-
PDF
- Split View
-
Views
-
Cite
Cite
Haley Bayne, Richard Q Vuong, Shubhneet Bal, Jeffrey West, Anya Laibangyang, David Doo, Obturator nerve schwannoma: a case report and review of the robotic literature, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae694, https://doi.org/10.1093/jscr/rjae694
Close - Share Icon Share
Abstract
Obturator schwannomas are rare and often misdiagnosed as intraperitoneal pelvic masses. The optimal surgical approach for their resection is unclear. This study presents a case demonstrating the safe use of robotics for resecting a benign pelvic schwannoma and reviews the literature on robotic cases. Here, a 40-year-old woman with right lower quadrant pain underwent imaging, revealing a 4.6 × 3.3 × 3.6 cm pelvic mass. She had a robotic-assisted laparoscopic excision, with pathology confirming a benign schwannoma. Complete tumor resection is the gold standard. The use of minimally invasive robotic-assisted surgery is increasing due to improved visualization, efficient movement, and safety, making it a viable option for resecting obturator schwannomas.
Introduction
Schwannomas are rare peripheral nerve sheath tumors that arise from Schwann cells of the epineurium. They can present in any age group and are most commonly found in the head, with a lower incidence in the retroperitoneum (~3% incidence) [1]. Even rarer are cases of schwannomas seen arising from the obturator nerve, with only 19 cases reported from 1988 to April 2024 [2–7]. Surgical removal is the primary treatment approach, as slow-growing schwannomas typically do not respond well to radiation or chemotherapy [8]. However, some cases have reported post-operative permanent neurological deficits when resecting obturator schwannomas due to the amount of excised nerve tissue [8]. This report describes the use of robotics in resecting an obturator nerve schwannoma and discusses its advantages for lesions requiring precise dissection in anatomically complex areas. Additionally, we review all reports of obturator schwannomas treated with robotic-assisted laparoscopy.
Materials and methods
This study describes a single case report of a 40-year-old female patient with an obturator nerve schwannoma resected using robotic-assisted laparoscopy. A retrospective review of imaging, surgical approach, and histopathology was performed. Outcomes were assessed by examining post-operative recovery and neurological function. Additionally, a literature review was conducted to compare the effectiveness and safety of robotic-assisted resection for obturator nerve schwannomas. Data analysis focused on procedural outcomes, including operative success and post-operative complications.
Results
A 40-year-old P4 woman, with a past medical history of celiac disease, hypothyroidism, and varicose veins, presented with intermittent right lower quadrant pain that occurs 1–2 times per week for over a year, exacerbated by sexual activity. She denied any changes in urinary habits, bowel movements, or early satiety. Transvaginal ultrasound measured the right ovary at 4.5 × 4.3 × 3.8 cm with a complex cyst measuring 4.6 × 3.3 × 3.6 cm and containing several cystic spaces with low-level internal echoes. Prior imaging showed the cyst had been slowly growing with dimensions from one year ago (Fig. 1) at 4.2 × 3.7 × 3.6 cm and three years ago at 2.8 × 2.1 × 1.6 cm. Magnetic resonance imaging (MRI) of the pelvis (Fig. 2) revealed a complex solid and cystic retroperitoneal mass abutting the right external iliac vessel. Although the patient reported only intermittent pain at this time, the continued increase in size was concerning for a potential neoplasm. Although malignancy could not be ruled out, the absence of elevated tumor markers like CA-125 suggested a benign finding. The decision was made to proceed with diagnostic laparoscopy for suspicion of growing ovarian lesion. The diagnostic laparoscopy successfully visualized normal-appearing ovaries and fallopian tubes bilaterally. However, a 4-cm firm, circumferential retroperitoneal mass within the right broad ligament along the sidewall of the pelvis was discovered. Due to the mass’s location and proximity to the right ureter and uterine artery, dissection was not attempted in favor of conservative treatment and monitoring.
