-
PDF
- Split View
-
Views
-
Cite
Cite
Daisuke Hashiba, Kazuki Fujimoto, Ryosuke Nakagawa, Toshifumi Maeyama, Hajime Arai, Seiji Ohtori, Vertebral fracture at the caudal end of diffuse idiopathic skeletal hyperostosis treated with vertebroplasty via double-endplate penetrating screw trajectory and posterior spinal fixation with a new hybrid strategy using cement-augmented fenestrated pedicle screws, Journal of Surgical Case Reports, Volume 2023, Issue 9, September 2023, rjad509, https://doi.org/10.1093/jscr/rjad509
Close - Share Icon Share
Abstract
Vertebral fractures in diffuse idiopathic skeletal hyperostosis (DISH) are often unstable. We encountered a case of vertebral fracture at the caudal end of DISH in which vertebroplasty was performed via a double endplate penetrating screw (DEPS) trajectory, and short posterior fixation was performed using the DEPS technique on the cranial vertebrae, including the fractured vertebra; conventional pedicle screw to the caudal vertebrae; and cement-augmented fenestrated pedicle screws to the caudal end vertebra. A 93-year-old man presented with a vertebral fracture at the caudal end of a DISH after a fall. He underwent surgery for lower back pain due to spinal instability. Vertebroplasty via DEPS trajectory can shorten the posterior fixation range. Using cement-augmented fenestrated pedicle screws to the caudal end vertebra enables balancing of the posterior fixation force. This strategy should be considered when a vertebral fracture is found at the caudal end of the DISH.
Introduction
Vertebral fractures in diffuse idiopathic skeletal hyperostosis (DISH) are prone to nonunion because the stress force is concentrated at the fracture site owing to instability with long lever arms [1]. Therefore, surgical intervention is required [2, 3].
Posterior fixation with endplate penetrating screws (PESs) is effective for DISH-related fractures because of its strong fixation force, and double-endplate penetration is more favorable than single-endplate penetration [4–6]. Vertebroplasty, augmenting the anterior vertebral body with void filler, and pedicle screw fixation are effective in maintaining spinal alignment for thoracolumbar fractures [7]. However, the use of vertebroplasty for vertebral fractures in DISH remains unclear.
Cement-augmented fenestrated pedicle screws can provide a strong fixation force for the osteoporotic spine [8, 9]. Herein, we report a successfully treated case of vertebral fracture at the caudal end of DISH, in which vertebroplasty was performed via a double-endplate penetrating screw (DEPS) trajectory, and short posterior fixation was performed using the DEPS technique on the cranial vertebrae, including the fractured vertebra; conventional pedicle screw to the caudal vertebrae; and cement-augmented fenestrated pedicle screws to the caudal end vertebra.
Case report
A 93-year-old man experienced back pain after falling off a chair approximately a week ago. The pain gradually deteriorated, and the patient could not walk. The patient was subsequently admitted to our hospital.
The patient complained of lower back pain during motion; however, no neurological deficit was noted. Radiographs of the thoracolumbar spine showed L1 vertebral body deformation (Fig. 1A and B). Computed tomography (CT) revealed anterior bony bridging by DISH from T1 to L1 and a vertebral fracture with bony defects in the caudal part of the L1 vertebral body (Fig. 1C).
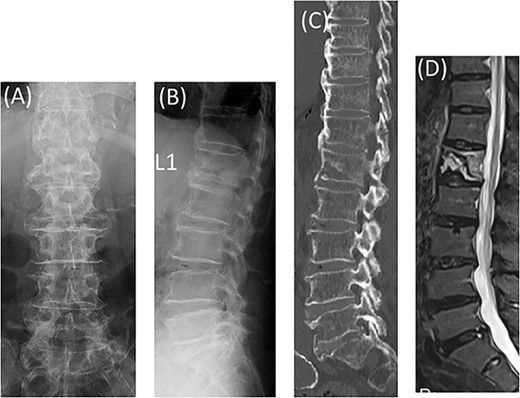
Radiographs showed L1 vertebral body deformation (A, B). CT and MRI STIR revealed anterior bony bridging by DISH and a vertebral fracture in the caudal part of the L1 vertebral body (C, D).
Magnetic resonance imaging (MRI) showed hyperintensities on short inversion time (TI) inversion recovery (STIR) in the L1 vertebral body, indicating a single caudal endplate fracture and ligament failure of the posterior element (Fig. 1D).
The diagnosis was an L1 vertebral fracture at the caudal end of DISH.
Posterior spinal fusion was performed under general anesthesia. Vertebroplasty with hydroxyapatite grafting was performed on the L1 vertebra via the DEPS trajectory from the L2 vertebra. Subsequently, using the DEPS technique, screws were placed at T12, L1, and L2, and conventional pedicle screws were placed at L3. Cement-augmented fenestrated pedicle screws were installed at L4 to enhance the pull-out strength (Fig. 2A–C)).
