-
PDF
- Split View
-
Views
-
Cite
Cite
Kah A Ho, Rajkumar Srinivasan, Torsion of Meckel’s diverticulum—a case report and literature review, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjad740, https://doi.org/10.1093/jscr/rjad740
Close - Share Icon Share
Abstract
Meckel’s diverticulum (MD) is the most common congenital anomaly of the gastrointestinal tract. Torsion is a rare complication of MD with only 48 cases described in the English literature to date. We describe a case of a 22-year-old male who presented to the emergency department with lower abdominal pain. Pre-operative computed tomography scan suggested a torted MD. This was confirmed on diagnostic laparoscopy and managed with segmental resection of the MD and a concurrent appendicectomy. Histopathology confirmed torsion of MD and a normal appendix. The patient recovered well without any complications. Torsion occurs invariably with giant MD defined as a length of >5 cm. Surgical options for MD include diverticulectomy, wedge resection and segmental resection via laparoscopic or open approach. The rate of pre-operative diagnosis remains low but with advances in imaging and awareness of this condition, this is likely to increase with time.
Introduction
Torted Meckel’s Diverticulum (MD) is a rare entity. We describe a case of MD torsion that was diagnosed pre-operatively and managed with laparoscopic resection. MD is the most common congenital anomaly of the gastrointestinal tract. It results from incomplete atrophy of the vitelline duct in the embryo and is classified as a true diverticulum containing all three layers of the intestinal wall [1, 2]. The prevalence of MD is ~0.3–2.9% in the general population with preponderance towards males [2]. The classical features of MD had long been taught as the ‘rule of twos′. The rule states MD is located 2 feet proximal to the ileocecal valve (ICV), presents before 2 years of age, seen twice as commonly in men as women and is found in 2% of the population [3].
Case report
A 22-year-old male presented to the emergency department with a 12 hour history of right iliac fossa and suprapubic pain. He had no other presenting complaints including nausea, vomiting, or anorexia. He had no significant past medical or surgical history except for a similar presentation to the hospital 3 months prior with spontaneous improvement of his pain and was discharged home without further investigations. He had no listed regular medications. On examination, he was afebrile with normal vital signs. He was tender to palpate over his right iliac fossa and suprapubic area with associated voluntary guarding. No signs of generalized peritonism could be elicited. He had raised white cell count of 15 × 109/L. His electrolytes, renal function, haemoglobin, and C-reactive protein (CRP) were normal.
Computed tomography (CT) of the abdomen and pelvis with portal venous phase contrast (see Fig. 1) demonstrated a gas and fluid filled blind structure in the right lower quadrant measuring 40 mm in diameter communicating with a small bowel loop anteriorly. There was a whorled appearance of its neck with subtle surrounding fat stranding suggestive for a torted MD. The appendix appeared to be separate from the abnormality, lying superiorly and to its right with its tip adjacent to the right iliac vessels. Small volume of free fluid in the pelvis was identified without free air in the peritoneal cavity to suggest hollow viscus perforation.

CT abdomen pelvis showing gas and fluid-filled structure in pelvis.
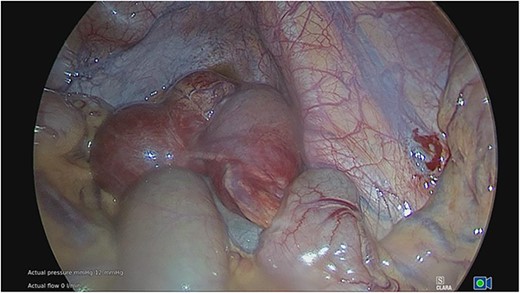
The patient was commenced on isotonic intravenous fluids and broad-spectrum intravenous antibiotics. Diagnostic laparoscopy was done on the same day confirming a torted MD with early gangrenous changes associated with a congenital band (see Figs 2 and 3). No evidence of perforation or purulence was identified during laparoscopy in the peritoneal cavity. A segmental resection of the MD with primary stapled anastomosis of the small intestine was performed through a 5 cm Pfannenstiel incision. The appendix though mildly injected did not demonstrate features of appendicitis macroscopically. Given its proximity to the pathology, an appendicectomy was performed concurrently.
