-
PDF
- Split View
-
Views
-
Cite
Cite
Andrej Nikolovski, Klaudia Gjinoska, Zhivorad Kocevski, Emil Stoicovski, Zan Mitrev, Giant (complex) inguinal hernia in female patient left untreated for 40 years: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae734, https://doi.org/10.1093/jscr/rjae734
Close - Share Icon Share
Abstract
A giant inguinal hernia is a rare clinical presentation in patients refusing hernia repair for different reasons during a long period. The appearance is remarkable, and the preoperative preparation and the surgery itself might be challenging. They can present in an emergency (hernia incarceration) or elective setting. Most of the patients are male, but exclusions exist. This is a rare case of a female patient with a giant inguinal hernia left untreated for 40 years.
Introduction
If left untreated, an inguinal hernia can grow and cause serious impairment of everyday activities. This is mostly seen in male patients [1]. However, inguinal hernia is the most common type of hernia in females, but it rarely reaches gigantic proportions [2]. This kind of presentation in female patients is extremely rare and only a few cases are reported in the literature. We present a case of a long-lasting inguinal hernia in a female patient left untreated for 40 years. The patient finally decided to be operated on due to reduced quality of life. Written informed consent was obtained from the patient for publication of this case report.
Case report
A 64-year-old female patient presented in the outpatient clinic with a complaint of a long-lasting hernia (~40 years) on the anterior abdominal wall. Two birth deliveries were self-reported (only the first with Caesarean section). Routinely treated and controlled hypertension was the only reported comorbidity. The patient noticed that the previously reducible hernia ‘won’t get back into the abdomen’ in the past 2 years. Due to the reduced quality of life and the bad aesthetic appearance, the patient decided to undergo an elective hernia repair procedure.
The physical exam revealed an irreducible giant abdominal wall hernia (mostly on the left lower part of the abdominal wall). Due to irreducibility, the hernia defect was not accessible for palpation and estimation. A previous low midline laparotomy scar was visible (Fig. 1A and B). A computerized tomography diagnostic scan of the abdomen was performed. It presented with a hernia defect (65 mm in width) in the left inguinal region (Fig. 2A–C).

Clinical appearance of the hernia (A – view from below, B – frontal view).
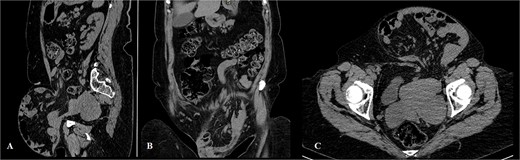
Computerized tomography of the abdomen (A – sagittal scan, B – coronal scan, C – axial scan).
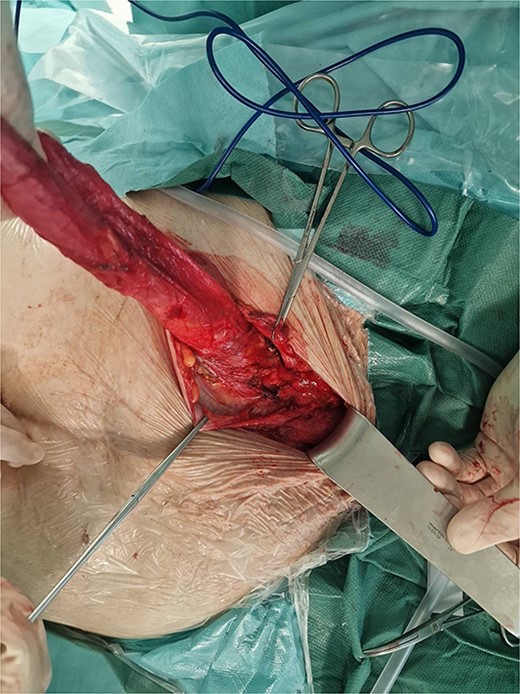
Surgery was planned with general anesthesia. Preoperative bowel preparation was not conducted in this case. The patient was set in a slight Trendelenburg position. As soon as an intravenous muscle relaxant was given as a part of the general anesthesia protocol, successful manual hernia reduction was performed and the defect became easily detectable. A left inguinal approach was decided to be performed. The hernia sac was visible after the left inguinal canal was opened, and its dissection was not technically demanding. The left uterine round ligament was resected and the hernia defect was defined as a direct (Fig. 3). The hernia sac was reduced and a standard Lichtenstein repair followed. A plastic surgeon excised the skin that used to cover the giant hernia. A subcutaneous suction drain was inserted (Fig. 4). Operative time was 75 minutes. In the postoperative period, local wound cellulitis with fever occurred and was treated with intravenous antibiotics (5 days of duration) and daily wound dressings. The hospital stay was 5 days.

