-
PDF
- Split View
-
Views
-
Cite
Cite
Matthew Binks, Femi E Ayeni, Senarath Edirimanne, Farid Meybodi, Goldilocks mastectomy with immediate reconstruction: enhancing aesthetic outcomes and preserving nipple complex, Journal of Surgical Case Reports, Volume 2024, Issue 11, November 2024, rjae682, https://doi.org/10.1093/jscr/rjae682
Close - Share Icon Share
Abstract
Despite significant advancements in early breast cancer detection, mastectomy remains a crucial treatment option for some patients. Immediate breast reconstruction post-mastectomy has emerged as an ideal procedure to minimize physical and psychosocial patient impacts, striving for improved cosmetic results. The “enhanced “Goldilocks mastectomy technique, characterized by nipple preservation or grafting and utilizing the fifth perforator anatomy, offers a sound approach to reconstruction in comorbid and large-breasted patients. This paper discusses the advantages, disadvantages, and real-world application of Goldilocks mastectomy in enhancing breast reconstruction outcomes and meeting patients' diverse needs.
Introduction
Mastectomy remains a vital tool in the management of select patients diagnosed with breast cancer. Immediate reconstruction of the breast mound following mastectomy offers many advantages to the patient by restoring form and function and improving their psychological, social and sexual outcomes [1–3].
Breast cancer is increasingly being diagnosed in patients of older age and with higher body mass index (BMI). With these and additional comorbidities, such as diabetes and cigarette smoking, comes a significant increase in the surgical and medical risks associated with post mastectomy reconstruction [4–9].
Described in 2012, the Goldilocks mastectomy uses a patients’ redundant subcutaneous tissue overlying the breast to recreate a smaller breast mound [10]. By avoiding prosthetic tissue and distant extramammary tissue transfer, the procedure has proven effective in high risk, obese patients [10, 11]. Nipple grafting has emerged as a viable enhancement of the Goldilocks mastectomy [12, 13].
Case Presentation
Case 1
PK, a 65-year-old woman, presented with macromastia and associated neck pain, back pain and skin irritation in the inframammary fold (Fig. 1). Whilst PK had multiple breast and other cancers on either side of her family, she did not have any personal history of breast cancer nor a known gene mutation. PK had previously developed secondary diabetes mellitus following steroid therapy for polymyalgia rheumatica. She was not on insulin and was a non-smoker. PK had a BMI of 35.1 kg/m2 and wore an FF bra with a nipple to sternal notch measurement of 40 cm bilaterally.

Photographs of patient PK preoperatively and at 6 months follow up.
After multiple discussions regarding reduction mammoplasty with or without nipple preservation, PK and the treating team opted for Goldilocks mastectomy with free nipple grafting, given the significant amount of subcutaneous tissue in her skin flaps.
In total, 1.5 kg of breast tissue was removed from the left breast and 1.6 kg from the right. The histopathology was benign. PK recovered well from the procedure and the nipple grafts were 100% viable bilaterally at her postoperative follow up (Fig. 1).
Case 2
CH, a 67-year-old woman, presented with screening mammogram-detected high-grade ductal carcinoma in situ (DCIS) of the left breast. The breasts were dense on Breast Imaging Reporting and Data System and MRI defined a 7 cm area of disease. CH had no personal or family history of breast or ovarian cancer. She was a non-smoker and did not suffer from immunocompromise.
On examination, CH had a 20 K breast size with extreme pseudoptosis with a nipple to sternal notch distance of 38 cm, bilaterally. There was no palpable abnormality in either breast.
Given the abundance of subcutaneous tissue in her breasts and a wish to avoid adjuvant radiotherapy, CH underwent bilateral Goldilocks mastectomies with free nipple grafts and a left sentinel lymph node biopsy (Fig. 2). The weight of the right mastectomy specimen was 2.125 kg and the left specimen was 1.820 kg.

CH recovered from the procedure uneventfully and the nipple-areola complex (NAC) graft was completely viable at 6-month review. The histopathology returned a 38 mm area of high-grade DCIS without any invasive disease. The multidisciplinary team meeting concluded that no adjuvant treatment was required.
Discussion
When faced with the high-risk patient requiring mastectomy, Goldilocks mastectomy offers a potentially safe path to a cosmetically sound result. In their seminal paper, Richardson and Ma, 2012, found a complication rate of 8% in their series of 30 patients and 50 breasts reconstructed with Goldilocks mastectomy [10]. In the largest published series of Goldilocks mastectomy, Chaudhry et al, performed 96 procedures on 50 patients with a mean BMI of 33.7 [11]. The authors reported a 9.38% complication rate, with only one breast requiring a takeback to theatre.
