-
PDF
- Split View
-
Views
-
Cite
Cite
Badhaasaa Beyene Bayissa, Ayantu Mekonnon Borena, Transverse colon and omental incarceration in femoral hernia: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 9, September 2023, rjad496, https://doi.org/10.1093/jscr/rjad496
Close - Share Icon Share
Abstract
A femoral hernia is one of the groin hernias with a high chance of incarceration and strangulation due to its narrow neck. Here, we report a case of transverse colon incarceration. A 65-year-old female patient presented with groin mass that failed to reduce and a dragging pain. Elective open femoral herniorrhaphy was done with the finding of viable incarcerated massive momentum along with transverse colon. Femoral hernias have a female-to-male ratio of about 10:1. Postmenopausal, increasing age, and constipation were some of the risk factors identified in our patient. Various types of organs can be found in the femoral hernia sac but one of the rarely reported organ was found in our case: a transverse colon. Femoral hernia with a large bulky soft mass can get incarcerated easily but relatively less prone to strangulation.
Introduction
Femoral hernia is a protrusion of the peritoneal sac that contains preperitoneal fat, abdominal, or pelvic mass through the femoral ring into the femoral canal inferior to the inguinal ligament [1]. It is bounded laterally by the femoral vein, anteriorly by the inguinal ligament, medially by the lacunar ligament, and posteriorly by the pectineal ligament. [2] The common contents of the femoral hernia sac are preperitoneal fat, omentum, and small intestine, but exceptionally, a case report written more than a century ago mentioned the presence of transverse colon and cecum within a huge sac [3]. The contents of the sac are rarely found to be appendix (De Garengeot’s hernia), bladder, Meckle’s diverticulum, ectopic testis, stomach and fallopian tube, cecum, sigmoid, ovary, uterus, gallbladder, kidney, stomach, and liver [4–6].
Femoral hernias account for about 2%–4% of groin hernia repairs. Despite their low incidence, they need urgent or emergent intervention once diagnosed as they often present with incarceration or else with strangulation, which demands emergency surgery and sometimes bowel resection, resulting in increased morbidity and mortality [7]. Herewith, we report one of the rarest presentations of a femoral hernia with a slightly large size and nonobstructed but incarcerated transverse colon along with omentum. The case is reported in line with the SCARE guideline [8].
Presentation of the case
A 65-year-old multipara women presented with a groin mass of 2-year duration. She noticed it as a small painless bulge that used to disappear in a lying position, but during the last 2 months of her presentation, it failed to reduce. She had been feeling pressure symptoms and abdominal discomfort while walking and straining. She has been chewing chat two to three times per week for more than 20 years. She also had a history of constipation. She has no history of trauma, previous surgery, or known chronic illness. Physical examination showed a BP of 135/80, PR75, RR 18, and a BMI of 18.4. Abdominal examination revealed a 6 × 4 cm irreducible soft, nontender mass inferior to right inguinal ligament (Fig. 1). Bowel sound was audible from the mass. Ultrasound has confirmed the diagnosis of a femoral hernia. Other routine and baseline tests showed normal results. A diagnosis of incarcerated femoral hernia was made, and patient was prepared for elective herniorrhaphy.

Femoral hernia in a 65-year-old female patient (arrow showing a bulky mass inferior to inguinal ligament with a normal overlying skin).
Under spinal anesthesia, trans-inguinal approach was made, and the hernia neck was visualized but difficult to reduce from that point. For this reason, infra-inguinal extension was made subcutaneously and the sac was approached, and the adherent sac was dissected and opened. The finding showed an incarcerated omentum and part of the transverse colon in the hernia sac with few adhesions otherwise viable (Fig. 2). Part of the incarcerated omentum was resected out as it was difficult to reduce in-mass. Then, the transverse colon reduced back safely to the abdominal cavity. High ligation of the sac and fixing of the pectinet ligament to the inguinal ligament were performed with an interrupted non-absorbable suture. The posterior wall of the inguinal floor was reconstructed and the inguinal ligament was strengthened to conjoin the tendon for prophylaxis purpose. The operation was performed by a consultant surgeon in a government hospital.