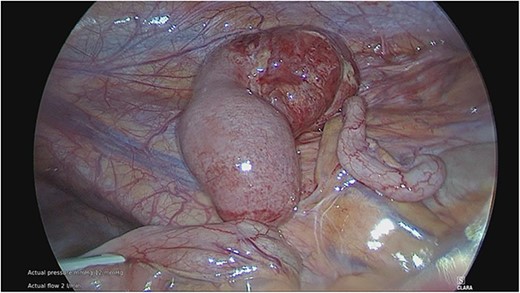
Torted MD with gangrenous distal portion. Adjacent appendix appears mildly injected.
Histopathology of the specimens confirmed torsion of MD and a normal appendix. The MD had a 6 cm length and 4 cm width. The patient had an uneventful postoperative course and was discharged home on the 4th postoperative day. He was seen for follow-up in the outpatient clinic 2 weeks later and he remained well with no complications.
Discussion
A comprehensive literature review of all cases of MD torsion was conducted on the PubMed and EMBASE database using search terms ‘torsion′ and ‘Meckel’s diverticulum′ with the Boolean operator ‘AND′. Additional articles were also found through searching reference lists and google scholar. Only 47 were found in the English language and the full text was available. Including our case, data were gathered for 48 patients with torsion of MD. Table 1 summarizes the findings gathered from all the case reports.
| Case . | Author . | Year . | Age (years) . | Sex . | Size (cm) . | Distance from ICV (cm) . | Approach . | Operation . |
|---|---|---|---|---|---|---|---|---|
| 1 | Our case | 2023 | 22 | M | 6 × 4 | 75 | Laparoscopy assisted | Segmental resection |
| 2 | Mashlah et al. | 2023 | 0.75 (9 months) | M | 120 | Laparotomy | Segmental resection | |
| 3 | Kafshgari et al. | 2023 | 5 | F | Laparotomy | Segmental resection | ||
| 4 | Munasinghe et al. | 2022 | 20 | M | 25 × 2 | 45 | Laparotomy | Segmental resection |
| 5 | Maree et al. | 2022 | 2.5 | M | Laparotomy | Wedge resection | ||
| 6 | Goh et al. | 2022 | 38 | M | 50 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 7 | Bejiga and Ahmed | 2022 | 20 | M | 8 | 60 | Laparotomy | Segmental resection |
| 8 | Onyemkpa et al. | 2021 | 49 | M | Laparoscopy | Diverticulectomy | ||
| 9 | Jha et al. | 2021 | 13 | F | 10 × 2 | 30 | Laparotomy | Segmental resection |
| 10 | Chen et al. | 2021 | 20 | M | 12 | 80 | Laparotomy | Diverticulectomy |
| 11 | Ahmed et al. | 2021 | 28 | F | Laparoscopy | Diverticulectomy | ||
| 12 | Ajmal et al. | 2020 | 25 | M | 12 | 50 | Laparotomy | Segmental resection |
| 13 | Nagata et al. | 2019 | 31 | F | 11 × 8 × 5 | 2 | Laparotomy | Ileocaecal resection |
| 14 | Hung et al. | 2019 | 48 | M | 10 | 40 | Laparotomy | Segmental resection |
| 15 | Yagnik | 2018 | 14 | M | Laparotomy | Segmental resection | ||
| 16 | Tiong et al. | 2018 | 44 | M | 10 × 2 | Laparotomy | Segmental resection | |
| 17 | Botezatu et al. | 2018 | 30 | F | 5 × 1 | 55 | Laparotomy | Diverticulectomy |
| 18 | Parab et al. | 2017 | 11 | F | 15 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 19 | Morao et al. | 2017 | 14 | M | 12 × 7 | 50 | Laparotomy | Segmental resection |
| 20 | Kohga et al. | 2017 | 49 | M | 8 × 7.5 | 130 | Laparoscopy assisted | Segmental resection |
| 21 | Yildiz et al. | 2016 | 21 | F | 12 × 3 | 45 | Laparoscopy ➔ Laparotomy | Diverticulectomy |
| 22 | Rosenbaum and Pollock | 2016 | 5 | M | 12 | Laparotomy | ||
