-
PDF
- Split View
-
Views
-
Cite
Cite
Sang Ho Oh, Yeong Sik Yun, A large fibrotic nodule on the A1 pulley with severe tenosynovitis after repetitive prolotherapy in trigger finger: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 8, August 2023, rjad089, https://doi.org/10.1093/jscr/rjad089
Close - Share Icon Share
Abstract
Prolotherapy is used to treat chronic musculoskeletal diseases. The efficacy of prolotherapy was recently acknowledged. However, it has not been usually used to treat trigger fingers. Our study was a case report of aggravated flexor tenosynovitis and a fibrous nodule on thickened A1 pulley after repetitive prolotherapy for treating the trigger finger. A 47-year-old electrical engineer complained of a locked and painful triggering in his right ring finger. Preoperative ultrasonography revealed a large hyperechoic mass on the A1 pulley and tenosynovitis. Mass resection and tenosynovectomy were performed. The histological examination revealed a benign fibrous nodule without inflammatory cells. There were no complications at 6 months post-operative, and the patient regained a full range of motion. Reducing inflammation around the flexor tendon and A1 pulley was the most important strategy for the non-surgical management of the trigger finger.
INTRODUCTION
Trigger finger, also known as stenosing flexor tenosynovitis of A1 pulley, affects adult population in the USA with a lifetime prevalence of 2% [1]. It causes painful triggering during finger movements or locking of the digit. Usually, it occurs mainly on dominant side, mostly on thumb and ring finger [2, 3]. Various conservative treatments, including extracorporeal shock wave therapy, corticosteroid injection and platelet-rich plasma therapy, were recently studied for treating trigger fingers, and steroid injection remain the most widely used conservative treatment [4, 5]. Steroid injection has a success rate of ~64% in treating the trigger finger [4]. An operative technique was usually performed for recurrent cases that did not improve with conservative treatment [2].
Prolotherapy is a used treatment that promotes reconstruction of tissues, such as weakened ligaments and tendons, by inducing proliferation of new cells, including platelet-rich plasma or stem cell therapy [6]. According to the mechanism of prolotherapy, it was used for chronic musculoskeletal diseases, for example, epicondylitis, Achilles tendinopathy, osteoarthritis, etc. However, there is no consensus on using prolotherapy for the treatment of hand diseases except osteoarthritis.
There are not any published reports on the use of prolotherapy for treating trigger fingers. In this article, we describe our experience in treating a patient with a fibrotic nodule and severe tenosynovitis, who received repeated prolotherapy for trigger finger.
CASE REPORT
In an institutional review board-approved case report, a 47-year-old male electrical engineer visited our hospital with a right ring finger (RRF) that was painfully triggering and locked in the morning as well as with swelling around the A1 area.
Before visiting our hospital, he went to another orthopedic clinic and had repetitive prolotherapy sessions on his RRF for 16 times to manage the simple, mild triggering symptoms without pain in the morning, which resolved in afternoon. His symptoms did not improve during prolotherapy, however, he received full-time prolotherapy. After the end of prolotherapy, no improvement or aggravation in symptoms of trigger finger was observed. In our clinic, we discovered a fixed extension position (extension contracture) with severe pain when the examiner pushed the patient’s ring finger volarly. Furthermore, patient complained of swelling and tenderness in A1 area.
Plain radiography revealed no abnormalities: 1.5 cm-sized hyperechoic mass without vascular invasion above thickened A1 pulley of RRF was observed on ultrasonography. There was severe tenderness around A1 pulley area as well as triggering of flexor tendon during passive flexion and RRF extension (Fig. 1).
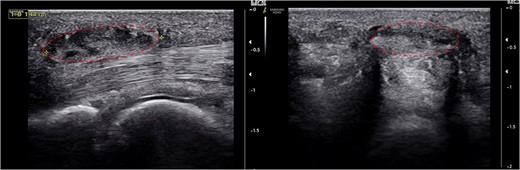
About 1.5 cm-sized hyperechoic mass (dotted circle) around the thickened A1 pulley and flexor tenosynovitis was detected.
During the operation, the 1.5 cm-sized mass was excised through the longitudinal incision on A1 pulley area. This mass was well defined and encapsulated, and it was tightly attached to the A1 pulley (Fig. 2). There was severe tenosynovitis around flexor tendon and severe adhesion between flexor digitorum superficialis and profundus. Extensive tenosynovectomy around and between flexors was performed. Flexor tendon had a severe splitting lesion (Fig. 3). We considered the possibility of tuberculosis tenosynovitis and performed mycobacterial culture and biopsy. However, histological examination revealed a simple benign fibrous nodule, and there was no evidence of tuberculosis infection.
