-
PDF
- Split View
-
Views
-
Cite
Cite
Yingjun Gao, Yun Hui, Haibo Liu, Binyi An, Fang Liu, Pilonidal cyst of the scalp, Journal of Surgical Case Reports, Volume 2023, Issue 9, September 2023, rjad493, https://doi.org/10.1093/jscr/rjad493
Close - Share Icon Share
Abstract
A 19-year-old male patient presented with a slow-growing mass on his scalp over a 10-year history. After resecting the mass, he was diagnosed with pilonidal cyst based on the clinical and histological findings. An unusual pilonidal disease is observed on the scalp in this report.
Introduction
Pilonidal disease, including pilonidal sinus and pilonidal cyst, is a rare chronic relapsing inflammatory disease characterized by the hair inside. The disease usually occurs in the sacrococcygeal region and occasionally in many other regions, such as the interdigital, armpit, and perineum. This paper describes a rare case of pilonidal cyst of the scalp.
Case presentation
A 19-year-old male presented with a small mass on his left scalp since infancy and denied any trauma history. The tumor had gradually increased in the recent two years, accompanied by pain after strenuous exercise. It had grown to a diameter of 20 × 10 mm on admission and was soft and painful to the touch. The scalp above the tumor was covered with hair of average density, without sinus orifice and pus discharge. Surgical excision was successfully performed on the patient under local anesthesia and primary suture. Gross specimen showed the mass as cystic, containing a large amount of cloudy fluid and hair (Fig. 1). Histopathologic examination of the specimen showed inflamed granulation tissue with scattered foreign body giant cells (Fig. 2).

Gross specimens showed the mass as cystic, containing abundant hair.
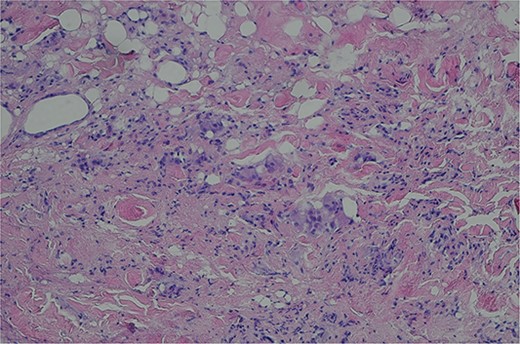
Histopathologic examination of the specimen showed inflamed granulation tissue with scattered foreign body giant cells (H&E; ×200).
Discussion
Pilonidal disease is typically found in the sacrococcygeal region, but rare cases have been reported at other sites. It is curious that the scalp, which displays the highest hair density, is not the most common site of this disease. To our knowledge, only six examples of pilonidal disease on the scalp appear in the English language literature. Among them, four cases were located in the occipital area [1–4], and two were in the post-auricle area [5, 6] (Table 1).
| Authors . | Year . | Age, gender . | Localization . | Sinus orifice . | Etiologic factor . | Recurrence/time . | |
|---|---|---|---|---|---|---|---|
| Acquired (trauma or surgery) . | Congenital . | ||||||
| Moyer DG | 1972 | 13, M | Occipital area | + | + | No/6 months | |
| Kosaka M et al. | 2007 | 4, M | Occipital area | + | + | No/1 year | |
| Chiu MW et al. | 2008 | 70, F | Occipital area | Unclear | + | Unclear | |
| Ak Nalbant O et al. | 2011 | 31, M | Post-auricle area | + | Unclear | No/5 months | |
| Kansal A et al. | 2016 | 42, F | Post-auricle area | + | + | No/6 months | |
| El Mehdi M et al. | 2022 | 4, F | Occipital area | + | + | Unclear | |
| Present case | 2022 | 19, M | Occipital area | − | + | No/5 months | |
| Authors . | Year . | Age, gender . | Localization . | Sinus orifice . | Etiologic factor . | Recurrence/time . | |
|---|---|---|---|---|---|---|---|
| Acquired (trauma or surgery) . | Congenital . | ||||||
| Moyer DG | 1972 | 13, M | Occipital area | + | + | No/6 months | |
| Kosaka M et al. | 2007 | 4, M | Occipital area | + | + | No/1 year | |
| Chiu MW et al. | 2008 | 70, F | Occipital area | Unclear | + | Unclear | |
| Ak Nalbant O et al. | 2011 | 31, M | Post-auricle area | + | Unclear | No/5 months | |
| Kansal A et al. | 2016 | 42, F | Post-auricle area | + | + | No/6 months | |
| El Mehdi M et al. | 2022 | 4, F | Occipital area | + | + | Unclear | |