| 23 | Luu et al. | 2016 | 34 | M | 17 | 40 | Laparotomy, segmental resection | Segmental resection |
| 24 | Kirmizi et al. | 2016 | 23 | F | 8 × 3 | 60 | Laparotomy | Segmental resection |
| 25 | Ahmed et al. | 2016 | 4 | M | 5 × 2 | 40 | Laparoscopy | Segmental resection |
| 26 | Tenreiro et al. | 2015 | 18 | M | 10 × 2 | 50 | Laparotomy | Segmental resection |
| 27 | Seshadri et al. | 2015 | 65 | M | 8 | 60 | Laparoscopy ➔ laparotomy | Diverticulectomy |
| 28 | Rencuzogullari et al. | 2015 | 37 | M | 60 | laparotomy | Segmental resection | |
| 29 | Ren et al. | 2015 | 32 | M | 12 × 5 × 4 | 90 | Laparotomy | Segmental resection |
| 30 | Hadeed et al. | 2015 | 29 | F | 30 | Laparoscopy | Diverticulectomy | |
| 31 | Murruste et al. | 2014 | 41 | M | 14 × 12 | 50 | Laparotomy | Segmental resection |
| 32 | Tassinari et al. | 2013 | 1 | M | 6 × 3 | 50 | Laparoscopy | Wedge resection |
| 33 | Sasikumar et al. | 2013 | 26 | M | 6 × 3 | Laparotomy | Segmental resection | |
| 34 | Nose et al. | 2013 | 11 | M | 6 × 2 | 70 | Laparoscopy | Wedge resection |
| 35 | Seth et al. | 2011 | 68 | M | Laparoscopy ➔ Laparotomy | Segmental resection | ||
| 36 | Halliday et al. | 2011 | 62 | F | 6.5 | Laparoscopy ➔ Laparotomy | Segmental resection | |
| 37 | Cartanese et al. | 2011 | 42 | M | 11 × 1.5 | 50 | Laparotomy | Diverticulectomy |
| 38 | Nunes et al. | 2009 | 47 | M | 14 × 3 | 80 | Laparotomy | Segmental resection |
| 39 | Kiyak et al. | 2009 | 42 | M | 7.5 × 1.5 | 80 | Laparotomy | Diverticulectomy |
| 40 | Prasad et al. | 2006 | 13 | M | Laparoscopy | Diverticulectomy | ||
| 41 | Limas et al. | 2006 | 6 | M | 16 × 4 × 4 | 50 | Laparotomy | Diverticulectomy |
| 42 | Tan and Zheng | 2005 | 51 | M | 10 × 3 | 60 | Laparotomy | Segmental resection |
| 43 | Farris and Fernbach | 2001 | 14 | M | Laparotomy | Resection | ||
| 44 | Malhotra et al. | 1998 | 54 | M | Laparotomy | Segmental resection | ||
| 45 | Gallego-Herrero et al. | 1998 | 2 | M | 5.8 × 3 | 20 | Not specified | |
| 46 | Moore and Burkle | 1988 | 3.5 | M | 8 × 2.5 | 60.9 | Not specified | |
| 47 | Webster | 1966 | 41 | M | Laparotomy | Diverticulectomy | ||
| 48 | NEJM | 1952 | 2.5 | M | 8 | 90 | Wedge resection |
| Case . | Author . | Year . | Age (years) . | Sex . | Size (cm) . | Distance from ICV (cm) . | Approach . | Operation . |
|---|---|---|---|---|---|---|---|---|
| 1 | Our case | 2023 | 22 | M | 6 × 4 | 75 | Laparoscopy assisted | Segmental resection |
| 2 | Mashlah et al. | 2023 | 0.75 (9 months) | M | 120 | Laparotomy | Segmental resection | |
| 3 | Kafshgari et al. | 2023 | 5 | F | Laparotomy | Segmental resection | ||
| 4 | Munasinghe et al. | 2022 | 20 | M | 25 × 2 | 45 | Laparotomy | Segmental resection |
| 5 | Maree et al. | 2022 | 2.5 | M | Laparotomy | Wedge resection | ||
| 6 | Goh et al. | 2022 | 38 | M | 50 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 7 | Bejiga and Ahmed | 2022 | 20 | M | 8 | 60 | Laparotomy | Segmental resection |
| 8 | Onyemkpa et al. | 2021 | 49 | M | Laparoscopy | Diverticulectomy | ||