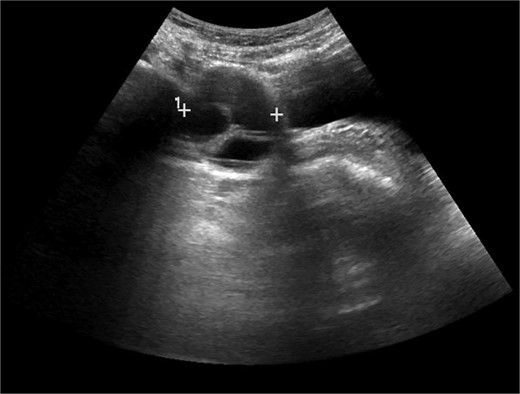
Transvaginal ultrasound image of right adnexa. Cystic structure with the measurement 4.2 × 3.7 × 3.6 cm at the time of imaging.
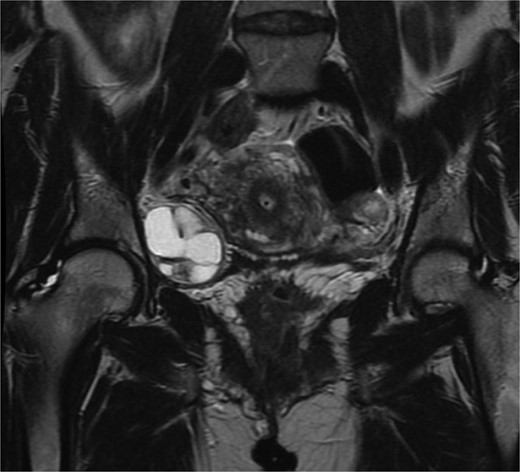
Coronal magnetic resonance imaging of the pelvis with contrast. Complex solid and cystic retroperitoneal mass abutting the right external iliac vessel, 4.4 cm × 4.0 cm × 3.8 cm in measurement.
A few weeks later, the patient returned to the clinic with worsening pain now increased to 1–2 times weekly, lasting up to 2 hours. The decision was made to perform robot-assisted laparoscopy for pelvic mass resection and possible salpingo-oophorectomy. The patient consented and underwent a diagnostic laparoscopy, as well as a robotic assisted pelvic and retroperitoneal mass excision. During the procedure, the mass was nested deep in the right broad ligament adjacent to the sidewall in the retroperitoneal space. Careful dissection revealed a 4.6 × 3.3 × 3.6 cm mass arising from the right obturator nerve. The mass was resected with no complications, and the patient was discharged to home later that day. The day after the procedure, the patient expressed concern for right leg sensory and motor deficits, which was thought to be related to inflammation. Physical exam remained normal. Patient was referred to physical therapy and later reported an improvement in symptoms. On last follow up, 3 years after the procedure, the patient continues to remain free of sensory or motor deficits.
Gross examination and cut sections revealed fragments of tan–white to tan–yellow tissue with some areas of hemorrhage measuring from 1.1 to 3.6 cm in the greatest dimension. Histopathological examination of the excised mass confirmed the diagnosis of a retroperitoneal schwannoma, characterized by S100 positivity (Fig. 3) and degenerative changes, including hemorrhage, hemosiderin, and cystic degeneration (Fig. 4), nuclear atypia (Fig. 5), and perivascular hyalinization (Fig. 6).
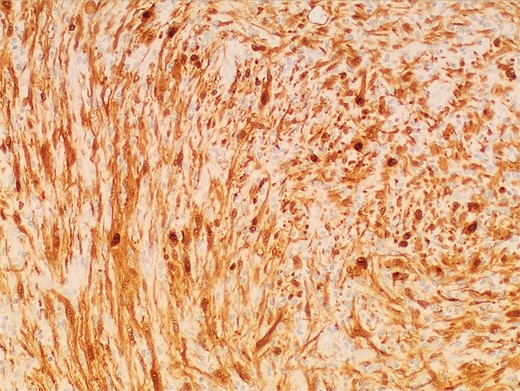
Photomicrograph of diagnostic histopathology showing strong and diffuse S100 immunohistochemical stain uptake by lesional cells.