The Goldilocks procedure also appears oncologically sound, with Richardson and Ma, having no episodes of locoregional recurrence of malignancy in 29 patients undergoing the procedure for malignancy [10].
The lipodermal flap created during a Goldilocks procedure is large and demands adequate blood supply to survive. During a mastectomy, the blood supply from the breast parenchyma, including the septal blood supply, is divided. As a result, the vascularity of the flap becomes a significant consideration for surgical success [14].
Vascularity is particularly important when accounting for the subsequent tissue folding to create the new breast mound [10]. Recent discoveries regarding the fifth anterior intercostal artery perforator (AICAP) vessels explain how such a large area of tissue remains perfused following a Goldilocks mastectomy [15]. Described by Nahabedian et al., it is now understood that instead of running with the fourth AICAP vessels in the mammary septum as previously thought, the fifth AICAPs take a divergent course and travel within the subcutaneous fat at the 6 o’clock position (Fig. 3). By performing an anatomical mastectomy and preserving the anterior lamellar fat of the breast, these vessels are retained and are the primary blood supply to the new breast mound [15].
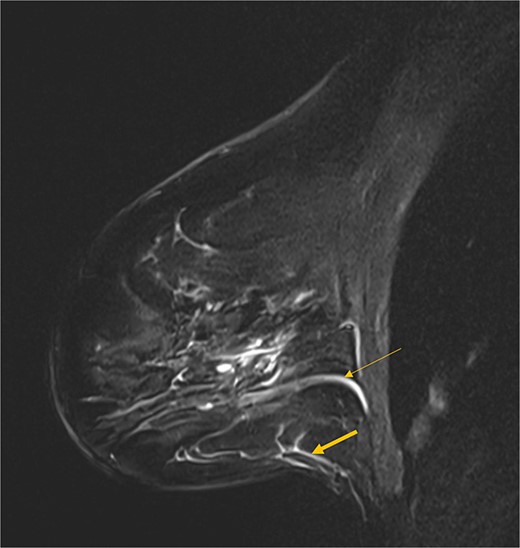
Sagittal MRI image showing the fourth AICAP vessels in the breast septum (thin arrow) and the fifth AICAP vessels travelling in the subcutaneous tissue (thick arrow).
Nipple preservation significantly improves patient quality of life following mastectomy with breast reconstruction [10]. Patients suitable for a Goldilocks mastectomy are typically very large-breasted as in our described cases. Between the pedicle lengths, the folding of the lipodermal flap and the retroareolar dissection required for an anatomical mastectomy, in situ NAC preservation is high risk during a Goldilocks mastectomy. As suitable patients commonly suffer from significant comorbidities, reoperation is best avoided. As such, free nipple grafting is an excellent enhancement of the Goldilocks mastectomy [4, 13].
Removing the NAC makes the lipodermal flap more flexible and easier to shape, as the NAC acts as an anchoring point and limits mobility. The NAC can then be grafted in an optimal location. In their 10-patient series of severely obese patients, Schwartz et al., used free nipple grafting in all of their patients with good outcomes [4].
Goldilocks mastectomy provides further benefits for comorbid patients on account of its abbreviated operative time when compared to skin sparing mastectomy with reconstruction [12]. It also allows select patients to avoid adjuvant radiotherapy and its inherent issues in macromastia.
Further enhancement of Goldilocks mastectomy with a second stage procedure involving fat grafting allows for further aesthetic improvement, particularly in patients with a lower BMI and less subcutaneous fat. The procedure may also be used as the first stage of a two-stage implant-based reconstruction, obviating the need for a tissue expander in high-risk populations [4].
While safe, the Goldilocks approach has limitations. The reconstruction is dependent on subcutaneous fat and outcomes will be poor in those with limited resources, particularly if there is minimal tissue for subsequent fat grafting.
Even in patients with a voluminous skin flap, the breast projection following Goldilocks mastectomy will typically be inferior to traditional means of reconstruction [11]. Additionally, the approach often results in redundant lateral tissue, which can produce a boxy appearance to the breast when coupled with limited projection [11].
Conclusion
By leveraging the fifth perforator anatomy, the Goldilocks mastectomy with nipple grafting offers a promising approach to achieving enhanced cosmetic outcomes while minimizing mastectomy’s physical and psychosocial impacts. This technique is particularly beneficial for suitable candidates who seek a less invasive reconstruction method or are ineligible for implant-based reconstruction. Future research and broader application of this technique will further define its role in modern breast surgery.
Conflicts of interest statement
The authors have no conflicts of interest to declare.
Funding
None declared.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.