| 9 | Jha et al. | 2021 | 13 | F | 10 × 2 | 30 | Laparotomy | Segmental resection |
| 10 | Chen et al. | 2021 | 20 | M | 12 | 80 | Laparotomy | Diverticulectomy |
| 11 | Ahmed et al. | 2021 | 28 | F | Laparoscopy | Diverticulectomy | ||
| 12 | Ajmal et al. | 2020 | 25 | M | 12 | 50 | Laparotomy | Segmental resection |
| 13 | Nagata et al. | 2019 | 31 | F | 11 × 8 × 5 | 2 | Laparotomy | Ileocaecal resection |
| 14 | Hung et al. | 2019 | 48 | M | 10 | 40 | Laparotomy | Segmental resection |
| 15 | Yagnik | 2018 | 14 | M | Laparotomy | Segmental resection | ||
| 16 | Tiong et al. | 2018 | 44 | M | 10 × 2 | Laparotomy | Segmental resection | |
| 17 | Botezatu et al. | 2018 | 30 | F | 5 × 1 | 55 | Laparotomy | Diverticulectomy |
| 18 | Parab et al. | 2017 | 11 | F | 15 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 19 | Morao et al. | 2017 | 14 | M | 12 × 7 | 50 | Laparotomy | Segmental resection |
| 20 | Kohga et al. | 2017 | 49 | M | 8 × 7.5 | 130 | Laparoscopy assisted | Segmental resection |
| 21 | Yildiz et al. | 2016 | 21 | F | 12 × 3 | 45 | Laparoscopy ➔ Laparotomy | Diverticulectomy |
| 22 | Rosenbaum and Pollock | 2016 | 5 | M | 12 | Laparotomy | ||
| 23 | Luu et al. | 2016 | 34 | M | 17 | 40 | Laparotomy, segmental resection | Segmental resection |
| 24 | Kirmizi et al. | 2016 | 23 | F | 8 × 3 | 60 | Laparotomy | Segmental resection |
| 25 | Ahmed et al. | 2016 | 4 | M | 5 × 2 | 40 | Laparoscopy | Segmental resection |
| 26 | Tenreiro et al. | 2015 | 18 | M | 10 × 2 | 50 | Laparotomy | Segmental resection |
| 27 | Seshadri et al. | 2015 | 65 | M | 8 | 60 | Laparoscopy ➔ laparotomy | Diverticulectomy |
| 28 | Rencuzogullari et al. | 2015 | 37 | M | 60 | laparotomy | Segmental resection | |
| 29 | Ren et al. | 2015 | 32 | M | 12 × 5 × 4 | 90 | Laparotomy | Segmental resection |
| 30 | Hadeed et al. | 2015 | 29 | F | 30 | Laparoscopy | Diverticulectomy | |
| 31 | Murruste et al. | 2014 | 41 | M | 14 × 12 | 50 | Laparotomy | Segmental resection |
| 32 | Tassinari et al. | 2013 | 1 | M | 6 × 3 | 50 | Laparoscopy | Wedge resection |
| 33 | Sasikumar et al. | 2013 | 26 | M | 6 × 3 | Laparotomy | Segmental resection | |
| 34 | Nose et al. | 2013 | 11 | M | 6 × 2 | 70 | Laparoscopy | Wedge resection |
| 35 | Seth et al. | 2011 | 68 | M | Laparoscopy ➔ Laparotomy | Segmental resection | ||
| 36 | Halliday et al. | 2011 | 62 | F | 6.5 | Laparoscopy ➔ Laparotomy | Segmental resection | |
| 37 | Cartanese et al. | 2011 | 42 | M | 11 × 1.5 | 50 | Laparotomy | Diverticulectomy |
| 38 | Nunes et al. | 2009 | 47 | M | 14 × 3 | 80 | Laparotomy | Segmental resection |
| 39 | Kiyak et al. | 2009 | 42 | M | 7.5 × 1.5 | 80 | Laparotomy | Diverticulectomy |
| 40 | Prasad et al. | 2006 | 13 | M | Laparoscopy | Diverticulectomy | ||
| 41 | Limas et al. | 2006 | 6 | M | 16 × 4 × 4 | 50 | Laparotomy | Diverticulectomy |
| 42 | Tan and Zheng | 2005 | 51 | M | 10 × 3 | 60 | Laparotomy | Segmental resection |
| 43 | Farris and Fernbach | 2001 | 14 | M | Laparotomy | Resection | ||
