-
PDF
- Split View
-
Views
-
Cite
Cite
Xi Yang, Yinhuan Ding, Yong Liu, Yixue Shi, Xiaolei Sun, A 17-year-old student with ankle sprain to leg amputation, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae003, https://doi.org/10.1093/jscr/rjae003
Close - Share Icon Share
Abstract
Cutaneous mucormycosis with ischemic complications is a life-threatening condition with high mortality rates, particularly in immunocompromised individuals. The incidence of mucormycosis has increased during the COVID-19 pandemic due to reduced immunity. We present the case of a 17-year-old high school student who experienced a sprained left lower extremity, followed by worsening pain and swelling due to the topical application of unknown local herbs. Eighteen days after the injury, she was admitted to our department in a comatose state with left lower limb ischemia. The patient had a history of uncontrolled diabetes mellitus and displayed a necrotic lesion on her left ankle, suggestive of invasive infectious fungi disease. Diagnostic procedures, including tissue staining and molecular analysis, identified Rhizopus oryzae as the causative organism. Administering amphotericin B yielded marked improvement, but the patient necessitated a mid-thigh amputation to curtail the infection’s advance, culminating in her successful discharge post-treatment.
Introduction
This report describes a critical case of cutaneous mucormycosis in a 17-year-old diabetic student, highlighting the urgency of early diagnosis and aggressive treatment, especially amid the COVID-19 pandemic. It focuses on the diagnostic challenges and treatment strategies for this rapidly progressing infection, particularly in immunocompromised patients.
Case report
A 17-year-old high school student sprained her left lower extremity. Over the 4 days following the injury, topical application of unknown local herbs exacerbated the pain and calf swelling. At 18 days after her ankle sprain, the girl went into a coma and was hospitalized in our department with ‘left lower limb ischemia.’ The patient had diabetes mellitus for three years without regular medication. Physical examination revealed a black necrotic lesion measuring approximately 15 × 10 cm2 on her left ankle, with erythematous blisters and slight edema in the lower leg (Fig. 1). The lesion skin temperature was abnormally low, and the foot and toes failed to flex dorsally. Digital subtraction angiography revealed total occlusion of the anterior tibial artery, posterior tibial artery and dorsalis pedis artery. The patient underwent a midline amputation of the left lower leg.

A black necrotic lesion on the left ankle, erythematous blisters and slight edema in the lower leg.
Given the reason, the history of uncontrolled diabetes mellitus and sprain, and the extreme progression of ischemia in the lower extremities, she was clinically suspected of invasive infectious fungi disease. Tissue staining with periodic acid-silver methenamine demonstrated filamentous fungi with small-vessel invasiveness (Fig. 2). Further staining with lactic acid phenol cotton blue after fungi culture revealed the morphology of the Rhizopus genus (Fig. 3), with creeping mycelium, root-like mycelium (pseudorrhiza), sporangiophore and sporangium. In addition, MALDI-TOF-MS analysis identified Rhizopus oryzae, with a confirmed score of 2.153, as the causative organism. Within amphotericin B therapy, she was rejuvenated, underwent a secondary mid-thigh amputation and then was discharged successfully.
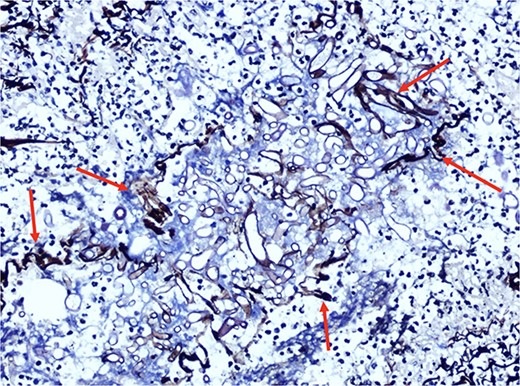
Filamentous fungi were revealed by tissue staining with periodic acid-silver methenamine.

The morphology of the Rhizopus genus on the staining with lactic acid phenol cotton after fungi culture.
Discussion
Mucormycosis, a rare but lethal opportunistic fungal infection, is characterized by its sudden onset, rapid progression, diagnostic difficulty and poor prognosis, with an incidence of approximately 1.7 per million and a mortality rate of 40–80% [1]. Although inhalation of airborne spores or direct ingestion are the main modes of transmission for mucormycosis, spores may penetrate the skin through occult wounds and subsequently invade the vessel wall to produce septic arteritis, causing severe thrombosis or infarction in the cutaneous subtype [2]. Concomitant necrotizing fasciitis is one of the most common skin manifestations of cutaneous mucormycosis [3]. Rhizopus oryzae is reported to be the most common human pathogenic fungus causing mucormycosis [4]. This life-threatening infection characterized by a fast onset, rapid progression and high mortality rate (>50% under standard therapy) usually occurs in immunocompromised individuals, as in this case [5, 6]. During the COVID-19 pandemic, the incidence rate surged considerably due to reduced immunity [7]. Early vigorous surgical debridement, as well as high-dose and full-course intravenous antifungal therapy, are critical in the treatment of mucormycosis.
Conflict of interest statement
All authors have no conflicts of interest to declare that they are relevant to the content of this article.
Funding
This study was supported by the International Science and Technology Innovation Cooperation Project of Sichuan Province (22GJHZ0278), the Sichuan Science and Technology Program (2022YFS0614), the Medical Research Project of Sichuan Province (S21020), the Science and Technology Strategic Cooperation Project of Luzhou Municipal People's Government and Southwest Medical University (2021LZXNYD-D10), and the Doctoral Research Initiation Program of the Affiliated Hospital of Southwest Medical University (19041).
References
- ischemia
- diabetes mellitus
- edema
- amphotericin b
- amputation
- coma
- mycoses
- adolescent
- administration, topical
- ankle
- diagnostic techniques and procedures
- immunity
- immunocompromised host
- mucormycosis
- necrosis
- pain
- thigh
- therapeutic immunosuppression
- natural immunosuppression
- fungus
- leg
- mortality
- ankle sprains
- leg amputation
- lower limb ischemia
- rhizopus oryzae
- cutaneous mucormycosis
- coronavirus pandemic