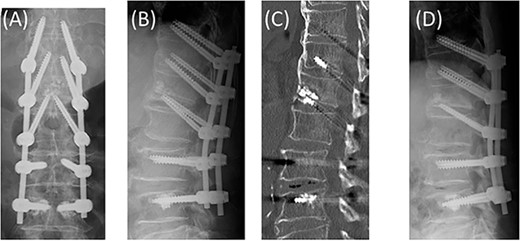
Vertebroplasty with hydroxyapatite grafting on the L1 vertebra via the DEPS trajectory from the L2 vertebra. The DEPS technique to T12, L1, and L2. Conventional pedicle screws to L3 and cement-augmented fenestrated pedicle screws to L4 (A, B, C). No screw loosening or kyphosis progression at 6 months postoperatively (D).
Postoperatively, the back pain improved, and external fixation using a frame-type thoracolumbar corset was also performed for 6 months. No screw loosening or kyphosis progression was noted at 6 months postoperatively (Fig. 2D).
Discussion
The current case demonstrates the following two points:
First, in a vertebral fracture at the caudal end of DISH, vertebroplasty via the DEPS trajectory shortened the posterior fixation range. DISH-related vertebral fractures are increasing with the progress of an aging society [10–12]. Moreover, a high prevalence of surgical complications is reported [2]. DISH fractures often require posterior spinal fixation at least three levels above and below the fractured vertebra because stress concentrates on the fractured site, causing instability [1–3]. PESs provide a stronger torque force than conventional pedicle screws, and their use in the fixation of ankylosed vertebrae reduces the amount of bleeding, fixation range, and screw loosening [4, 5]. In addition, double-endplate penetration is more favorable than single-endplate penetration [6]. Vertebroplasty, augmenting the anterior vertebral body with void fillers such as hydroxyapatite, and posterior fixation with pedicle screws is effective for maintaining spinal alignment without segmental fusion [7]. Grafting is often performed via a transpedicular trajectory, indicating the difficulty of inserting PESs into the fractured vertebra. However, by grafting via the DEPS trajectory, PESs can be inserted into the fractured vertebra, which is expected to reduce fixation range (Fig. 3B). To our knowledge, this is the first case of DISH caudal vertebral fracture treated with vertebroplasty via the DEPS trajectory.
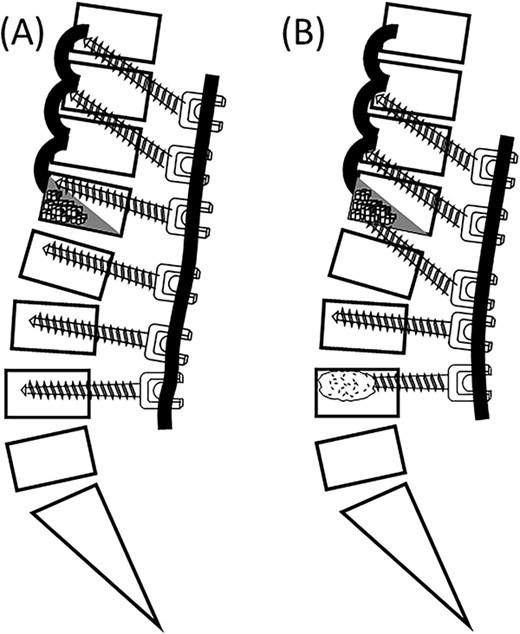
Vertebroplasty via transpedicular trajectory. The DEPS technique to the cranial vertebrae and conventional PPS to the caudal vertebrae (A). Vertebroplasty via the DEPS trajectory. The DEPS technique to the cranial vertebrae and cement-augmented fenestrated pedicle screws to the caudal end vertebra (B).
Second, inserting screws with the DEPS technique to the cranial vertebrae, with the conventional pedicle screw to the caudal vertebrae, and with cement-augmented fenestrated pedicle screws to the caudal end vertebra balances the posterior fixation force. It has been reported that patients with a vertebral fracture at the caudal end of DISH are treated with the DEPS technique to the cranial vertebrae and with conventional percutaneous pedicle screws (PPS) inserted into the caudal vertebrae [6]. However, it can result in an imbalance between cranial and caudal fixation forces (Fig. 3A). Cement-augmented fenestrated pedicle screws have been reported to provide a higher fixation force than conventional pedicle screws [8, 9]. The imbalance between cranial and caudal fixation forces can be solved using cement-augmented fenestrated pedicle screws (Fig. 3B). To our knowledge, there have been no reports of vertebral fractures at the caudal end of DISH treated with this strategy. Backout of the screws was not observed, leading to a favorable postoperative outcome 6 months after surgery.
In conclusion, in a vertebral fracture at the caudal end of DISH, vertebroplasty via the DEPS trajectory can augment the anterior vertebral body. Inserting screws with the DEPS technique to cranial vertebrae, with the conventional pedicle screw to caudal vertebrae, and with cement-augmented fenestrated pedicle screws to the caudal end vertebra solves the imbalance between cranial and caudal fixation forces. The same strategy can be applied to spinal metastases that occur at the caudal end of the DISH. However, these findings were based on a single case report, and long-term follow-up is necessary.
Conflict of interest statement
None declared.
Funding
This work was supported in part by Grants-in-Aid for Research from the National Center for Global Health and Medicine (23A 3002).
Data availability
All data found about this case are included in this published article.



