-
PDF
- Split View
-
Views
-
Cite
Cite
Zlatan Zvizdic, Melika Bukvic, Nermina Ibisevic, Alena Firdus, Asmir Jonuzi, Semir Vranic, Perforated anterior tenia coli-type appendicitis in a case of vermiform appendix duplex in a toddler: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 12, December 2024, rjae784, https://doi.org/10.1093/jscr/rjae784
Close - Share Icon Share
Abstract
Duplication of the vermiform appendix is a rare anomaly observed in patients undergoing appendectomy. A 27-month-old male toddler presented with a 9-day history of abdominal pain, vomiting, and diarrhea, progressing to an acute abdomen with signs of severe peritonitis. Intraoperative findings revealed a periappendicular infiltrate from a perforated vermiform appendix of the tenia coli type. A second, inflamed appendix was incidentally discovered in its typical location during the procedure. Vermiform appendix duplication presents a clinical challenge due to its rarity and potential for complications. According to the Cave–Wallbridge classification, this case represents Type B2, or the tenia coli variant, characterized by a perforated appendix originating at the tenia coli convergence and a smaller, secondary appendix in a retrocecal position. This case emphasizes the importance of thorough distal and proximal exploration during initial appendectomy when this anomaly is suspected, particularly in cases of Type B2.
Introduction
Although acute appendicitis (AA) is one of the most common nontraumatic indications for surgery, AA in children <3 years of age is a rare finding [1]. An even rarer finding is a duplex appendix with an incidence of 0.004%–0.009% among patients undergoing appendectomy [2, 3]. A vermiform appendix duplex can be an isolated congenital anomaly or associated with cecal duplication. As a routine investigation of appendix duplication is not carried out in clinical surgical practice due to its rarity, synchronous appendicitis or secondary appendicitis of the remaining unrecognized duplicated appendix can cause serious consequences and complications due to delayed diagnosis and treatment. With no acute manifestation of disease, the presence of a double appendix is detected incidentally during surgery or a postmortem examination [2]. Although appendix duplication anomaly is uncommon, it may have substantial clinical and medicolegal significance [4].
We report a case of a 27-month-old male with a tenia coli-type perforated vermiform appendix duplex and secondary inflamed appendix incidentally detected in the usual position during the same surgical procedure.
Case report
A 27-month-old male toddler presented to the Emergency Department with acute abdominal pain and signs of severe peritonitis. He had experienced abdominal pain, vomiting, and diarrhea for 9 days and was initially treated in a regional hospital under the suspicion of acute gastroenteritis, receiving intravenous rehydration, dietary adjustments, zinc supplementation, probiotics, and, subsequently, ciprofloxacin. As his condition worsened over the last 2 days, he was referred to our institution.
On examination, he was febrile, tachypneic, tachycardic, and hypotensive. Abdominal examination revealed a rigid abdomen with a palpable mass and marked tenderness and guarding in the right abdomen. Laboratory results indicated a leukocyte count of 19 × 109/μl, significantly elevated C-reactive protein (210 mg/dl), and a platelet count over 1 000 000/mm3, with normal coagulation tests. Abdominal ultrasound revealed echogenic fluid, prominent and hyperechoic mesenteric and omental fat, and a mass occupying the right abdomen from the subhepatic region to the pelvis. Contrast-enhanced CT of the abdomen confirmed a right abdominal mass adherent to the posteroinferior surface of the liver’s right lobe, cecum, terminal ileum, and right pelvis (Fig. 1A and B), but the appendix was not visualized. Inflammatory changes in the adjacent mesenteric fat were also noted.
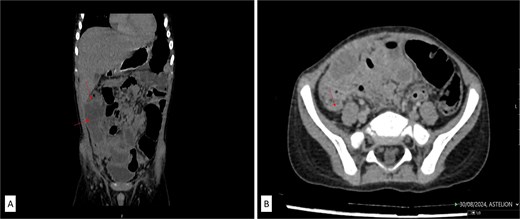
(A) Contrast-enhanced abdominal CT in coronal and axial scans showed an irregularly shaped mass in the right abdomen (labeled) in the form of extensive inflammatory mass which is in the close contact with the inferior liver surface, involving parts of ascending colon, cecum, and terminal ileum. (B) Retrocecal tubular structure (labeled) inseparable of dorsal wall of coecum which can correlate to the operative findings of second appendix.
Following fluid resuscitation and antibiotic administration, a laparotomy was performed via a McBurney’s incision. Intraoperatively, purulent peritonitis with fibrin-purulent membranes and a diffuse mass in the right abdomen were observed. The appendicular infiltrate and periappendicular abscess extended from the subhepatic region to the right pelvis (Fig. 1A and B). The surgical treatment of periappendicular abscess included the evacuation of all visible pus and exudates and conducted a thorough rinse with warm saline until the outflow was free of contaminants and the operation bed was clean. Despite technical challenges due to adhesive bowel loops, distorted anatomy, and inflammation affecting a wide area in the abdominal cavity—including the cranial position of the appendix on the cecal tenia above the ileocecal valve—we successfully performed an appendectomy, submitting the fragmented perforated appendix for histopathological analysis. During further exploration, a second, retrocecal appendix approximately 30 mm long was found, attached to the cecum without visible signs of inflammation, and was resected.
