-
PDF
- Split View
-
Views
-
Cite
Cite
Waniyah Masood, Raheel Ahmed, Faizan Ahmed Fazlani, Shaheryar Shakir, Md Al Hasibuzzaman, Multiple intussusceptions secondary to Peutz–Jegher’s syndrome in an adult male: a case report from Pakistan, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjae008, https://doi.org/10.1093/jscr/rjae008
Close - Share Icon Share
Abstract
Intussusception is a medical condition characterized by invagination of the intestinal segment, causing obstruction and leading to potential complications such as ischemia, necrosis and perforation. While paediatric intussusception is well documented with a peak in ages between 4 and 36 months, adult intussusception is a rare condition usually involving a lead point. In this article, we present an uncommon case of an adult male with worsening of his long-standing lower abdominal pain for the last 2 months. Radiological test reports revealed target-like lesions demonstrating two intestinal intussusceptions, for which he underwent a small bowel anastomosis, exploratory laprotomy and resection. On receiving the histopathology report, hamartomatous polyps with features favouring Peutz–Jegher’s syndrome were identified as a possible lead point.
Introduction
Intussusception is a medical condition that involves telescoping invagination of an intestinal segment into the lumen of the proximal segment, causing an obstruction. The long-term invagination can impair blood flow and can cause ischemia, necrosis and perforation. The prevalence of paediatric intussusception, which has a peak incidence between 4 and 36 months of age, is well documented and typically has a benign aetiology without a pathological lead point [1]. Adult intussusception (AI), however, is a rare condition that only accounts for 1%–5% of all occurrences of intestinal obstruction and in 90% of cases involves an underlying lead point. Adults in the fifth decade or later are typically affected. Notably, intussusception risk is increased by any alteration to the regular pattern of intestinal peristalsis. Meckel’s diverticulums, hematomas, benign or malignant tumours, polyps and vascular abnormalities can all be served as lead points for the condition [2].
According to the landmarks of its origin and extension, the bowel intussusception is typically divided into four types: Enteric type: the intussusception is restricted to the small intestine; Ileocolic type: the ileum passes the ileocolic segment, but the appendix does not invaginate; Ileocecal type: the ileocecal portion invaginates into the ascending colon; and Colocolonic type: the intussusception is restricted to the colon and rectum. Enteric, ileocolic and colocolonic types together account for 49.5%, 29.1% and 19.9% of all cases, respectively [3].
Since AI has nonspecific clinical signs, an accurate preoperative diagnosis could be challenging. Pain is the most prevalent symptom of adult patients; however, its intermittent nature encourages a delayed diagnosis. The next most frequent symptoms includes nausea, vomiting, abnormal bowel habits and gastrointestinal (GI) bleeding [4]. While abdominal X-ray, small bowel series with barium and abdominal ultrasound are among the diagnostic techniques that may help in the diagnosis of intussusception, computed tomography (CT) is now considered as the gold standard.
Case description
A 28-year-old male of lean build (body mass index of 14.3) with no known comorbidity presented to the Emergency Department for evaluation of worsening of his intermittent lower abdominal pain and vomiting since 2 months. Abdominal pain was gradual in onset, non-shifting with no aggravating factors and was relieved on taking pain killers. Abdominal pain was also associated with vomiting: two to three episodes per day; vomiting was non-bloody and non-projectile. According to the patient he has been experiencing on and off gastric symptoms such as altered bowel habits, loss of appetite, heart burn and regurgitation since the age of 10 years. Regarding his past medical and surgical history, the patient was admitted having similar issue 6 months back in medicine ward and observed no improvement on treatment. He had exploratory laparotomy done in year 2012 and was also operated for some gastric issue in year 2000, no records available. On examination, abdomen was soft, tenderness and slight distention was felt in the lower quadrant, and gut sounds were audible. The cardiovascular and respiratory examination was unremarkable. On Digital rectal examination, normal anal tone was observed however, fecal and blood staining was positive.
Investigations
Blood tests, a 12-lead electrocardiogram, a chest X-ray and an abdominal X-ray were conducted in light of the ongoing abdominal pain, but the results were unremarkable. Additionally, pre- and post-contrast CT of the pelvis and abdomen was performed in a variety of planes and settings. After administering oral and intravenous contrast, it was seen that the proximal small bowel loops were dilated along with an ileo-ileal intussusception in the midline in the hypogastric region and jejuno-jejunal intussusception in the lumbar region. Figure 1 shows a CT coronal picture of the abdomen and pelvis that illustrates an intussusception and dilated loops. A spherical mass referred as ‘target-like lesion/donut-like lesion’, which is indicative of intussusception, is also seen in the CT axial image as seen in Fig. 2.

CT coronal picture of the abdomen and pelvis, illustrating dilated loops and intussusception.
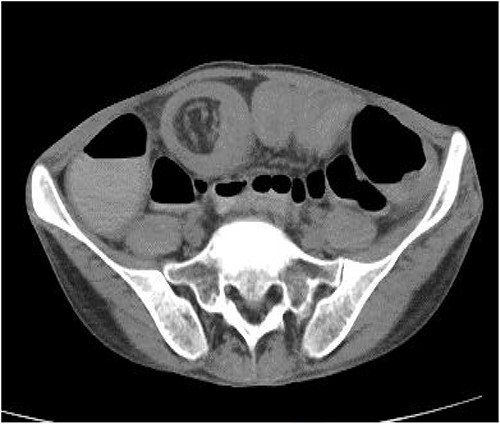
CT axial image showing a spherical mass referred as ‘target-like lesion/ donut-like lesion’, indicative of intussusception.
