-
PDF
- Split View
-
Views
-
Cite
Cite
Binar Burhan Abdulrahman, Jeza Muhamad Abdul Aziz, Mohammed Kak Bra Salih, Muhammad Jabar Rashid, Mohammed Latif Ahmed, Ramyar Hersh Awl, Shanga Baram Rauf, Harem Habil Hama Ali, Nguyen Tien Huy, Mariwan Kadir Rasheed, Recurrence of tuberculous tenosynovitis in wrist tendon of a butcher: rare case report, Journal of Surgical Case Reports, Volume 2023, Issue 8, August 2023, rjad353, https://doi.org/10.1093/jscr/rjad353
Close - Share Icon Share
Abstract
Diagnosing of tuberculous arthritis can be challenging due to its insidious onset and non-specific clinical presentation. A high index of suspicion is required for early diagnosis. A 54-year-old butcher was admitted to an orthopedic clinic with complaints of pain, paresthesia and an enlarging mass in the left wrist, which limited finger flexion. Initially the patient was diagnosed with carpal tunnel syndrome (CTS); the patient had no history of tuberculosis (TB), but had direct contact with animals. On clinical examination, a small mass was found in the distal volar region of the forearm and no lymphadenopathy was observed. Despite the diagnosis the patient refused to receive TB treatment. After a period of 4 months, the patient once again exhibited symptoms of CTS. This case highlights the importance of considering TB as a potential etiology for persistent symptoms of carpal tunnel surgery. Early diagnosis and prompt initiation of TB treatment can result in favorable outcomes and can prevent future recurrence.
INTRODUCTION
The most deadly infectious illness is tuberculosis (TB), which claims the lives of nearly 2 million people each year. The World Health Organization ranks it as the fourth largest avoidable cause of mortality in underdeveloped nations. While pulmonary TB is the most common form of the illness seen in clinical settings. Nonetheless, extrapulmonary TB accounts for 10–20% of occurrences in immunocompetent persons and for 60% of cases in immunocompromised patients at the present time [1].
TB can affect the extremities and has become an extremely uncommon illness, particularly in industrialized regions. Despite this, there have been reports of post-operative chronicity as well as recurrence tendencies following surgery [2].
The compound palmar ganglion is another name for tuberculous tenosynovitis of the wrist, though ganglion is a misnomer. It makes up 5% of the overall infection of the bone and joint TB. At a far later stage, it begins to show long-lasting swelling, dull aching pain and a few other symptoms. The ulnar or radial bursae of the hand are the most often affected areas [3].
TB infections of the hand and wrist are uncommon. The diagnosis of the involvement of the hand and wrist may be challenging due to the rarity of tuberculosis and the overlap of symptoms with other diseases [4]. We describe a recurrence of tuberculous tenosynovitis in the wrist of a butcher man.
CASE REPORT
A 54-year-old butcher man was presented to the orthopedic clinic with 1-year history of pain, paresthesia and enlarging mass of the left wrist and palm. It was associated with the limitation of finger flexion. Operated with carpal tunnel syndrome (CTS) and diagnosed with tuberculous tenosynovitis, however, the patient refused to receive TB treatment. After a period of 4 months, the patient once again exhibited symptoms of CTS. As he had pain and paresthesia in the distribution of the median nerve in the hand, continuously, the patient awoke with burning pain, tingling and numbness. Then, the patient received treatment (rifampin, isoniazid and pyrazinamide), which led to symptomatic improvement. After 6 months of TB treatment, the patient was asymptomatic, and at the 1-year follow-up, there was no evidence of recurrence The patient has not any history of TB and also has not had any contact with any person with TB, but as he is a butcher and has direct contact with animals. However, he had no history of night sweats, weight loss, cough, hemoptysis or dyspnea.
During an inspection, a tiny mass was found to be located over the distal side of the volar region of the forearm. While the axillary and supra-trochlear lymph nodes were examined, the results were normal, and there was no evidence of lymphadenopathy when the patient was palpated.
The patient exhibited signs and symptoms of CTS, and he also had mass in the wrist joint. The electrodiagnostic test revealed that nerve conduction has slowed down across the wrist, and the ultrasound revealed that there was swelling of soft tissue over the distal side of the forearm, with the possibility of a ganglion developing over the median nerve of the left wrist, which is known as compound palmar ganglion, Laboratory values showed that the C-reactive protein (CRP) and erythrocyte sedimentation rate were high. Tenosynovectomy was done under general anesthesia (Fig. 1), and the orthopedic surgeon removed the mass that invaded the median nerve, distal flexor tendons and expansion to the metacarpophalangeal joint (Fig. 2). The mass was excised and was sent for histopathological examination (HPE) and culturing, which revealed a cyst wall, thickened synovial lining, numerous epithelioid granulomas, multiple giant cells and foci of caseating granulomatous inflammation, which are highly suggestive of tuberculous tenosynovitis and negative for malignancy. The acid-fast stain indicated high bacilli bacteria, and a 4-week culture showed Mycobacterium tuberculosis. Amoxicillin, 1-mg vial, for 4 days, and TB treatments (rifampin, isoniazid and pyrazinamide) for 1 month improved the lesions. He was asymptomatic after 6 months of TB treatment. One year after surgery, there was no evidence of recurrence.