Discussion
Inguinal hernia is the most common anterior wall hernia in both genders of whom 10% are female patients. According to this, inguinal hernia repair is a commonly performed procedure [3]. The term ‘complex inguinal hernia’ refers to hernias with large defects, multiple recurrences, hernia bilaterality, and large to giant hernia sac existence as in this case [4].
Inguinoscrotal presentation in male patients with an unrepaired long-lasting hernia is clinically remarkable [5], but it is not exclusive to the male gender. The literature review led us to conclude that giant inguinal hernias in female patients are reported in just two cases, thus making this report the third one (Table 1).
| Reference number . | Author/year . | Gender . | Age (years) . | Hernia side . | Duration of clinical presentation (years) . | Presentation at surgery . | Type of hernia repair . |
|---|---|---|---|---|---|---|---|
| [6] | Cervantes et al./2020 | F | 85 | Right | 25 | Elective | Mesh repair (technique not specified) |
| [7] | Rossi et al./2017 | F | 67 | Right | 10 | Emergency | Not reported |
| This case report | Nikolovski et al./2024 | F | 64 | Left | 40 | Elective | Lichtenstein repair |
| Reference number . | Author/year . | Gender . | Age (years) . | Hernia side . | Duration of clinical presentation (years) . | Presentation at surgery . | Type of hernia repair . |
|---|---|---|---|---|---|---|---|
| [6] | Cervantes et al./2020 | F | 85 | Right | 25 | Elective | Mesh repair (technique not specified) |
| [7] | Rossi et al./2017 | F | 67 | Right | 10 | Emergency | Not reported |
| This case report | Nikolovski et al./2024 | F | 64 | Left | 40 | Elective | Lichtenstein repair |
| Reference number . | Author/year . | Gender . | Age (years) . | Hernia side . | Duration of clinical presentation (years) . | Presentation at surgery . | Type of hernia repair . |
|---|---|---|---|---|---|---|---|
| [6] | Cervantes et al./2020 | F | 85 | Right | 25 | Elective | Mesh repair (technique not specified) |
| [7] | Rossi et al./2017 | F | 67 | Right | 10 | Emergency | Not reported |
| This case report | Nikolovski et al./2024 | F | 64 | Left | 40 | Elective | Lichtenstein repair |
| Reference number . | Author/year . | Gender . | Age (years) . | Hernia side . | Duration of clinical presentation (years) . | Presentation at surgery . | Type of hernia repair . |
|---|---|---|---|---|---|---|---|
| [6] | Cervantes et al./2020 | F | 85 | Right | 25 | Elective | Mesh repair (technique not specified) |
| [7] | Rossi et al./2017 | F | 67 | Right | 10 | Emergency | Not reported |
| This case report | Nikolovski et al./2024 | F | 64 | Left | 40 | Elective | Lichtenstein repair |
According to the classification of Trakarnsagna et al., these hernias are classified into three types:
- Type 1 (hernia sac descends below the mid-thigh but above an imaginary horizontal line midway between mid-thigh and superior patellar border);
- Type 2 (hernia sac descends below the imaginary horizontal line midway between mid-thigh and superior patellar border, and not extending beyond the superior patellar border and.
-Type 3 (hernia sac descends or extends beyond the superior patellar border) [8].
A proposal for modification of this classification was given by Oyewale and Ariwoola where not only the hernia sac extension is considered, but also the presence of loss of domain of the abdominal cavity which might influence the postoperative outcome in terms of abdominal compartment syndrome development [9]. In this case report, the hernia was classified as type 2 according to Trakarnsagna and type 2a according to the proposed modification by Oyewale and Ariwoola.
The surgical procedure for the repair of a giant inguinal hernia differs from region to region. The majority of the patients from sub-Saharan Africa were reported to be treated with modified Bassini and Nylon Darn repair [9]. In developed countries, different tension-free techniques are used [10]. The open preperitoneal repair (Stoppa and Wantz procedure) is also reported to be used for these complex hernias [4]. Last but not least, the standard Lichtenstein repair for inguinal hernia is an effective and simple method, as in this case.
Postoperative hematoma in the scrotum is a common adverse event in male patients treated for giant inguinal hernia [8]. Parallel to that, in female patients, hematoma occurrence in great labia might occur. The major postoperative complications include intraabdominal hypertension followed by abdominal compartment syndrome, cardiorespiratory complications, and the need for elective postoperative ventilation [11].
Conclusion
Regardless of the patient's level of education, the existing fear of surgery, and treatment delay, part of them eventually will be operated upon in elective or emergency circumstances. This case reports a successful treatment of a giant inguinal hernia in a female patient that postponed inguinal hernia repair for 40 years.
Conflict of interest statement
None declared.
Funding
None declared.



