-
PDF
- Split View
-
Views
-
Cite
Cite
Deepak Dev Vivekanandan, Lucas Canaan, Marshall Robaczewski, Mena Louis, Abigayle Wyer, John Clifton Hastings, Coronary-Pulmonary Artery Fistula and critical LAD stenosis: surgical ligation and revascularization, Journal of Surgical Case Reports, Volume 2024, Issue 12, December 2024, rjae775, https://doi.org/10.1093/jscr/rjae775
Close - Share Icon Share
Abstract
Coronary-pulmonary artery fistulas are rare congenital anomalies that can lead to significant clinical complications, especially when associated with coronary artery disease. We present a case of a 61-year-old male who presented with progressive dyspnea and chest discomfort. Imaging revealed a coronary-pulmonary artery fistula with 60% stenosis in the proximal left anterior descending artery. Due to the size and complexity of the fistula, along with the need for coronary artery revascularization, the patient underwent surgical ligation of the fistula combined with coronary artery bypass grafting. The patient had an uneventful recovery and was discharged on postoperative Day 6. At the 3-month follow-up, he reported a complete resolution of symptoms. This case illustrates the importance of surgical intervention in managing complex coronary fistulas with associated coronary artery disease and highlights the need for individualized treatment approaches.
Introduction
Coronary artery fistulas (CAFs) are rare vascular anomalies with an incidence of 0.9% in the general population [1]. These fistulas can either be congenital or acquired, leading to abnormal connections between coronary arteries and cardiac chambers or great vessels [2]. Coronary-pulmonary artery fistulas (CPFs) involve an abnormal communication between a coronary artery and the pulmonary artery, which can lead to symptoms like angina, dyspnea, and, if untreated, progressive heart failure [3]. The co-existence of coronary artery disease (CAD), especially significant stenosis in a major vessel, complicates management by increasing the risk of ischemia.
This case involves a 61-year-old male with both a CPF and critical left anterior descending (LAD) artery stenosis, successfully managed by open surgical ligation of the fistula and coronary artery bypass grafting (CABG) using the left internal mammary artery (LIMA) to the LAD.
Case report
A 61-year-old male with a history of hypertension, hyperlipidemia, and gastroesophageal reflux disease presented for outpatient evaluation following progressive shortness of breath and chest discomfort over the past few months. Symptoms began 7 years prior when he had experienced similar but less frequent episodes, which had recently increased in both frequency and severity. Coronary computed tomography angiography (CCTA) identified a CPF and significant LAD stenosis, prompting a referral for further evaluation and surgical intervention.
The CCTA revealed a well-developed CPF originating from the proximal LAD (Fig. 1), with moderate stenosis (50–70%) in the proximal LAD. The patient’s total coronary artery calcium score (Agatston score) was 672, indicative of advanced coronary atherosclerosis. Coronary angiography confirmed a diffuse 60% stenosis in the ostial and mid LAD, with mild luminal irregularities (<20%) in the left main coronary artery and right coronary artery (RCA). It also redemonstrated the presence of proximal LAD to pulmonary artery fistula (Fig. 2). No significant oxygen saturation step-up was observed, indicating the absence of a hemodynamically significant shunt.
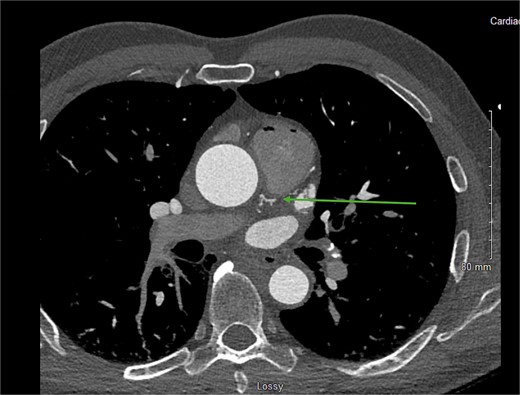
CCTA showing the CPF originating from the proximal LAD (green arrow).
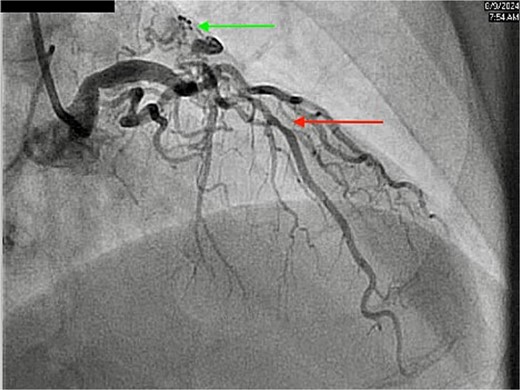
Coronary angiography showing diffuse stenosis in the LAD (red arrow) and CPF (green arrow).
The patient’s symptoms and diagnostic findings of critical LAD stenosis and the risk of ischemia due to the coronary-pulmonary fistula warranted surgical intervention. Given the size and complexity of the fistula, percutaneous closure was a feasible option, however since CABG was necessary to address the concomitant LAD stenosis plan was to proceed with surgical ligation.
A median sternotomy was performed, and the LIMA was harvested. The CPF was identified (Fig. 3) and ligated using three figure-of-eight sutures (Fig. 4), with additional clips applied to control flow through a secondary branch. The fistula was ligated at multiple location to decrease the chances of recanalization. Cardiopulmonary bypass (CPB) was initiated and LIMA-LAD anastomosis was performed. CPB was successfully weaned without complications. The patient was transferred to the cardiovascular intensive care unit in stable condition.
