-
PDF
- Split View
-
Views
-
Cite
Cite
Mehdi Bourakkadi Idrissi, Younes Dkhissi, Pneumoperitoneum and Chilaiditi syndrome: navigating a diagnostic conundrum, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae056, https://doi.org/10.1093/jscr/rjae056
Close - Share Icon Share
Abstract
Chilaiditi sign represents a rare condition marked by the interposition of the bowel between the diaphragm and liver, mimicking pneumoperitoneum on radiological imaging. The syndrome manifests with gastrointestinal symptoms and is often confused with more serious conditions. This case report presents a rare instance of Chilaiditi syndrome, initially misdiagnosed as pneumoperitoneum based on chest X-ray findings. The patient, a 61-year-old woman, arrived at the emergency department complaining of acute epigastric pain. Initial tests, including a chest X-ray, suggested pneumoperitoneum, but a subsequent contrast-enhanced abdominal CT-scan revealed the interposition of the right colon between the liver and diaphragm, characteristic of Chilaiditi sign. The patient’s symptoms, including abdominal pain and diarrhea, were consistent with Chilaiditi syndrome. The patient was treated successfully with intravenous antibiotics and fluids, showing significant improvement within 48 hours. The report highlights the importance of differentiating Chilaiditi syndrome from other acute abdominal conditions to avoid unnecessary surgical intervention.
Introduction
The Chilaiditi sign is a rare entity. It is often considered as a fortuitous radiological finding, which is visible on a plain abdominal or chest X ray. It is a radiological manifestation of a gas filled bowel’s interposition between the right hemi-diaphragm and the liver, which can mistakenly be confused with pneumoperitoneum [1]. Its incidence is that of 0.3% for chest X-rays and 2.4% for CT-scans [2].
Chilaiditi syndrome is the development of symptoms in association with this radiological finding [3]. The condition was initially identified by Demetrius Chilaiditi, a Greek radiologist, in the year 1910 [4]. It is considered to be extremely rare, with an estimated frequency of between 0.2 and 2.5% of the general population [3].
Although its cause is uncertain, numerous risk factors have been determined, including hepatic factors such as cirrhosis or hepatic atrophy, and anomalies or absence of the falciform ligament. Diaphragmatic factors, such as diaphragmatic paralysis, as well as colonic factors such as anomalies or absence of colonic suspensory ligaments, dolichocolon have also been identified [5].
We present a case of a female patient, who presented at the emergency room with a pain in the upper abdomen, whose chest X-ray showed a pseudo-pneumoperitoneum that has led to further investigation.
Case presentation
We present a case of a 61-year-old woman, with no history of past illness, who presented to the emergency department with acute constant pain in the epigastric region, with a mild fever.
Upon further questioning, she explained that she has been experiencing a constant abdominal pain, mainly localized in the epigastric region, with a sense of abdominal distension, followed by episodes of diarrhea, evolving in a subfebrile context. Clinical examination found a tenderness in the epigastric region, while the remainder of the abdomen was supple.
We then proceeded by performing a blood work, which revealed an elevated white blood cell count of 15.40 × 1,000/𝜇l (4.8–10.8), with a C-Reactive Protein level at 80. Simultaneously, a chest X-ray revealed air beneath the right diaphragmatic dome, suggestive of pneumoperitoneum (Fig. 1).
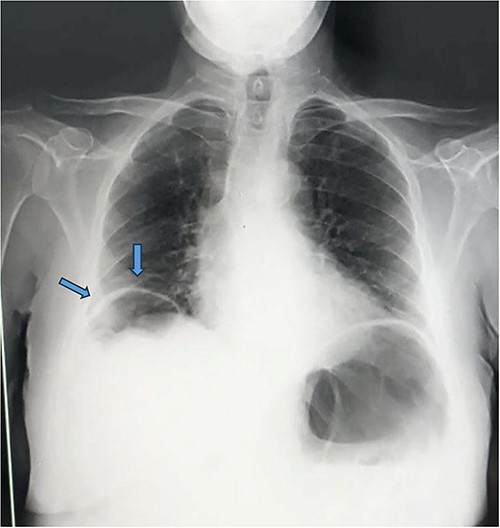
Appearance of pneumoperitoneum beneath the right diaphragmatic dome.
We decided to complete our investigation by performing a contrast enhanced abdominal CT-scan. The result of which showed an interposition of the right colon between the liver and diaphragm, with circumferential thickening of the sigmoid colon, suggestive of an inflammatory or infectious nature, without pneumoperitoneum (Fig. 2).