Histopathologic examination confirmed severe acute transmural appendicitis with thick fibrinopurulent deposits in one specimen (Fig. 2A and B) and secondary appendicitis with fibrinopurulent deposits on the serosa in the other (Fig. 2C and D). The patient had an uneventful postoperative recovery and was discharged in stable condition after 8 days. Intraoperative discovery of a duplicated vermiform appendix prompted a reevaluation of the preoperative CT scan, which revealed an additional appendix in a typical retrocecal position, measuring 24.1 mm in length, that was not initially detected (Fig. 3).
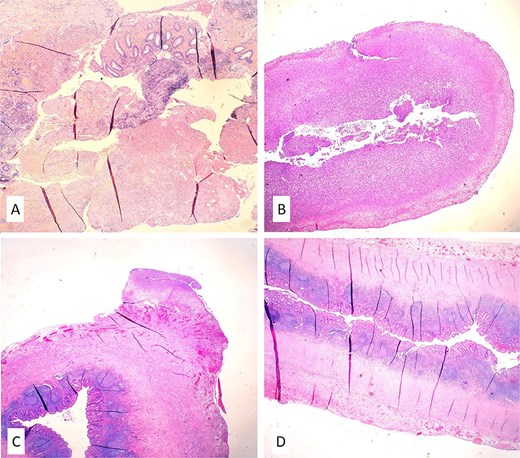
Histopathology confirmed a fragmentary finding of severe acute transmural appendicitis and thick fibrinopurulent deposits in one specimen (A, B) and secondary inflammation of appendiceal tissue with fibrinopurulent deposits on the serosa in the other (C, D) (hematoxylin and eosin/H&E/stains, magnification 10×).

Postoperatively analyzed preoperative contrast-enhanced sagittal abdominal CT scan detected a retrocecal 24.1 mm long tubular structure (a smaller second secondary inflamed appendix) with a transverse diameter of 5.6 mm and a wall thickness of 1.8 mm adherent to/inseparable from the dorsal wall of the cecum (labeled).
Discussion
This case report highlights the rare phenomenon of appendix duplication, a condition warranting attention due to its exceptional rarity and potential complications. Despite being recognized for over 130 years, < 200 cases have been reported in the literature [5]. Very few of these cases have involved AA, including the case presented here. The rarity is 2-fold in our instance, as it involves both a duplicated vermiform appendix and a very young patient—a 27-month-old toddler. In this age group, AA is particularly uncommon and challenging to diagnose promptly, as illustrated by the 9-day delay in referral for surgical consultation following the onset of symptoms.
The widely accepted modified Cave–Wallbridge classification system categorizes duplicated vermiform appendices into three types: Type A, Type B (subdivided into B1 and B2), and Type C [6, 7]. Type A duplication involves a single cecum with a partially duplicated appendix [6, 7]. Type B1 presents two distinct appendices on either side of the ileocecal valve. Type B2, or the tenia coli variant, features a retrocecal appendix originating from the convergence of the tenia coli, along with a smaller second appendix on the anterior tenia at a variable distance from the first [6, 7]. Type C includes two separate ceca, each with its appendix. Our case exemplifies the Type B2, or tenia coli variant, which is the most common form of duplication, accounting for ~37% of reported cases [8]. Type B2 is believed to arise from the persistence of a transient cecal protuberance during the sixth week of embryonic development. Unlike cases reported by Raja et al. and Rathore et al., where the inferior appendix was perforated and the duplicated appendix was inflamed and positioned superiorly along the anterior tenia [9, 10], our findings revealed a perforated anterior tenia coli-type appendix with a secondary, unchanged appendix located normally, incidentally identified during surgery.
Given that routine exploration of the ascending colon is generally not performed after clinically confirmed appendicitis originating at the cecum, the incidental discovery of a nonsymptomatic duplicated appendix during open surgery is highly unlikely. However, the improved visualization capabilities of laparoscopy enhance the likelihood of diagnosing related anomalies, such as vermiform appendix duplication. Findings like ours may support the practice of comprehensive distal exploration—examining the entire cecum and ascending colon—during appendicular surgeries, whether open or laparoscopic, akin to the common practice of proximal exploration to rule out Meckel's diverticulum.
In conclusion, a duplicated vermiform appendix presents a significant clinical challenge due to its rarity and potential complications. Awareness of this anomaly, especially Type B2 with one anatomically typical and one atypical appendix, underscores the importance of thorough distal and proximal exploration during appendicular surgery.
Author contributions
Z.Z., A.F., and A.J. treated the patient. M.B., N.I., and S.V. were involved in the diagnostics. Z.Z. and S.V. conceived this case study and drafted the manuscript. All authors read and approved the final version of the manuscript.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
Data are available from the corresponding authors on a reasonable request.