| 44 | Malhotra et al. | 1998 | 54 | M | Laparotomy | Segmental resection | ||
| 45 | Gallego-Herrero et al. | 1998 | 2 | M | 5.8 × 3 | 20 | Not specified | |
| 46 | Moore and Burkle | 1988 | 3.5 | M | 8 × 2.5 | 60.9 | Not specified | |
| 47 | Webster | 1966 | 41 | M | Laparotomy | Diverticulectomy | ||
| 48 | NEJM | 1952 | 2.5 | M | 8 | 90 | Wedge resection |
ICV: ileocaecal valve; M: male; F: female.
| Case . | Author . | Year . | Age (years) . | Sex . | Size (cm) . | Distance from ICV (cm) . | Approach . | Operation . |
|---|---|---|---|---|---|---|---|---|
| 1 | Our case | 2023 | 22 | M | 6 × 4 | 75 | Laparoscopy assisted | Segmental resection |
| 2 | Mashlah et al. | 2023 | 0.75 (9 months) | M | 120 | Laparotomy | Segmental resection | |
| 3 | Kafshgari et al. | 2023 | 5 | F | Laparotomy | Segmental resection | ||
| 4 | Munasinghe et al. | 2022 | 20 | M | 25 × 2 | 45 | Laparotomy | Segmental resection |
| 5 | Maree et al. | 2022 | 2.5 | M | Laparotomy | Wedge resection | ||
| 6 | Goh et al. | 2022 | 38 | M | 50 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 7 | Bejiga and Ahmed | 2022 | 20 | M | 8 | 60 | Laparotomy | Segmental resection |
| 8 | Onyemkpa et al. | 2021 | 49 | M | Laparoscopy | Diverticulectomy | ||
| 9 | Jha et al. | 2021 | 13 | F | 10 × 2 | 30 | Laparotomy | Segmental resection |
| 10 | Chen et al. | 2021 | 20 | M | 12 | 80 | Laparotomy | Diverticulectomy |
| 11 | Ahmed et al. | 2021 | 28 | F | Laparoscopy | Diverticulectomy | ||
| 12 | Ajmal et al. | 2020 | 25 | M | 12 | 50 | Laparotomy | Segmental resection |
| 13 | Nagata et al. | 2019 | 31 | F | 11 × 8 × 5 | 2 | Laparotomy | Ileocaecal resection |
| 14 | Hung et al. | 2019 | 48 | M | 10 | 40 | Laparotomy | Segmental resection |
| 15 | Yagnik | 2018 | 14 | M | Laparotomy | Segmental resection | ||
| 16 | Tiong et al. | 2018 | 44 | M | 10 × 2 | Laparotomy | Segmental resection | |
| 17 | Botezatu et al. | 2018 | 30 | F | 5 × 1 | 55 | Laparotomy | Diverticulectomy |
| 18 | Parab et al. | 2017 | 11 | F | 15 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 19 | Morao et al. | 2017 | 14 | M | 12 × 7 | 50 | Laparotomy | Segmental resection |
| 20 | Kohga et al. | 2017 | 49 | M | 8 × 7.5 | 130 | Laparoscopy assisted | Segmental resection |
| 21 | Yildiz et al. | 2016 | 21 | F | 12 × 3 | 45 | Laparoscopy ➔ Laparotomy | Diverticulectomy |
| 22 | Rosenbaum and Pollock | 2016 | 5 | M | 12 | Laparotomy | ||
| 23 | Luu et al. | 2016 | 34 | M | 17 | 40 | Laparotomy, segmental resection | Segmental resection |
| 24 | Kirmizi et al. | 2016 | 23 | F | 8 × 3 | 60 | Laparotomy | Segmental resection |
| 25 | Ahmed et al. | 2016 | 4 | M | 5 × 2 | 40 | Laparoscopy | Segmental resection |
| 26 | Tenreiro et al. | 2015 | 18 | M | 10 × 2 | 50 | Laparotomy | Segmental resection |
| 27 | Seshadri et al. | 2015 | 65 | M | 8 | 60 | Laparoscopy ➔ laparotomy | Diverticulectomy |
| 28 | Rencuzogullari et al. | 2015 | 37 | M | 60 | laparotomy | Segmental resection | |
