-
PDF
- Split View
-
Views
-
Cite
Cite
Feng Yu, Xuefeng Bu, Nana Meng, Leizhou Xia, Acute purulent enteritis after appendectomy: report of a case, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae027, https://doi.org/10.1093/jscr/rjae027
Close - Share Icon Share
Abstract
Acute purulent enteritis is uncommon, which occasionally occurs in association with mechanical injuries from foreign bodies of helminth parasites and the contaminated food, leading to bacterial invasion. Herein we report a case of acute purulent enteritis after appendectomy. A 44-year-old male was diagnosed with right lower abdominal pain and vomiting. Acute appendicitis was diagnosed, and an open appendectomy was performed. Postoperatively, the patient developed symptoms of small intestine obstruction. A laparotomy revealed necrosis of the small intestine, and resection was performed. Pathological examination confirmed acute purulent enteritis. Acute purulent enteritis, which is a serious disease resulting in great disaster to patients, following appendectomy is uncommon. Prompt recognition and abdominal computerized tomography scanning are crucial for accurate diagnosis. Early intervention is necessary to prevent complications.
Introduction
Acute suppurative enteritis is a rare and severe condition that can occur following appendectomy. It is characterized by bacterial invasion of the intestine, often associated with mechanical injury from foreign bodies or contaminated food. In this case report, we present a patient who developed acute suppurative enteritis after undergoing appendectomy. Very few such cases have been reported previously [1, 2].
Case report
A 44-year-old male patient was admitted to our department in June 2010 with complaints of metastatic right lower abdominal pain persisting for 26 h and vomiting after eating and drinking. Physical examination revealed tenderness in the right lower quadrant. Urinalysis, amylase, lipase, as well as renal and liver function tests, showed results within the normal range. Laboratory testing indicated a white blood cell count of 16.4 × 109/L, with neutrophils (N) accounting for 0.902. Based on these findings, a diagnosis of acute appendicitis was made.
After approximately 2 h of positive preoperative preparations, an open appendectomy was performed, lasting for 30 min. Intraoperatively, fecalith obstruction of the appendix lumen and edematous wall were observed. Pathological examination confirmed acute suppurative appendicitis (Fig. 1A).
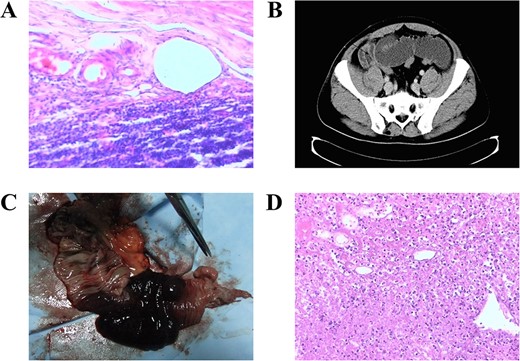
The representative pathological findings and imaging photos of the case. (A) The pathological examination showed acute suppurative appendicitis (Hematoxylin & Eosin staining, ×100). (B) Abdominal CT scan reveals evidence of small intestine obstruction, characterized by the presence of a dilated small intestine with an air-fluid level, as indicated by a black arrow. (C) Resected specimen of the small bowel. (D) The pathological examination revealed the presence of acute purulent enteritis accompanied by intestinal necrosis (Hematoxylin & Eosin staining, ×100).
Postoperatively, the patient experienced a complicated course characterized by fever, followed by abdominal pain, noticeable abdominal distension, cessation of flatus and stool passage, and other symptoms. Conservative treatment measures, including gastrointestinal decompression, parenteral nutrition, fluid replacement and administration of anti-infectives, failed to yield significant improvement. On the fifth postoperative day, abdominal computerized tomography (CT) was conducted, revealing small intestine obstruction (Fig. 1B). Notably, there was evident small intestine expansion with a diameter of approximately 47 millimeters (mm). Subsequently, an immediate laparotomy was performed.
During the second operation, necrosis of the small intestine measuring approximately 150 centimeters (cm) in length, with the affected region located 40 cm from the ileocecal junction, was identified. Additionally, yellow-green exudate was observed in the right upper part of the abdomen. Resection of the necrotic small bowel was carried out (Fig. 1C). The postoperative recovery was uneventful, and the patient was discharged after 9 days. Pathological examination confirmed acute purulent enteritis with intestinal necrosis (Fig. 1D).
A long-term follow-up, spanning over 13 years, was conducted. The patient currently remains asymptomatic, with good appetite, regular bowel habits and a normal body mass index.
Discussion and conclusion
Acute appendicitis is a common surgical emergency in China, often caused by blockage of the appendix by fecalith, foreign objects or, rarely, tumors. The recommended treatment for acute appendicitis is appendectomy, either through open or laparoscopic surgery, to prevent complications such as perforated appendicitis and appendiceal abscess [1, 2].
Acute purulent enteritis is a rare condition that can occur due to mechanical injuries caused by helminth parasites or contaminated food, leading to mucosal defects and subsequent bacterial invasion [3, 4]. Although cases of acute purulent enteritis complicated with submucosal polypoid lymphangioma of the small bowel have been reported [5], there are no previous reports of acute purulent enteritis following appendectomy. In this case, the most likely cause of purulent enteritis was contaminated food. Symptoms of acute appendicitis were present initially, and the postoperative pathology confirmed suppurative appendicitis. However, we suspect that purulent enteritis already existed during the operation, although it was not visible to the naked eye. The pathogenesis of purulent enteritis may be similar to that of appendicitis, with changes in bowel phenotype and impaired enterocinesia contributing to the development of the condition [6, 7].
The occurrence of secondary acute purulent enteritis after appendectomy is uncommon. Recognizing and documenting small bowel responses following major abdominal surgery is crucial for accurate diagnosis. Abdominal CT scanning is commonly used to assess postoperative complications. In this case, contrast-enhanced abdominal CT scan played a significant role in identifying small bowel complications. Therefore, in cases of suspected abdominal complications based on physical findings and laboratory tests, immediate abdominal CT scan should be performed for differential diagnosis.
In conclusion, acute purulent enteritis is a serious disease that can lead to severe complications if not treated promptly. Early intervention is crucial to prevent intestinal perforation, electrolyte disturbance, septic shock and multiple organ dysfunction syndrome.
Ethics approval and consent to participate
Written informed consent for publication of this case report was obtained from the patient and this study obtained ethics approval from the Ethics Committee of Affiliated People's Hospital, Jiangsu University, which was conducted in accordance with the Declaration of Helsinki.
Acknowledgements
The authors thank the studies and books that were included in this article.
Author contributions
Feng Yu, Conceptualization (equal), investigation (lead), writing—original draft (lead); Xuefeng Bu, Conceptualization (supporting), writing—original draft (supporting); Nana Meng, Funding acquisition (supporting), writing—review and editing (supporting); Leizhou Xia, Funding acquisition (lead), conceptualization (equal), writing—original draft (supporting), writing—review and editing (lead). All authors read and approved the final manuscript.
Conflict of interest statement
The authors report no conflicts of interest.
Funding
This work was supported by the funding from the Innovation and Entrepreneurship Plan of Jiangsu province (No. SCBS202101), the Research Foundation of Jinshan Doctor of Zhenjiang City (2021-JSYZ-13) and the Research Foundation of The Affiliated People's Hospital of Jiangsu University (Nos KFB2020005, KFQM-08) from Leizhou Xia, and Science and Technology Planning Social Development Project of Zhenjiang City (FZ2022132, SH2023041) from Nana Meng.
Data availability
All data generated or analyzed during this study were included in this article.