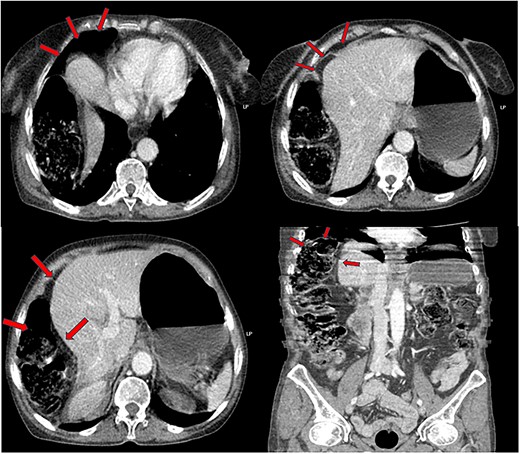
Interposition of the right colic angle and a part of the ascending colon, between the right diaphragm and the liver (image of pseudo-pneumoperitoneum).
A bacteriological and parasitological study of the stool revealed an involvement of Escherichia coli.
Immediately, the patient was started on a course of antibiotics administered intravenously, alongside IV fluids. The following day, we noticed a relief in the abdominal pain, with normal bowel transit. A repeated lab work performed after 48 hours showed a significant decrease in the biological inflammatory markers.
Our patient was discharged after 2 days stay, on oral antibiotics, and a follow-up consult scheduled 1 week later was satisfactory with no signs of abdominal discomfort.
Discussion
Chilaiditi sign is radiolucency in the subdiaphragmatic space that results from bowel interposition between the diaphragm and the liver [6].
The absence of the hepato-diaphragmatic space and intact digestive tract in the normal anatomy of the hepatic region prevents the above-mentioned interposition. This prevention is attributed to the presence of organ-fixing structures, including the mesentery, the greater omentum apron, the peritoneum, digestive ligaments, and vascular pedicles. Elevated intra-abdominal pressures, along with intestinal gas distension and, notably, digestive mobility, play a central role in the creation of a virtual inter-hepato-diaphragmatic space [7].
This sign can be mistaken with a pneumoperitoneum, which signifies the presence of a perforated intra-abdominal bowel, particularly if accompanied by signs such as abdominal tenderness and guarding. Conversely, a pseudo-pneumoperitoneum describes the presence of intra-peritoneal air which appears as free, but in reality, it is contained within an organ [1, 8].
As per the literature, the Chilaiditi sign transforms into the Chilaiditi syndrome when discernible gastrointestinal symptoms arise (such as abdominal pain, anorexia, nausea, vomiting, or constipation) due to compression or obstruction of the interposed visceral segment between the liver and the right hemidiaphragm [3].
Our patient presented with abdominal pain and bloating, alongside diarrhea.
Its differential diagnoses include right diaphragmatic hernia, but more importantly, diagnostic and therapeutic emergencies such as pneumoperitoneum and subphrenic abscess, which may erroneously lead to surgical explorations [5].
It is highly important to differentiate each entity, mainly due to management differences.
The Chilaiditi sign typically does not necessitate treatment. In cases of the syndromic form, symptomatic management involves the use of laxatives and hydration. Surgical intervention is rarely indicated unless complications, such as perforation and arise [3, 6, 7].
Chilaiditi syndrome is generally managed through medical means, with surgical intervention being considered in instances of obstructive complications to alleviate the obstruction and prevent future recurrences [9].
Surgery procedure is only performed if the patient does not respond to the conservative treatment or there is evidence of bowel ischemia or mechanical bowel obstruction. Therefore, differentiating Chilaiditi’s syndrome with other causes of an acute abdomen, as well as careful monitoring during conservative treatment are very important in the management [2, 8].
In most instances, patients with this condition respond well to conservative management. Surgery is primarily reserved for cases where conservative treatment fails or there is a suspicion of serious complications such as ischemia or perforation. When surgery is necessary, it can be conducted using traditional open techniques, or minimally invasive approaches such as laparoscopic or robotic surgery [2, 6]. The surgical strategy might involve resecting the affected part of the colon, known as a right hemicolectomy, or affixing the liver to the abdominal wall to eliminate the space that allows for colonic displacement [7].
Conclusion
Chilaiditi’s syndrome and sign frequently present as diagnostic challenges, often resembling hollow viscus perforation due to the presence of pseudo-pneumoperitoneum on X-ray images, which can lead to unwarranted surgeries. Ensuring an accurate diagnosis is vital to circumvent such invasive treatments, with a preference for conservative management in cases without complications. Medical professionals should integrate a patient’s clinical history and physical examination findings to accurately diagnose these conditions and prevent unnecessary surgical referrals.
Conflict of interest statement
None declared.
Funding
No funding was received for this case report.
Data availability
The data that support the findings of this study are available from the corresponding author (MBI) upon reasonable request.



