-
PDF
- Split View
-
Views
-
Cite
Cite
Hirokazu Matsushima, Morihiro Katsura, Masafumi Ie, Yoshimitsu Fukuzato, Combined stepladder incision and Sistrunk procedure for en bloc resection of supraclavicular thyroglossal duct cysts, Journal of Surgical Case Reports, Volume 2023, Issue 8, August 2023, rjad445, https://doi.org/10.1093/jscr/rjad445
Close - Share Icon Share
Abstract
The accurate diagnosis and therapeutic strategies of thyroglossal duct cysts (TGDCs) are challenging for surgeons if the opening with exudate is far from the hyoid bone. A 7-year-old boy presented with a right supraclavicular mass and persistent pus. Ultrasonography and magnetic resonance imaging revealed the fistula to the hyoid bone. Suspecting a TGDC, we combined the stepladder incision technique and the Sistrunk procedure. The first skin incision cut through the opening in a spindle shape, and the second incision was made in the skin just above the hyoid bone. This combined technique allowed en bloc resection of the TGDC and the hyoid bone to the base of the tongue. Cervical masses are commonly encountered in surgical clinics, and even distant openings off the midline must be considered in the differential diagnosis of TGDCs. This treatment strategy is essential for preventing the recurrence of TGDCs and ensures optimal cosmetic outcomes.
INTRODUCTION
Thyroglossal duct cysts (TGDCs) are cervical masses commonly encountered in pediatric practice. Although TGDCs can occur anywhere in the thyroid gland’s migratory pathway during development, they rarely extend beyond the thyroid gland [1]. We present a case of a TGDC located in the supraclavicular region for which radical resection was performed by combining the stepladder incision and the Sistrunk procedure.
CASE REPORT
A 7-year-old boy with no previous history of disease presented to a local clinic with a painless right cervical mass persisting for 6 months. He had undergone several puncture drainages at the clinic; however, the pus exudate persisted, and he was referred to our hospital. The opening with the exudate was located on the caudal side of the thyroid cartilage, which seemed to be a slight induration to the right of the midline (Fig. 1A). Ultrasonography showed a continuous cord-like echogenic image along the hyoid muscle group from the opening to the bottom of the hyoid bone (Fig. 1B). Magnetic resonance imaging (MRI) revealed a continuous high-signal area from the fistula to the hyoid bone on T2-weighted images (Fig. 1C). The patient was diagnosed with a TGDC based on ultrasonography and MRI, and underwent a radical surgery called the Sistrunk procedure, in which the central part of the hyoid bone and the thyroglossal duct remnant were removed en bloc. In this case, the opening with the exudate was far from the hyoid bone; therefore, we used the stepladder incision technique, in which the first skin incision was made to cut through the opening in a spindle shape, and the second incision was made in the skin just above the hyoid bone (Fig. 1A). After the skin incision was made around the opening, the fistula wall was identified, and the peri-fistula area was dissected as far as possible toward the hyoid bone. The sinus tract was pulled out from the caudal incision and was traced to the foramen caecum, which included en bloc removal of the central position of the hyoid bone (Fig. 1D). A histological examination revealed pseudostratified ciliated columnar epithelium and thyroid-like follicular structures. The patient recovered and was discharged on day 3. No recurrence was observed at the 1-year follow-up, and the scars were not noticeable.
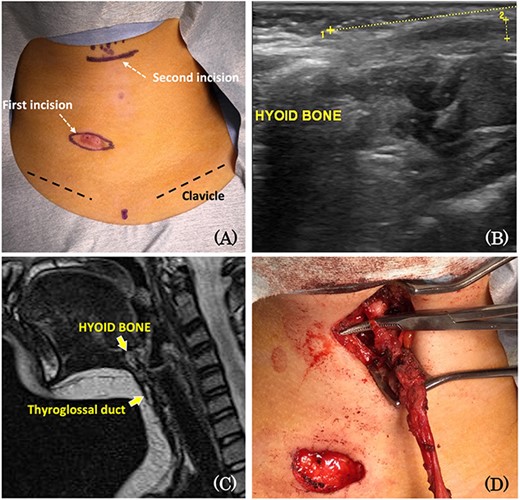
(A) The opening with the exudate was located in the caudal side of the thyroid cartilage and the right of the midline. Stepladder incision; the first skin incision was made to cut through the opening in a spindle shape, and the second incision was made in the skin just above the hyoid bone. (B) Ultrasonography showing a continuous cord-like echogenic image from the opening to the bottom of the hyoid bone. (C) MRI scan showing a continuous high-signal area from the opening with the exudate to the hyoid bone on T2-weighted images. (D) The sinus tract was pulled out from the first incision and was traced to the foramen caecum, which included en bloc removal of the central position of the hyoid bone.
DISCUSSION
Before birth, the thyroid gland descends from the foramen caecum to the anterior surface of the pharynx. The thyroglossal duct usually disappears; however, if it remains after birth, repeated local infection and inflammation can lead to TGDCs. Thus, they can form at any site in the migratory region of the primitive thyroid gland [1]. However, they rarely form in the supraclavicular or suprasternal region, as in our case [2]. It has been hypothesized that when located suprasternally, the TGDC is more likely caused by an infection extending inferiorly rather than the result of the hyperdescent of the thyroglossal duct remnant [2]. Thus, the differential diagnosis of an anterior cervical mass in children should include congenital dermoid cysts, ectopic thyroid tissue, cervical bronchogenic cysts and aberrant cervical thymus, in addition to TGDCs [2]. Furthermore, ultrasonography plays an important role in such cases.
TGDCs have a high recurrence rate after inadequate surgery [1], with ~1–2% of cysts becoming malignant [3]. Currently, the gold standard for surgical intervention is the Sistrunk procedure, with the lowest recurrence rate [1]. Post-inflammatory fibrosis has been reported to be a risk factor for recurrence, and post-inflammatory fibrosis and disease recurrence are also risk factors for worse cosmetic outcomes [4]. The stepladder incision technique for radical excision of suprasternal TGDCs has also been previously reported [2]. Thus, even if the opening with the exudate is far from the hyoid bone, like in our case, this technique can be used to ensure that the hyoid bone and TGDC are straightforwardly cored out.
In conclusion, cervical masses are common in surgical clinics; therefore, even a sinus orifice farther away from the hyoid bone or off the midline must be considered in the differential diagnosis of TGDCs. Combining the stepladder incision technique and Sistrunk procedure allows en bloc resection of the TGDCs and the central portion of the hyoid bone and further excision of a core of tissue above the hyoid bone to the base of the tongue. This treatment strategy is essential for the prevention of the recurrence TGDCs and ensures optimal cosmetic outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The authors received no financial support for the research, authorship and/or publication of this article.
DATA AVAILABILITY
Data sharing is not applicable to this article as no new data were created or analyzed in this study.