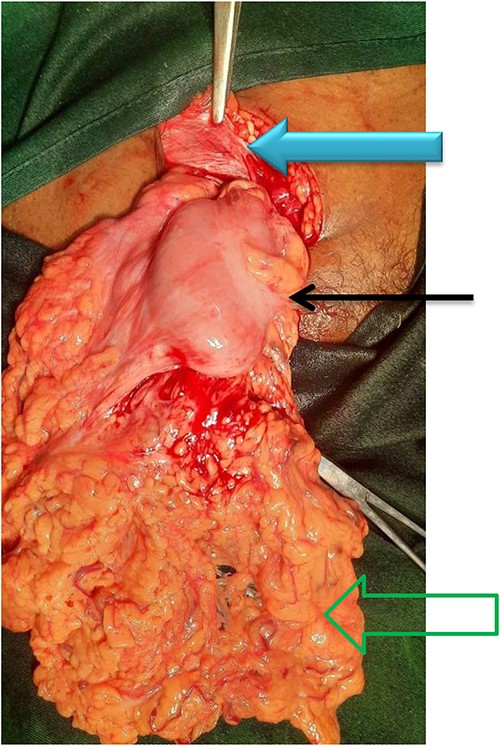
The content of the sac along with its contents (green open arrow shows viable omentum, black solid arrow shows transverse colon, and solid blue arrow shows an inguinal ligament).
The patient had stayed uneventful, smooth post-operative course, and was discharged on the third post-operative day. Follow-ups at 2 weeks, 4 weeks, and 4 months were smooth, and there was no recurrence.
Discussion
Lifetime occurrence of a groin hernia is 27%–43% in men and 3%–6% in women. Femoral hernias occur less commonly than inguinal hernias and typically account for about 3% of all groin hernias. While inguinal hernias are still the most common regardless of gender, femoral hernias have a female-to-male ratio of about 10:1 [9].
Patients between 0–5 years and 75–80 years constituted the two dominant groups for inguinal hernia repair. By contrast, the age-specific prevalence of femoral hernia repair increased steadily throughout life, peaking at age 80–90 years in both men and women [10].
The incidence of femoral hernia increases during the postmenopausal period as a result of several factors: being multiparous, factors increasing intra-abdominal pressure like smoking, COPD, ascites, constipation, and collagen vascular diseases [11]. Chronic constipation which is probably attributed to Khat chewing, a green leaf known to cause constipation [12], age, and being multiparous are some of the risk factors identified in our patient.
Different contents in femoral hernias have been reported in the literature, such as appendix, small intestine, omentum, bladder, Meckel’s diverticulum, ectopic testis, stomach [13], and transverse colon. The later one is reported only once in the literature by Catellani [3] and isolated transverse colon incarceration has never been reported to the best of our knowledge. We presented the later type along with adherent omentum to the hernia sac having a bulky mass which had a wider neck. These types of contents are relatively less prone to strangulation, but repair has to be done as soon as the diagnosis was made because delay in intervention might lead to strangulation and increase complications, such as bladder and intestinal perforation, abdominal wall and pelvic abscesses, Fournier’s gangrene, and urinary and intestinal fistulas to the skin, vagina, and scrotum [7, 14] that increase in-hospital patient mortality by 7-fold [15].
The management of femoral hernia has recently been popularized with mesh repair even though tissue repairs are being practiced in different setups and conditions as an option of repair [16]. We used pure tissue repair as we could not get mesh at the time of the planned surgery.
Conclusion
Even if femoral hernia has an increased risk of strangulation and incarceration, larger hernia with bulky structures in its side like transverse colon along its omentum has lesser rates of complications. However, regardless of their content, all femoral hernias should be managed as an urgent or emergent condition.
Acknowledgements
We express our heartfelt gratitude to our families and to those who helped us through the long journey of medical school and practice. We also acknowledge our patient for her willingness to publish her case.
Author contributions
B.B.B.: conceptualization, acquired the data, and written the original draft of the case report. A.M.B.: methodology, written the manuscript, involved in literature review, and edited the final manuscript. Both authors read and approved the final manuscript for publication.
Conflict of interest statement
None declared.
Funding
None declared.
Ethics statement
Ethical approval was waived by our Institutional health research ethics review committee (IHRERC).
Consent
Written, signed, and informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Guarantor
Dr Badhaasaa Beyene.