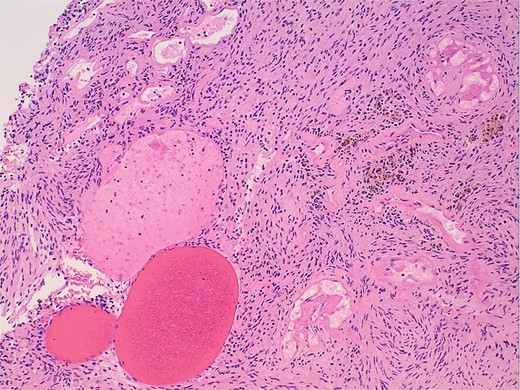
Photomicrograph of diagnostic histopathology showing cystic degeneration and hemorrhage with hemosiderin laden macrophages.
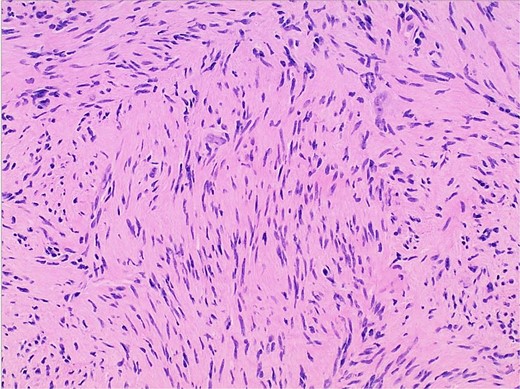
Photomicrograph of diagnostic histopathology showing elongated wavy cells with tapered ends of nuclei and modest amount of cytoplasm.
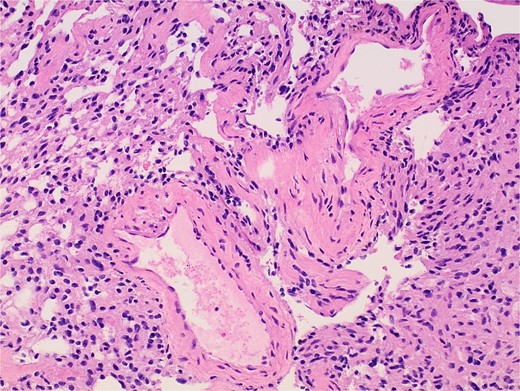
Photomicrograph of diagnostic histopathology showing thickened blood vessel walls with hyalinization.
Discussion
Obturator nerve schwannomas are a rare entity categorized under retroperitoneal schwannomas, which boast an incidence rate of 3% of all schwannomas. Because of their infrequency and challenging preoperative presentation, the obturator schwannoma in our case was first managed conservatively as an ovarian cyst until more concerning features arose (i.e. interval increase in size and persistent pain). The proximity to major structures and need for precise dissection led to the decision to utilize robotic-assisted laparoscopy to completely resect the schwannoma with no lasting neurological deficits. This is especially encouraging as prior cases of non-robotic laparoscopic management of obturator nerve schwannomas have reported permanent postoperative neurological deficits [8].
The use of robotics in resecting obturator nerve schwannomas remains limited but does show promise. As our case has shown, robotics may provide a way to excise obturator schwannomas while preserving the integrity of the nerve. In fact, the four reports of robotic-assisted laparoscopic resection of obturator schwannomas reported no permanent postoperative neurological complications (Table 1) [6–7, 9–10]. Even in instances where patients experienced neural injury, they ultimately recovered without issues in daily activities [9], similar to this report. Contrastingly, some patients with obturator nerve schwannomas (1/3 of patients within an 11-year span at one hospital) suffered permanent neurologic deficits following laparoscopic resection [4]. Furthermore, robotic surgery offers an enhanced postoperative recovery for patients with a presumed shorter length of stay post-operatively in hospital settings [11]. Some limited data has suggested that the earlier return to normal activities and shorter hospitalizations can offset the initial costs and training period needed to obtain expertise in gynecologic surgeries, including retroperitoneal schwannomas [12, 13].