| 29 | Ren et al. | 2015 | 32 | M | 12 × 5 × 4 | 90 | Laparotomy | Segmental resection |
| 30 | Hadeed et al. | 2015 | 29 | F | 30 | Laparoscopy | Diverticulectomy | |
| 31 | Murruste et al. | 2014 | 41 | M | 14 × 12 | 50 | Laparotomy | Segmental resection |
| 32 | Tassinari et al. | 2013 | 1 | M | 6 × 3 | 50 | Laparoscopy | Wedge resection |
| 33 | Sasikumar et al. | 2013 | 26 | M | 6 × 3 | Laparotomy | Segmental resection | |
| 34 | Nose et al. | 2013 | 11 | M | 6 × 2 | 70 | Laparoscopy | Wedge resection |
| 35 | Seth et al. | 2011 | 68 | M | Laparoscopy ➔ Laparotomy | Segmental resection | ||
| 36 | Halliday et al. | 2011 | 62 | F | 6.5 | Laparoscopy ➔ Laparotomy | Segmental resection | |
| 37 | Cartanese et al. | 2011 | 42 | M | 11 × 1.5 | 50 | Laparotomy | Diverticulectomy |
| 38 | Nunes et al. | 2009 | 47 | M | 14 × 3 | 80 | Laparotomy | Segmental resection |
| 39 | Kiyak et al. | 2009 | 42 | M | 7.5 × 1.5 | 80 | Laparotomy | Diverticulectomy |
| 40 | Prasad et al. | 2006 | 13 | M | Laparoscopy | Diverticulectomy | ||
| 41 | Limas et al. | 2006 | 6 | M | 16 × 4 × 4 | 50 | Laparotomy | Diverticulectomy |
| 42 | Tan and Zheng | 2005 | 51 | M | 10 × 3 | 60 | Laparotomy | Segmental resection |
| 43 | Farris and Fernbach | 2001 | 14 | M | Laparotomy | Resection | ||
| 44 | Malhotra et al. | 1998 | 54 | M | Laparotomy | Segmental resection | ||
| 45 | Gallego-Herrero et al. | 1998 | 2 | M | 5.8 × 3 | 20 | Not specified | |
| 46 | Moore and Burkle | 1988 | 3.5 | M | 8 × 2.5 | 60.9 | Not specified | |
| 47 | Webster | 1966 | 41 | M | Laparotomy | Diverticulectomy | ||
| 48 | NEJM | 1952 | 2.5 | M | 8 | 90 | Wedge resection |
| Case . | Author . | Year . | Age (years) . | Sex . | Size (cm) . | Distance from ICV (cm) . | Approach . | Operation . |
|---|---|---|---|---|---|---|---|---|
| 1 | Our case | 2023 | 22 | M | 6 × 4 | 75 | Laparoscopy assisted | Segmental resection |
| 2 | Mashlah et al. | 2023 | 0.75 (9 months) | M | 120 | Laparotomy | Segmental resection | |
| 3 | Kafshgari et al. | 2023 | 5 | F | Laparotomy | Segmental resection | ||
| 4 | Munasinghe et al. | 2022 | 20 | M | 25 × 2 | 45 | Laparotomy | Segmental resection |
| 5 | Maree et al. | 2022 | 2.5 | M | Laparotomy | Wedge resection | ||
| 6 | Goh et al. | 2022 | 38 | M | 50 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 7 | Bejiga and Ahmed | 2022 | 20 | M | 8 | 60 | Laparotomy | Segmental resection |
| 8 | Onyemkpa et al. | 2021 | 49 | M | Laparoscopy | Diverticulectomy | ||
| 9 | Jha et al. | 2021 | 13 | F | 10 × 2 | 30 | Laparotomy | Segmental resection |
| 10 | Chen et al. | 2021 | 20 | M | 12 | 80 | Laparotomy | Diverticulectomy |
| 11 | Ahmed et al. | 2021 | 28 | F | Laparoscopy | Diverticulectomy | ||
| 12 | Ajmal et al. | 2020 | 25 | M | 12 | 50 | Laparotomy | Segmental resection |
| 13 | Nagata et al. | 2019 | 31 | F | 11 × 8 × 5 | 2 | Laparotomy | Ileocaecal resection |
| 14 | Hung et al. | 2019 | 48 | M | 10 | 40 | Laparotomy | Segmental resection |
