, thus streamlining the entire process. Our uterine defect was closed using a single-layer locked technique, which ensured adequate hemostasis.
While some authors, such as Cecchini et al. [5], have favored double-layered sutures, Perdue et al. [6] utilized a single-layered closure. No guidelines exist to determine the optimal mode of closure related to outcomes in the first-trimester uterine rupture. Our case report is unique because no other case reports have been found that identify patients with first-trimester uterine rupture in their future pregnancies to assess the outcomes.
This case report emphasizes the importance of having a high clinical suspicion for uterine rupture, especially in the setting of an MVC, particularly if the patient has a history of a scarred uterus. Irrespective of the gestational age during which the rupture initially occurred, patients with a history of uterine rupture should be advised on delivery timing in subsequent pregnancies before the onset of labor to minimize the risk of a repeat rupture and reduce the likelihood of unfavorable fetal and maternal outcomes [7, 8].
Conflict of interest statement
None declared.
Funding
None declared.