| Author, Year . | Patient assigned gender at birth, age . | Clinical Aspects . | Imaging Findings . | Treatment . | Histological Examination . | Follow-Up . |
|---|---|---|---|---|---|---|
| Bulisani, 2024 | 51-year-old female | Left pelvic pain ×3 months, normal physical exam. | CT abdomen and pelvis showed pelvic lesion in left iliac vessels, hypodense contrast enhancement measuring 4.6 × 3.4 cm. MRI showed extraperitoneal lesion located medially and inferiorly to left external iliac vessels, 4.9 × 3.7 cm. | Surgical resection of tumor due to suspected obturator nerve schwannoma. Robotic surgery was elected to decrease risk for postoperative negative outcomes. | Pedicled, encapsulated neoplasia of 6.8 × 5.2 × 2.9 cm. No necrosis or mitotic areas but hyalinization present. Diffuse S100 staining confirms presence of schwannoma. | NA |
| Chopra, 2017 | 46-year-old male | Left pelvic pain, sharp in nature and radiates down. Patient denies weight loss, fever, loss of appetite. Physical exam shows palpable pelvic mass. | Pelvic ultrasound demonstrated complex cystic mass, unclear etiology, measuring 6.0 × 4.9 × 4.9 cm and located along the left lateral pelvic sidewall. | Patient agreed to undergo robotic excision due its location. Tumor was found to be within the obturator nerve, so 5–6 cm resection of the obturator nerve was undertaken. | Negative for CA 125, alpha fetoprotein, lactate dehydrogenase, beta-human chorionic gonadotropin. Tumor exhibited myxoid, edematous and cystic features. Stains positive for S100. | Discharged on postoperative day 2. No sensory or motor deficit complaints. |
| Liakos, 2020 | 58-year-old male | Inguinal pain radiating to the inner surface of the left thigh, independent of event. | Ultrasound showed no abnormal findings. Multiparametric MRI of the prostate showed thickening of the left obturator nerve. | Robot assisted prostatectomy due to suspected prostate mass. During associated left pelvic lymphadenectomy, a mass measuring 0.9 × 0.5 × 0.3 cm was found in the middle intrapelvic portion of the left obturator nerve. | Yellow mass noted on gross pathology. Histology showed cystic architecture and tissue consistent with a benign schwannoma. | Immediately postoperatively, the patient experienced loss of sensation on left medial thigh, but this was resolved by time of discharge. No other neurological deficits noted. |
| Perrin, 2017 | 27-year-old male | Incidental finding on abdominal ultrasonography for benign hematuria. Asymptomatic for pain. | Ultrasound showed stones in the kidney with no hydronephrosis. Contrast enhanced CT showed a solid mass measuring 4.1 × 3.8 × 4.5 cm in the right side of the pelvic cavity, between the internal and external iliac vessels. | Robotic procedure performed, locating tumor in retroperitoneal space behind right external iliac artery and up to right ureter, in obturator foramen. | Serum carcinoembryonic antigen, CA 19–9 and prostate specific antigen were not overexpressed. CT guided biopsy confirmed diagnosis of benign schwannoma prior to operation. After operation, specimen was 5.7 × 4.2 cm hard enveloped mass. Whorls and interlacing spindle cells noted on histopathology. Cells stained positive for S100 protein. | Patient discharged on postoperative day 3. No neurological deficits noted postoperatively. |
| Author, Year . | Patient assigned gender at birth, age . | Clinical Aspects . | Imaging Findings . | Treatment . | Histological Examination . | Follow-Up . |
|---|---|---|---|---|---|---|
| Bulisani, 2024 | 51-year-old female | Left pelvic pain ×3 months, normal physical exam. | CT abdomen and pelvis showed pelvic lesion in left iliac vessels, hypodense contrast enhancement measuring 4.6 × 3.4 cm. MRI showed extraperitoneal lesion located medially and inferiorly to left external iliac vessels, 4.9 × 3.7 cm. | Surgical resection of tumor due to suspected obturator nerve schwannoma. Robotic surgery was elected to decrease risk for postoperative negative outcomes. | Pedicled, encapsulated neoplasia of 6.8 × 5.2 × 2.9 cm. No necrosis or mitotic areas but hyalinization present. Diffuse S100 staining confirms presence of schwannoma. | NA |