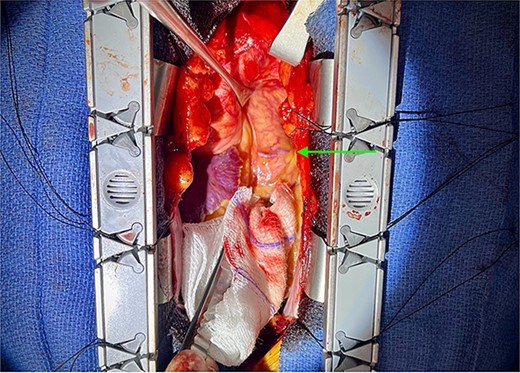
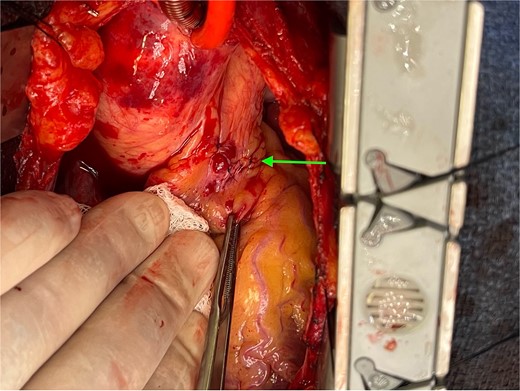
Ligation of coronary to pulmonary artery fistula with figure-of-eight sutures.
On postoperative Day 1 (POD), he remained hemodynamically stable with minimal chest tube drainage, and inotropes were discontinued. By POD2, the patient had been transferred to the step-down unit after being weaned off norepinephrine, and a low-dose beta-blocker was initiated. On POD3, a chest X-ray showed mild pulmonary edema and a small left pleural effusion, both managed with intravenous diuresis. The patient’s respiratory status improved with diuresis and ambulation. By POD4, his pacing wires were removed, and he was making steady progress. On POD6, patient was discharged home in good condition. The patient was started on long-term secondary prevention measures, including daily aspirin 81 mg and atorvastatin 40 mg, and was encouraged to continue lifestyle modifications to mitigate future cardiovascular risk.
At the 3-month follow-up, the patient reported resolution of chest pain and improvement in exercise tolerance.
Discussion
CPFs are rare but clinically significant conditions, especially when associated with CAD. CPFs create a left-to-right shunt that can lead to coronary steal syndrome, reducing myocardial perfusion and contributing to ischemia [4, 5]. This patient’s presentation with progressive dyspnea and chest pain was due to both the CPF and significant LAD stenosis. Left untreated, the combination of coronary steal and critical LAD stenosis could have led to severe ischemic events or heart failure.
Imaging studies, including CCTA and coronary angiography, were instrumental in identifying the fistula’s anatomy and confirming the severity of the LAD stenosis. The patient’s elevated coronary artery calcium score (Agatston score) of 672, placing him in the 96th percentile based on the Multi-Ethnic Study of Atherosclerosis database, which compares coronary artery calcium scores across different age and gender groups indicated a significant burden of atherosclerotic disease [6], further supporting the decision to pursue surgical revascularization.
In this case of a CPF with concomitant critical LAD stenosis, surgical ligation was chosen due to the size and complexity of the fistula, as well as the need for CABG to address the patient’s significant CAD. While catheter-based closure is often the preferred option for smaller, uncomplicated fistulas [7], it was deemed unsuitable here given the large, high-flow nature of the fistula and the requirement for simultaneous revascularization. Surgical ligation remains the optimal choice for large or complex fistulas, especially when additional conditions, such as CAD requiring CABG, must be addressed [8]. The successful combination of LIMA-LAD bypass and ligation of the fistula at multiple locations ensured both adequate revascularization and complete closure of the abnormal connection, resulting in a favorable outcome for the patient.
The patient’s postoperative course was uncomplicated, with early resolution of symptoms and no significant complications. Surgical ligation of the fistula was successful, and using LIMA for LAD bypass ensured long-term patency, reducing the risk of recurrent ischemia. The patient’s management was further enhanced by initiating secondary prevention measures, including antiplatelet therapy and lipid-lowering agents.
Conclusion
This case illustrates the successful management of a CPF with concomitant LAD stenosis through open surgical ligation and CABG. The combination of significant CAD and a large coronary fistula required a multidisciplinary approach, with surgery offering definitive treatment. The patient’s postoperative recovery and long-term outcomes were favorable, underscoring the importance of timely diagnosis, individualized treatment, and ongoing follow-up in managing complex coronary anomalies.
Author contributions
Deepak Dev Vivekanandan: Conceived the Case Report, performed the Literature Review, and was the primary author of the manuscript; Coordinated clinical data collection and imaging analysis. Lucas Canaan: Assisted with clinical data interpretation, intraoperative imaging acquisition, and manuscript editing. Marshall Robaczewski: Contributed to the surgical case management, provided intraoperative details, and critically reviewed the manuscript. Mena Louis: Contributed to data collection and preparation of the Discussion section. Abigayle Wyer: Assisted with the Literature Review, References, and preparation of the Abstract and Introduction sections. John Clifton Hastings III: Supervised the project and provided critical revisions to the manuscript, ensuring its accuracy and clinical relevance.
Conflict of interest statement
None declared.
Funding
None declared.
References
Lee KY, Chang K, Lee JM, et al.