| 15 | Yagnik | 2018 | 14 | M | Laparotomy | Segmental resection | ||
| 16 | Tiong et al. | 2018 | 44 | M | 10 × 2 | Laparotomy | Segmental resection | |
| 17 | Botezatu et al. | 2018 | 30 | F | 5 × 1 | 55 | Laparotomy | Diverticulectomy |
| 18 | Parab et al. | 2017 | 11 | F | 15 | Laparoscopy ➔ laparotomy | Segmental resection | |
| 19 | Morao et al. | 2017 | 14 | M | 12 × 7 | 50 | Laparotomy | Segmental resection |
| 20 | Kohga et al. | 2017 | 49 | M | 8 × 7.5 | 130 | Laparoscopy assisted | Segmental resection |
| 21 | Yildiz et al. | 2016 | 21 | F | 12 × 3 | 45 | Laparoscopy ➔ Laparotomy | Diverticulectomy |
| 22 | Rosenbaum and Pollock | 2016 | 5 | M | 12 | Laparotomy | ||
| 23 | Luu et al. | 2016 | 34 | M | 17 | 40 | Laparotomy, segmental resection | Segmental resection |
| 24 | Kirmizi et al. | 2016 | 23 | F | 8 × 3 | 60 | Laparotomy | Segmental resection |
| 25 | Ahmed et al. | 2016 | 4 | M | 5 × 2 | 40 | Laparoscopy | Segmental resection |
| 26 | Tenreiro et al. | 2015 | 18 | M | 10 × 2 | 50 | Laparotomy | Segmental resection |
| 27 | Seshadri et al. | 2015 | 65 | M | 8 | 60 | Laparoscopy ➔ laparotomy | Diverticulectomy |
| 28 | Rencuzogullari et al. | 2015 | 37 | M | 60 | laparotomy | Segmental resection | |
| 29 | Ren et al. | 2015 | 32 | M | 12 × 5 × 4 | 90 | Laparotomy | Segmental resection |
| 30 | Hadeed et al. | 2015 | 29 | F | 30 | Laparoscopy | Diverticulectomy | |
| 31 | Murruste et al. | 2014 | 41 | M | 14 × 12 | 50 | Laparotomy | Segmental resection |
| 32 | Tassinari et al. | 2013 | 1 | M | 6 × 3 | 50 | Laparoscopy | Wedge resection |
| 33 | Sasikumar et al. | 2013 | 26 | M | 6 × 3 | Laparotomy | Segmental resection | |
| 34 | Nose et al. | 2013 | 11 | M | 6 × 2 | 70 | Laparoscopy | Wedge resection |
| 35 | Seth et al. | 2011 | 68 | M | Laparoscopy ➔ Laparotomy | Segmental resection | ||
| 36 | Halliday et al. | 2011 | 62 | F | 6.5 | Laparoscopy ➔ Laparotomy | Segmental resection | |
| 37 | Cartanese et al. | 2011 | 42 | M | 11 × 1.5 | 50 | Laparotomy | Diverticulectomy |
| 38 | Nunes et al. | 2009 | 47 | M | 14 × 3 | 80 | Laparotomy | Segmental resection |
| 39 | Kiyak et al. | 2009 | 42 | M | 7.5 × 1.5 | 80 | Laparotomy | Diverticulectomy |
| 40 | Prasad et al. | 2006 | 13 | M | Laparoscopy | Diverticulectomy | ||
| 41 | Limas et al. | 2006 | 6 | M | 16 × 4 × 4 | 50 | Laparotomy | Diverticulectomy |
| 42 | Tan and Zheng | 2005 | 51 | M | 10 × 3 | 60 | Laparotomy | Segmental resection |
| 43 | Farris and Fernbach | 2001 | 14 | M | Laparotomy | Resection | ||
| 44 | Malhotra et al. | 1998 | 54 | M | Laparotomy | Segmental resection | ||
| 45 | Gallego-Herrero et al. | 1998 | 2 | M | 5.8 × 3 | 20 | Not specified | |
| 46 | Moore and Burkle | 1988 | 3.5 | M | 8 × 2.5 | 60.9 | Not specified | |
| 47 | Webster | 1966 | 41 | M | Laparotomy | Diverticulectomy | ||
| 48 | NEJM | 1952 | 2.5 | M | 8 | 90 | Wedge resection |
ICV: ileocaecal valve; M: male; F: female.