| Chopra, 2017 | 46-year-old male | Left pelvic pain, sharp in nature and radiates down. Patient denies weight loss, fever, loss of appetite. Physical exam shows palpable pelvic mass. | Pelvic ultrasound demonstrated complex cystic mass, unclear etiology, measuring 6.0 × 4.9 × 4.9 cm and located along the left lateral pelvic sidewall. | Patient agreed to undergo robotic excision due its location. Tumor was found to be within the obturator nerve, so 5–6 cm resection of the obturator nerve was undertaken. | Negative for CA 125, alpha fetoprotein, lactate dehydrogenase, beta-human chorionic gonadotropin. Tumor exhibited myxoid, edematous and cystic features. Stains positive for S100. | Discharged on postoperative day 2. No sensory or motor deficit complaints. |
| Liakos, 2020 | 58-year-old male | Inguinal pain radiating to the inner surface of the left thigh, independent of event. | Ultrasound showed no abnormal findings. Multiparametric MRI of the prostate showed thickening of the left obturator nerve. | Robot assisted prostatectomy due to suspected prostate mass. During associated left pelvic lymphadenectomy, a mass measuring 0.9 × 0.5 × 0.3 cm was found in the middle intrapelvic portion of the left obturator nerve. | Yellow mass noted on gross pathology. Histology showed cystic architecture and tissue consistent with a benign schwannoma. | Immediately postoperatively, the patient experienced loss of sensation on left medial thigh, but this was resolved by time of discharge. No other neurological deficits noted. |
| Perrin, 2017 | 27-year-old male | Incidental finding on abdominal ultrasonography for benign hematuria. Asymptomatic for pain. | Ultrasound showed stones in the kidney with no hydronephrosis. Contrast enhanced CT showed a solid mass measuring 4.1 × 3.8 × 4.5 cm in the right side of the pelvic cavity, between the internal and external iliac vessels. | Robotic procedure performed, locating tumor in retroperitoneal space behind right external iliac artery and up to right ureter, in obturator foramen. | Serum carcinoembryonic antigen, CA 19–9 and prostate specific antigen were not overexpressed. CT guided biopsy confirmed diagnosis of benign schwannoma prior to operation. After operation, specimen was 5.7 × 4.2 cm hard enveloped mass. Whorls and interlacing spindle cells noted on histopathology. Cells stained positive for S100 protein. | Patient discharged on postoperative day 3. No neurological deficits noted postoperatively. |
| Author, Year . | Patient assigned gender at birth, age . | Clinical Aspects . | Imaging Findings . | Treatment . | Histological Examination . | Follow-Up . |
|---|---|---|---|---|---|---|
| Bulisani, 2024 | 51-year-old female | Left pelvic pain ×3 months, normal physical exam. | CT abdomen and pelvis showed pelvic lesion in left iliac vessels, hypodense contrast enhancement measuring 4.6 × 3.4 cm. MRI showed extraperitoneal lesion located medially and inferiorly to left external iliac vessels, 4.9 × 3.7 cm. | Surgical resection of tumor due to suspected obturator nerve schwannoma. Robotic surgery was elected to decrease risk for postoperative negative outcomes. | Pedicled, encapsulated neoplasia of 6.8 × 5.2 × 2.9 cm. No necrosis or mitotic areas but hyalinization present. Diffuse S100 staining confirms presence of schwannoma. | NA |