Management
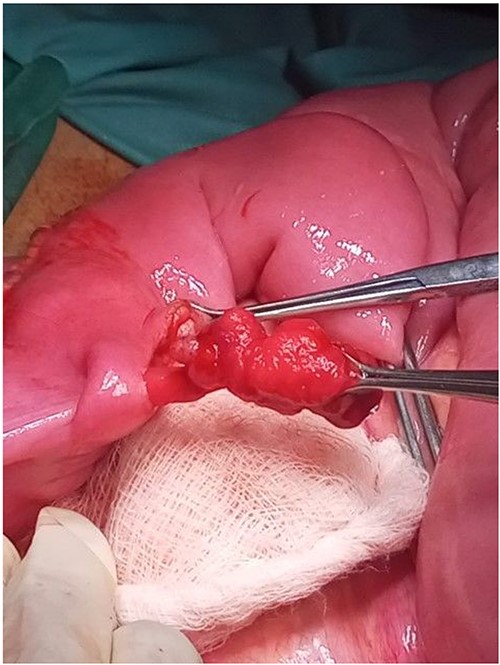
Based on the patient’s clinical state and the imaging findings, it was decided to proceed with operational management. The patient underwent a small bowel anastomosis, exploratory laprotomy and resection. Operative results included a telescoping sections 7.5 feet distal to the duodenojejunal flexure (DJ), 1.5 feet distal to DJ and 2.5 feet distal to DJ harbouring sessile pedunculated polyps (Figs 3–4). The intussusception lengths were 2 × 2, 1.5 × 1.5, and 1.5 × 1.5 cm, respectively. Following identification, enterotomies using diathermy were performed; a few polyps from the intussusception site were excised along with resection of the telescoped segment and end-to-end anastomosis was done in an extramucosal, subserosal manner in an uninterrupted fashion. Resected polyp, intestinal segment and mesenteric lymph nodes were all sent to the lab for histopathology. The patient received intravenous fluids and antibiotics throughout the brief postoperative interval, which went uneventful. On Day 3, a postoperative ultrasound of the whole abdomen was done, and it showed no evidence of intussusception. After 5 days, the patient was discharged from the hospital. On follow-up after 2 weeks, patient showed improvement with the symptoms, vitals and clinical state was unremarkable. On receiving histopathology report, hamartomatous polyps with features favouring Peutz–Jegher’s syndrome (PJS) were identified, with no evidence of invasion, dysplasia or malignancy seen.

Discussion
PJS is a rare autosomal dominant genetic condition characterized by the development of GI hamartomatous polyps and mucocutaneous melanin pigmentation. It affects 55% of first-degree relatives with a prevalence of 1:1200000, and is typically diagnosed between the ages of 20 and 30. Hamartomatous polyps are multilobed polyps with a papillary surface and branching bands of smooth muscle covered in glandular epithelium; they may be pedunculated or sessile. They are mostly prevalent in small bowel (64%), colon (53%), stomach (49%), rectum (32%), gallbladder, bronchial passages, bladder and ureters. Other clinical manifestations of PJS include mucocutaneous hyperpigmentation of the mouth, lips, nose, eyes, genitalia or fingers, as well as a family history of the condition [5].PJS is linked to a higher risk of cancers, including extra-intestinal and GI malignancies. The reported lifetime risk for any malignancy ranged between 37% and 93% in a systematic evaluation of 20 observational studies evaluating over 1644 people with PJS [6]. The colorectal region is shown to be the most frequently affected by cancer, followed by the breast, stomach, small intestine and pancreas. The carcinoma transformation in the PJS may require rigorous monitoring and surveillance performed with colonoscopy and upper endoscopy of the GI system at risk [6].
Besides malignancy, patients with PJS have a high lifetime risk of GI bleeding, bowel obstruction, rectal prolapse and intussusception at an early age. Polyps >15 mm typically induces intussusceptions. A cohort study by van Lier et al. [7] including 110 PJS patients found that intussusception affected 76 individuals (69%) overall, with a median age of 16 (3–50) years. At age 20, the risk of intussusception was 50% (95% confidence interval: 17–23 years), and it was unaffected by sex, family history or mutation status. In 95% of cases, intussusceptions involved the small intestine, and manifested as an acute abdomen.
Patients who experience multiple intussusceptions almost invariably need surgical intervention. In case of PJS an addition to polypectomy could be beneficial. The significance of follow-up in patients with PJS, however, is particularly important, in part because it is critical to monitor the location, size and number of polyps to avoid further GI difficulties and anaemia, as well as to eventually check for carcinogenic changes [8].
Conclusion
In adults presenting with abdominal pain, intussusception must be taken into consideration as a possible differential diagnosis, despite its rarity. An accurate and prompt diagnosis is essential for timely diagnosis and to decrease the morbidity and mortality linked to intussusception. Depending on the underlying cause, treatment options can range from conservative measures to surgical surgery. Intussusception and GI lumen obstruction are two complications of a rare inherited PJS. Symptoms may be alleviated by surgery, such as polypectomy and resection.
Conflict of interest statement
None declared.
Funding
None declared.
Consent for publication
Written consent was taken from the patient.