| Present case | 2022 | 19, M | Occipital area | − | + | No/5 months | |
| Authors . | Year . | Age, gender . | Localization . | Sinus orifice . | Etiologic factor . | Recurrence/time . | |
|---|---|---|---|---|---|---|---|
| Acquired (trauma or surgery) . | Congenital . | ||||||
| Moyer DG | 1972 | 13, M | Occipital area | + | + | No/6 months | |
| Kosaka M et al. | 2007 | 4, M | Occipital area | + | + | No/1 year | |
| Chiu MW et al. | 2008 | 70, F | Occipital area | Unclear | + | Unclear | |
| Ak Nalbant O et al. | 2011 | 31, M | Post-auricle area | + | Unclear | No/5 months | |
| Kansal A et al. | 2016 | 42, F | Post-auricle area | + | + | No/6 months | |
| El Mehdi M et al. | 2022 | 4, F | Occipital area | + | + | Unclear | |
| Present case | 2022 | 19, M | Occipital area | − | + | No/5 months | |
| Authors . | Year . | Age, gender . | Localization . | Sinus orifice . | Etiologic factor . | Recurrence/time . | |
|---|---|---|---|---|---|---|---|
| Acquired (trauma or surgery) . | Congenital . | ||||||
| Moyer DG | 1972 | 13, M | Occipital area | + | + | No/6 months | |
| Kosaka M et al. | 2007 | 4, M | Occipital area | + | + | No/1 year | |
| Chiu MW et al. | 2008 | 70, F | Occipital area | Unclear | + | Unclear | |
| Ak Nalbant O et al. | 2011 | 31, M | Post-auricle area | + | Unclear | No/5 months | |
| Kansal A et al. | 2016 | 42, F | Post-auricle area | + | + | No/6 months | |
| El Mehdi M et al. | 2022 | 4, F | Occipital area | + | + | Unclear | |
| Present case | 2022 | 19, M | Occipital area | − | + | No/5 months | |
Pilonidal disease includes pilonidal sinus and pilonidal cyst. Pilonidal sinus usually has an orifice, from which discharge of pus can be observed in some cases, whereas pilonidal cyst does not have these characteristics. Five previously reported cases have a definite sinus orifice [2–6], and one is not mentioned [1]. In this case, no sinus orifice was found in either physical or imaging examination, so it belongs to the pilonidal cyst, which is relatively rare in pilonidal disease.
The etiology of pilonidal disease is still unclear, and there are two theories, congenital and acquired, which are still controversial. According to the literature records, acquired pilonidal disease accounts for the majority, and congenital causes should be considered in the etiology if there is no trauma or surgery history and the mass is present for a long time or since birth. Among the previously reported cases, five have a history of trauma or surgery [1–4, 6], and one is unclear [5].
In summary, our case is a congenital pilonidal cyst, which is unique among all reported pilonidal diseases of the scalp. Although this disease is rare in the scalp, the differential diagnosis of the subcutaneous head nodule and chronic sinus should be included. There have been many studies on the pathogenesis and surgical techniques of pilonidal disease, but how to further reduce the misdiagnosis rate and postoperative recurrence rate still needs continuous exploration.
Conflict of interest statement
The authors declare no competing interests.
Funding
None.
Data availability
All data found about this case are included in this published article.
Author contributions
Yingjun Gao (Literature search, wrote and approved the final submitted version), Yun Hui (Literature search, wrote and approved the final submitted version), Haibo Liu (Concept, design, Clinical management and diagnosis, edited and approved the final submitted version), Binyi An (Concept, design, Clinical management and diagnosis, edited and approved the final submitted version), and Fang Liu (Concept, design, Clinical management and diagnosis, edited and approved the final submitted version)
References
Author notes
Yingjun Gao and Yun Hui contributed equally to this work.