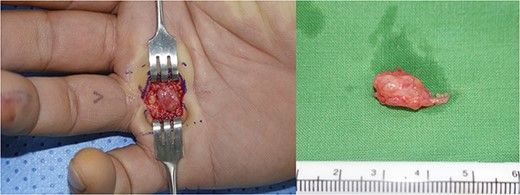
The encapsulated mass was excised through a longitudinal incision; the mass was surrounded with inflammatory tissue.

(A) Severe inflammatory tenosynovitis and adhesion around the flexor tendon was observed; (B) A longitudinally split flexor superficialis tendon lesion with tenosynovitis was observed.
The patient’s post-operative course was favorable. There were no signs of recurrence or infection during the 6-month post-operative follow-up. Follow-up ultrasonography was performed during outpatient clinic visits at 1, 3 and 6 months after operation. One month after operation, mild swelling of the operative site and tenderness were observed; however, ultrasonography revealed that there were no problems with flexor tendon gliding, recurrence of mass lesion or tenosynovitis. We encouraged patients’ scar massage and range of motion. All complaints were resolved 3 months after the operation. During 6-month post-operative follow-up, full range of motion was observed without any complications (Fig. 4).

The appearance after 6 months post-operative showed a full range of motion without complications or symptoms.
DISCUSSION
Prolotherapy has recently been used to treat chronic musculoskeletal diseases. Musculoskeletal condition is the most common reason for patients to visit their clinics in USA [7, 8]. Prolotherapy was recently acknowledged for its effectiveness, and it was widely used for treating lateral epicondylitis, Achilles tendinopathy, osteoarthritis, temporomandibular joint (TMJ) disease, etc. [7].
The main mechanism of prolotherapy is paradoxical treatment method that induces regeneration by further causing acute inflammation where there is a painful lesion. After injection of a stimulating element, the secondary healing process for musculoskeletal pathology was induced, and fibroblast was the most essential cell during the process. It makes abundant collagen around the lesion, resulting in a stronger and thicker ligament, increased stability and pain relief, and this process heals tendinopathy. Because the tendinopathies, such as lateral epicondylitis, Achilles tendinopathy and TMJ disease, are non-inflammatory painful degenerative pathologies, therefore, prolotherapy, a treatment that induces a new inflammatory response, is widely used as a good method [9].
In this article, the patient visited our clinic due to a painful and locked digit during the flexion, with swelling around A1 area. On preoperative ultrasonography, there were large non-cystic mass lesions and severe tenosynovitis. The patients experienced significantly worsened symptoms after repeated prolotherapy. After mass excision and A1 pulley release with tenosynovectomy, histological examination of excised mass revealed a benign fibrotic nodule with tenosynovitis.
The mechanism of prolotherapy induced new inflammatory response on the tendon and ligament pathology; however, because trigger finger is an inflammatory tenosynovitis, prolotherapy can worsen the inflammation. Additionally, repeated injection and injection trauma around A1 pulley cause more inflammation and fibroblast activity. It differed from the original mechanism of prolotherapy, which made a new inflammatory response to non-inflammatory degenerative pathology. Trigger finger occurred due to disproportion between the A1 pulley and flexor tendon; recurrent prolotherapy and recurrent injection trauma cause worse tenosynovitis and thicker A1 pulley due to fibroblast activation; and finally, it can create a fibrotic nodule. It did not contain any inflammatory cells. It probably has passed the inflammation phase, and the fibrotic nodule was a product of resolving inflammation.
There are no case reports of using prolotherapy for tendinopathy of the fingers yet. In this article, a case of a benign fibrous nodule on the flexor sheath and severe flexor tenosynovitis that occurred after repeated prolotherapy was reported. It was the first prolotherapy case for treating stenosing tenosynovitis of fingers (trigger finger). We believe that reducing inflammation around flexor tendon was the most important strategy for the non-surgical management of trigger finger.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The authors have no proprietary or commercial interests regarding any of the materials discussed in this article.
DATA AVAILABILITY
The data set used in this article will be made available on request from Sang Ho Oh (fwmesser@hanmail.net).
DECLARATION OF ETHICAL APPROVAL FOR STUDY
Institutional Review Board of Korea National Institute for Bioethics Policy approved this case report (No. KoNIBP-P01-202203-01-033).
DECLARATION OF INFORMED CONSENT
Patients provided informed consent for the publication of the clinical photographs included in this article.