Among the 48 patients, there were 38 males and 10 females. The age ranged from 9 months to 68 years old with a median age of 24 years. There were 17 paediatric cases and 31 adult cases. The most common symptom at presentation was abdominal pain (98%), followed by vomiting (58%), fever (33%), distension (33%), obstipation (23%), and diarrhoea (10%). White cell count was raised in majority of patients (42/47 = 89%). C-reactive protein was not frequently measured but when it was done, the result was abnormal (12/15 = 80%).
The length of MD ranged from 5 cm to 25 cm (mean = 10.3 cm). This is longer than the reported mean of MD in general which is 3.05 cm [2]. Giant MD has been historically defined as MD longer than 5 cm and is theorized to be more prone to complications [4]. Of note, all the patients with torsion of MD had a length of at least 5 cm. The incidence of giant MD is unknown but there have been no instances of incidental finding of asymptomatic giant MD [5].
The width of MD ranged from 1 cm to 12 cm (mean = 3.6 cm). This is also longer than the reported mean of MD in general of 1.58 cm [2]. The distance from ICV ranged from 2 cm up to 130 cm (mean = 56.4 cm). This is slightly higher than the mean distance from ICV for MD in general which is 52.4 cm [2].
In most of the cases the MD was diagnosed intraoperatively (94%). Among these, there were 8 cases where imaging suggested a blind-ending fluid or gas filled structure, but diagnosis was not ultimately made before operation. A pre-operative diagnosis of MD was made in only three of the cases with CT (6.5%).
Surgical options for MD include diverticulectomy, wedge resection, and segmental resection via laparoscopic or open approach [6, 7]. Among patients with torsion of MD, the approach was more commonly done through laparotomy (63%) compared to laparoscopy (31%). This is likely due to the need for diagnosis in the deteriorating surgical patient with unknown diagnosis. The approach was unknown in some of the cases (6%). Of those that started with laparoscopy, most were converted to laparotomy (40%) and some laparoscopy assisted (13%). Among patients with torsion of MD, definitive surgical management was achieved with segmental resection (54%), diverticulectomy (25%) followed by wedge resection (8%). One case required ileocecal resection as the MD was only 2 cm from the IC valve. Appendicectomy was also done in 25% of patients.
Conclusion
We describe a rare case of torsion of MD in a young male patient which was managed with segmental resection without complications. A comprehensive literature review of all previous cases of torsion of MD showed that majority of patients presented with abdominal pain with a leucocytosis. Torsion occurs invariably with giant MD defined as a length of >5 cm. The rate of pre-operative diagnosis remains low but with advances in imaging and awareness of this condition, this would be expected to increase with time which would directly impact on its surgical approach and management.
Conflict of interest statement
No conflict of interests to declare.
Funding
None declared.



