-
PDF
- Split View
-
Views
-
Cite
Cite
Tejminder S Sidhu, Shaurya Jhamb, Matan M Ben David, Surgical resection of isolated portohepatic melanoma metastases—a case report, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjad726, https://doi.org/10.1093/jscr/rjad726
Close - Share Icon Share
Abstract
Metastatic melanoma is a significant public health issue in Australia and New Zealand. Although melanoma commonly metastasises to the liver, isolated hepatic metastases are rare, with isolated metastasis to portohepatic lymph nodes being scarce. As such, the optimal management strategy for this subset of patients remains unclear. Here, we present a case of a patient with isolated portohepatic metastases management with a combination neoadjuvant immunotherapy and surgical resection.
Introduction
Malignant melanoma is a significant public health burden within Australia and New Zealand, and the incidence is rising progressively [1]. The liver is a common site of metastasis for cutaneous melanoma; however, isolated hepatic metastases are rare. Cutaneous melanoma metastasises to the liver in 14%–20% of cases [2, 3], and management of these metastases remains a significant challenge. Metastatic deposits to portohepatic lymph nodes have been described in the context of disseminated disease; however, isolated deposits to this anatomical region have not been described in the literature. The primary management modality of choice of Stage IV melanoma has recently shifted to checkpoint inhibitor immunotherapy; however, if there are isolated hepatic metastases, options may also include chemoembolization, surgical resection, and hepatic intra-arterial chemotherapy [4]. Owing to the rarity of isolated hepatic metastases in this setting, there are limited substantive data regarding the role of surgery. There are no randomized controlled studies available at present, and the bulk of the published literature comprises single centre experience [4]. Here, we present a case of isolated portahepatic lymph node melanoma metastases managed with immunotherapy and surgery in a patient with a history of greater than 24 months post previously excised cutaneous melanoma.
Case presentation
A 72-year-old female was referred to the hepatopancreaticobiliary (HPB) surgery clinic with an FDG avid exophytic lesion measuring 44 × 56 × 78 mm, thought to be arising from the caudate lobe of the liver projecting inferiorly into the portacaval space (Fig. 1A and B). The patient’s oncological history was significant for a previous excision of a left infraorbital/cheek lesion 2 years prior. This initial cutaneous lesion was found to be a superficial spreading melanoma with a Breslow thickness of 2.8 mm with no lymphovascular invasion or ulceration; the margins were clear, however, <5 mm, overall staged as T3aNxM0. The patient was offered a wide local excision and sentinel lymph node biopsy; however, the patient declined and proceeded with close surveillance with six monthly PET scans. The patient was otherwise fit and well with minimal past medical history.
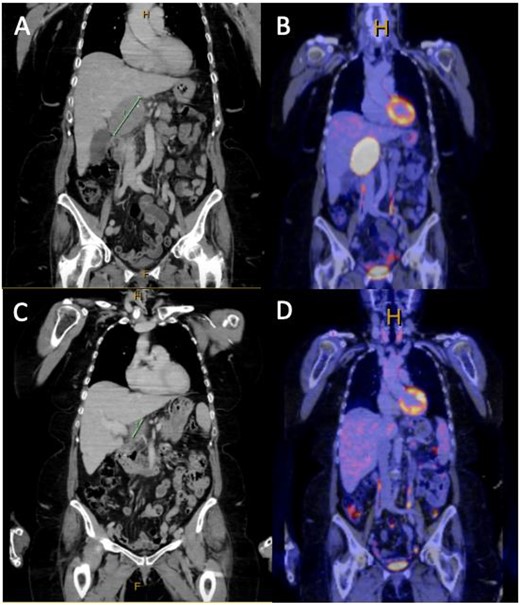
(A and B) Coronal slice of surveillance CT and FDG PET showing a 44 × 56 × 78 mm PET avid exophytic lesion abutting the caudate lobe extending into portocaval space suspicious for metastatic melanoma, given the patients history of cutaneous melanoma; (C and D) coronal slice of CT and FDG PET post three cycles of dual immunotherapy, showing complete metabolic response and significant reduction in size of the metastatic lesion demonstrated in (A) and (B).
Given the high FDG avidity of the caudate lesion endoscopic ultrasound and fine needle aspirate, biopsies were arranged. Histopathology from this biopsy was consistent with a diagnosis of metastatic melanoma. Based on the imaging and tissue diagnosis, the patient was discussed at the HPB multidisciplinary team meeting, and decision was made for the commencement of immunotherapy with potential for surgical resection if there is adequate disease response. The patient was proceeded with dual immunotherapy (ipilimumab and nivolumab), and upon completion of three cycles of immunotherapy, there was a repeat PET/CT scan. The repeat PET scan showed complete metabolic response of the lesion abutting the caudate lobe, which was no longer FDG avid and had reduced in size significantly. The patient underwent a portohepatic lymphadenectomy and cholecystectomy. No macroscopic disease was observed within the peritoneal cavity and a hard 30 × 40 mm nodule was resected from within the hepatoduodenal ligament along with a lymph node packet containing several visible nodes from porta-hepatis to duodenum, including hepatic nodes. Histopathology from this operation showed granulomatous reaction with no viable malignancy remaining. The patient was discharged from HPB surgical clinics 4 weeks postoperatively with an appropriate medical oncology follow-up. The patient is currently 2 months postsurgery and has commenced single-agent immunotherapy with nivolumab as an adjuvant treatment with a planned repeat PET scan when treatment is completed.
Discussion
Historically, metastatic melanoma was known to carry a poor prognosis. However, recent advances in checkpoint inhibitor immunotherapy drugs have significantly improved survival. Combination therapy with cytotoxic T-lymphocyte associated protein 4 inhibitors (ipilimumab) and anti-programmed cell death protein 1 inhibitors (nivolumab and pembrolizumab) has shown significant survival benefit over monotherapy [5]. Prior to immunotherapy, it was estimated that overall Stage IV melanoma had a 5-year survival of between 5% and 15%, depending on the location of metastases [6, 7]. Visceral metastases have a significantly worse prognosis than cutaneous, subcutaneous, or nodal metastases as well as pulmonary metastases [6]. Resection of hepatic metastatic deposits secondary to melanoma remains a contentious topic with limited available literature. Rose et al. (2001) conducted a retrospective review of the databases of two large volume melanoma centres with the aim of assessing the role of surgical resection with regards to hepatic melanoma metastases [8]. While patient selection was important, this series showed that metastasectomy of limited hepatic metastases improved the overall survival [8].
In the case presented, the patient was an otherwise well 72-year-old woman with minimal comorbidities. The patient had biopsy-proven metastatic lesion to the portocaval lymph nodes as well as a suspicious Segment VI lesion necessitating management. The lesions responded well to immunotherapy and the resection specimen showed no residual malignancy. Given the recency of the management of this patient, we are unable to comment on the effect on survival; however, at present, the patient remains disease-free and is completing adjuvant immunotherapy. While there is limited literature on the subject, surgical resection of isolated portohepatic metastases in conjunction with checkpoint inhibitor immunotherapy may work synergistically to improve patient outcomes, and robust research into this topic is needed, given the significant public health burden associated with metastatic melanoma.
Conflict of interest statement
None declared.
Funding
None declared.