| Chopra, 2017 | 46-year-old male | Left pelvic pain, sharp in nature and radiates down. Patient denies weight loss, fever, loss of appetite. Physical exam shows palpable pelvic mass. | Pelvic ultrasound demonstrated complex cystic mass, unclear etiology, measuring 6.0 × 4.9 × 4.9 cm and located along the left lateral pelvic sidewall. | Patient agreed to undergo robotic excision due its location. Tumor was found to be within the obturator nerve, so 5–6 cm resection of the obturator nerve was undertaken. | Negative for CA 125, alpha fetoprotein, lactate dehydrogenase, beta-human chorionic gonadotropin. Tumor exhibited myxoid, edematous and cystic features. Stains positive for S100. | Discharged on postoperative day 2. No sensory or motor deficit complaints. |
| Liakos, 2020 | 58-year-old male | Inguinal pain radiating to the inner surface of the left thigh, independent of event. | Ultrasound showed no abnormal findings. Multiparametric MRI of the prostate showed thickening of the left obturator nerve. | Robot assisted prostatectomy due to suspected prostate mass. During associated left pelvic lymphadenectomy, a mass measuring 0.9 × 0.5 × 0.3 cm was found in the middle intrapelvic portion of the left obturator nerve. | Yellow mass noted on gross pathology. Histology showed cystic architecture and tissue consistent with a benign schwannoma. | Immediately postoperatively, the patient experienced loss of sensation on left medial thigh, but this was resolved by time of discharge. No other neurological deficits noted. |
| Perrin, 2017 | 27-year-old male | Incidental finding on abdominal ultrasonography for benign hematuria. Asymptomatic for pain. | Ultrasound showed stones in the kidney with no hydronephrosis. Contrast enhanced CT showed a solid mass measuring 4.1 × 3.8 × 4.5 cm in the right side of the pelvic cavity, between the internal and external iliac vessels. | Robotic procedure performed, locating tumor in retroperitoneal space behind right external iliac artery and up to right ureter, in obturator foramen. | Serum carcinoembryonic antigen, CA 19–9 and prostate specific antigen were not overexpressed. CT guided biopsy confirmed diagnosis of benign schwannoma prior to operation. After operation, specimen was 5.7 × 4.2 cm hard enveloped mass. Whorls and interlacing spindle cells noted on histopathology. Cells stained positive for S100 protein. | Patient discharged on postoperative day 3. No neurological deficits noted postoperatively. |
| Author, Year . | Patient assigned gender at birth, age . | Clinical Aspects . | Imaging Findings . | Treatment . | Histological Examination . | Follow-Up . |
|---|---|---|---|---|---|---|
| Bulisani, 2024 | 51-year-old female | Left pelvic pain ×3 months, normal physical exam. | CT abdomen and pelvis showed pelvic lesion in left iliac vessels, hypodense contrast enhancement measuring 4.6 × 3.4 cm. MRI showed extraperitoneal lesion located medially and inferiorly to left external iliac vessels, 4.9 × 3.7 cm. | Surgical resection of tumor due to suspected obturator nerve schwannoma. Robotic surgery was elected to decrease risk for postoperative negative outcomes. | Pedicled, encapsulated neoplasia of 6.8 × 5.2 × 2.9 cm. No necrosis or mitotic areas but hyalinization present. Diffuse S100 staining confirms presence of schwannoma. | NA |
| Chopra, 2017 | 46-year-old male | Left pelvic pain, sharp in nature and radiates down. Patient denies weight loss, fever, loss of appetite. Physical exam shows palpable pelvic mass. | Pelvic ultrasound demonstrated complex cystic mass, unclear etiology, measuring 6.0 × 4.9 × 4.9 cm and located along the left lateral pelvic sidewall. | Patient agreed to undergo robotic excision due its location. Tumor was found to be within the obturator nerve, so 5–6 cm resection of the obturator nerve was undertaken. | Negative for CA 125, alpha fetoprotein, lactate dehydrogenase, beta-human chorionic gonadotropin. Tumor exhibited myxoid, edematous and cystic features. Stains positive for S100. | Discharged on postoperative day 2. No sensory or motor deficit complaints. |