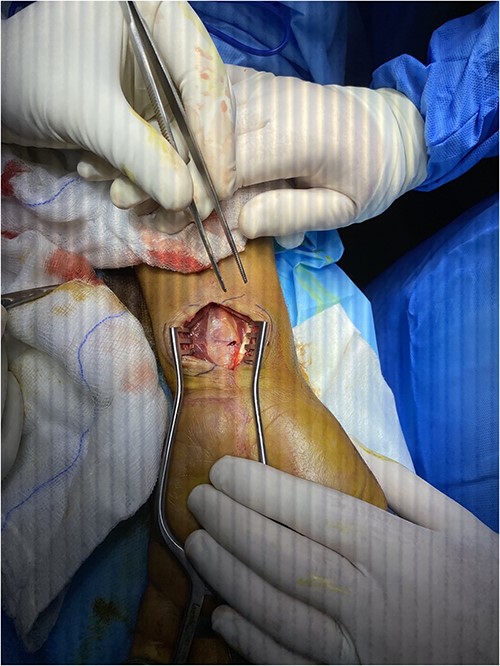

The mass that invaded the median nerve, distal flexor tendons and expansion to metacarpophalangeal joint.
DISCUSSION
TB infections, which are spread by aerosolized germs, often appear as pulmonary presentations. Rarely, the hematogenous spread of TB might have an impact on the musculoskeletal system. Only 1–5% of TB patients, according to prior research, had musculoskeletal symptoms that have been reported. The majority of cases of osteoarticular TB affect the main weight-bearing joints, with the lumbar vertebral bodies being the most frequent location, followed by the hips and then the knees [4, 5]. In the current case, the TB tenosynovitis was present in the wrist joint. There are very few cases of TB of the synovial sheath of the flexor tendons of the hands involving the radial or ulnar bursa [3].
The gold standard for diagnosing of tuberculous arthritis is the isolation of M. tuberculosis from synovial fluid, tissue biopsy or culture. However, these tests have a low sensitivity and can take weeks to obtain results [6]. In the presented case, the diagnosis was made based on the HPE of the excised mass, which revealed typical features of tuberculous tenosynovitis; acid-fast stain and culture confirmed the diagnosis.
Most individuals with tenosynovitis are over the age of 60, and the condition manifests itself as an insidious, slow-growing mass that resembles a sausage along the tendon that is inflamed tendon. In most cases, pain and restricted movement are the subsequent symptoms to appear, followed by erythema and warmth in the affected region. Sometimes, the mass puts pressure on the median nerve, which results in a condition that is similar to CTS [4]. The clinical picture of the present case was quite general and the cause of the inflammation was unknown. Males, particularly those working in agricultural or labor-intensive industries or who are involved in animal care, are more likely to be impacted. There are two ways that tuberculous tenosynovitis can arise: by the hematogenous spread of infection from a focal center of infection, or through direct injection from surrounding diseased tissue [7]. The present case was of a butcher who had contact with animals and was suspected to be infected from infected animals.
More than 50% of cases with TB tenosynovitis return within 1 year of therapy, indicating that this condition has a propensity for local recurrence [8]. The current case report recurrence of tuberculous tenosynovitis in the wrist tendon, who had previously been diagnosed. CTS may occur from the mass impact caused by wrist tenosynovitis in the already restricted flexor compartment around the wrist [9]. Our patient underwent a surgery for carpal tunnel and confirmed TB infection 4 months ago, but he refused antitubercular therapy. Possible reasons for recurrence, including inadequate treatment, poor compliance and drug resistance, but concluded that the cause could not be definitively determined. They recommended that patients with tuberculous tenosynovitis be followed closely after treatment to monitor for recurrence.
CONCLUSION
This case highlights the importance of considering TB as a potential etiology for persistent symptoms following carpal tunnel surgery, particularly in patients with occupational contact with animals. Early diagnosis and prompt initiation of TB treatment can result in favorable outcomes and can prevent a recurrence; and the pathologist and microbiologist must be consulted to diagnose tuberculous tenosynovitis. It is crucial to closely monitor and follow up patients with tuberculous tenosynovitis after successful treatment.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
The authors confirm that this study was prepared by COPE rules and regulations. The manuscript was approved by the ethical committee of Baxshin Research Center (BRC0200423) dated 1 February 2023.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review from the editor of this journal.
GUARANTOR
All authors have read and approved the manuscript; on behalf of all the contributors, I will act as guarantor and will correspond with the journal from this point onward.