| Liakos, 2020 | 58-year-old male | Inguinal pain radiating to the inner surface of the left thigh, independent of event. | Ultrasound showed no abnormal findings. Multiparametric MRI of the prostate showed thickening of the left obturator nerve. | Robot assisted prostatectomy due to suspected prostate mass. During associated left pelvic lymphadenectomy, a mass measuring 0.9 × 0.5 × 0.3 cm was found in the middle intrapelvic portion of the left obturator nerve. | Yellow mass noted on gross pathology. Histology showed cystic architecture and tissue consistent with a benign schwannoma. | Immediately postoperatively, the patient experienced loss of sensation on left medial thigh, but this was resolved by time of discharge. No other neurological deficits noted. |
| Perrin, 2017 | 27-year-old male | Incidental finding on abdominal ultrasonography for benign hematuria. Asymptomatic for pain. | Ultrasound showed stones in the kidney with no hydronephrosis. Contrast enhanced CT showed a solid mass measuring 4.1 × 3.8 × 4.5 cm in the right side of the pelvic cavity, between the internal and external iliac vessels. | Robotic procedure performed, locating tumor in retroperitoneal space behind right external iliac artery and up to right ureter, in obturator foramen. | Serum carcinoembryonic antigen, CA 19–9 and prostate specific antigen were not overexpressed. CT guided biopsy confirmed diagnosis of benign schwannoma prior to operation. After operation, specimen was 5.7 × 4.2 cm hard enveloped mass. Whorls and interlacing spindle cells noted on histopathology. Cells stained positive for S100 protein. | Patient discharged on postoperative day 3. No neurological deficits noted postoperatively. |
Diagnosing schwannomas early poses challenges, as they often begin asymptomatically or with nonspecific signs [8, 14]. Preoperative diagnoses most commonly are determined to be of unclear etiology [7, 10]. Definitive diagnosis of schwannomas requires histopathological examination with S100 protein positivity [11, 15]. Malignant transformation of retroperitoneal schwannomas is extremely rare [11]. As such, patients with small, asymptomatic obturator nerve schwannomas can opt for an elective surgical approach [8]. Shared decision-making should be followed in patients who do undergo surgery as the risk of lasting neurological deficits is influenced by the amount of tissue being resected, type of laparoscopic platform used by the surgeon, and follow-up with physiotherapy.
Conclusions
This case highlights the potential advantages of robotic-assisted laparoscopy for the resection of obturator nerve schwannomas, particularly in anatomically complex regions where precise dissection is critical to preserving nerve function. Our case and literature review suggest that robotics may offer enhanced control, leading to successful tumor removal with minimal neurological compromise. As observed in this case and in a review of similar reports, robotic-assisted techniques can reduce the risk of permanent postoperative deficits commonly associated with traditional approaches. Given the rarity of obturator nerve schwannomas, further studies are warranted to establish the role of robotic surgery in optimizing outcomes and minimizing recovery time for patients with this challenging diagnosis.
Author contributions
HNB contributed to the literature review, as well as the design and drafting, of the manuscript. RQV participated in the manuscript design and revisions. SB and JW provided imaging and pathology data. AL and DD offered critical revisions and assisted with data interpretation. All authors reviewed, revised, and approved the final manuscript.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
Data supporting the findings of this study are available within the article. Additional information, including imaging and histopathology details, may be provided by the corresponding author upon reasonable request. Due to patient privacy concerns, some data may be restricted.



