-
PDF
- Split View
-
Views
-
Cite
Cite
Marco Tozzi, Andrea Gobbo, Alvaro Yebes, Bogdan Spiridonescu, Rados Djinovic, The dire consequences of multiple failed hypospadias repairs: a case report of a cavernosal reconstruction with mesh and malleable prosthesis, Journal of Surgical Case Reports, Volume 2023, Issue 7, July 2023, rjad430, https://doi.org/10.1093/jscr/rjad430
Close - Share Icon Share
Abstract
The management of hypospadias during the neonatal period should be carried out exclusively in specialized medical centers because of the potential dire complications that may arise. In this report, we present a case of a 22-year-old male who underwent thirteen unsuccessful surgical procedures for his penoscrotal hypospadias in various hospitals. The purpose of this case report is to describe the surgical correction of severe corporal fibrosis and penile curvature that ensued from the multiple failed hypospadias corrections. We implanted an extra cavernosal malleable penile prosthesis and reconstructed the tunica albuginea defect with surgical meshes used in hernia repairs.
INTRODUCTION
Hypospadias is a common congenital urological abnormality in male infants, characterized by a dorsally hooded foreskin, proximal urethral opening and ventral penile curvature. The SRY gene product expressed during 7–8 weeks of gestation plays a vital role in masculinization, testosterone production and regression of female structures [1]. Dihydrotestosterone becomes crucial for proper penis development during the 8–12 weeks’ gestational phase. Surgical intervention is typically recommended between 6 and 18 months of age, preferably at specialized medical centers to minimize complications [2, 3]. Hypospadias reconstruction aims to achieve a straight phallus with normal urinary and sexual function, and an esthetically pleasing appearance. Common complications after hypospadias repair include urethrocutaneous fistula, urethral diverticulum, persistent curvature and urethral stricture [4, 5]. This case report describes a challenging surgical reconstruction of a severely compromised penis following multiple hypospadias corrections.
CASE REPORT
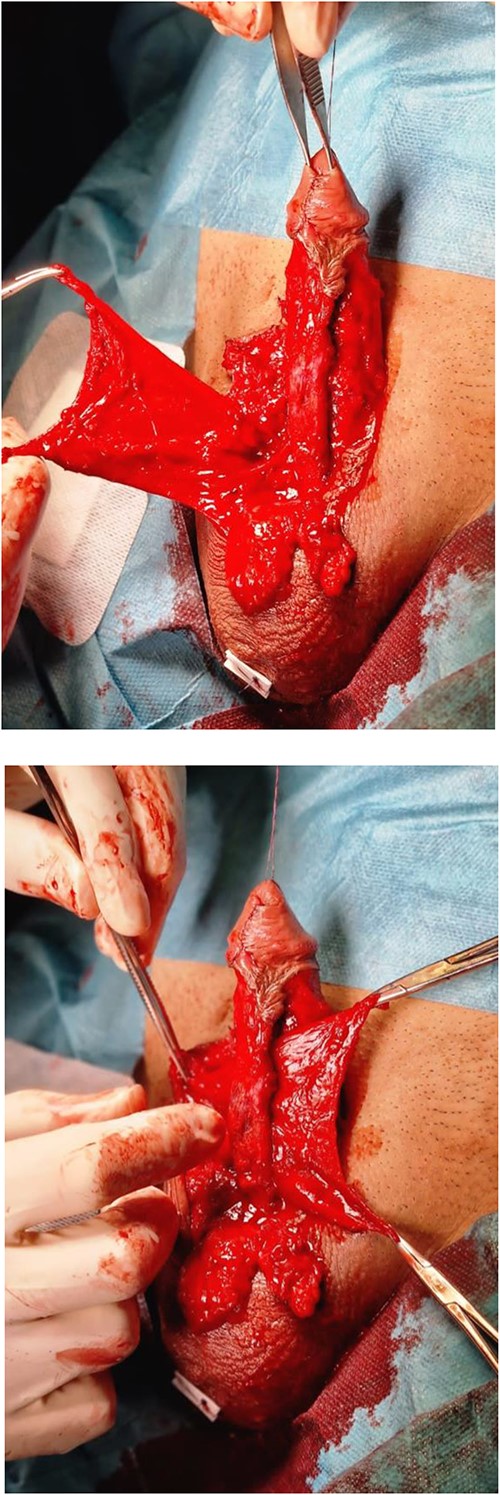
We present the case of a 22-year-old man who had undergone 13 previous surgical treatments for penoscrotal hypospadias in various hospitals. Prior to the surgery, the patient underwent dynamic Doppler ultrasound of the penis, which revealed a ventral curvature of ~90° because of significant fibrosis in the middle and distal parts of the cavernosal bodies and cavernosal erectile tissue. The peak systolic velocity measured >35 ml/s, the end-diastolic velocity was <5 ml/s, and the resistive index exceeded 0.8. Upon entering the operating room, we observed a short and retracted circumcised penis as the result of the multiple prior treatments. The penoscrotal hypospadias had already been partially resolved, resulting in distal hypospadias (Fig. 1). Hydraulic erection confirmed the findings from the Doppler ultrasound. After a longitudinal incision of the albuginea for the length of the penile shaft, we implanted a Genesis malleable penile prosthesis (Coloplast®) with a diameter of 9.5 mm and a length of 8 cm to provide stability and volume without entering the proximal cavernosal bodies. In this way, the prosthesis served as a tutor for the distal penile shaft, leaving untouched the crural portion. The prosthesis was not allocated entirely inside the penile cavernosal bodies to prevent damage to the erectile tissue. The penile implant was secured and covered on the ventral side using the polypropylene mesh Ultrapro® (Ethicon US LLC) (Fig. 2). The urethra was mobilized, and a dartos flap from the right side of the penile skin was placed between the urethra and cavernosal bodies (Fig. 3). Reconstruction of the ventral penile skin was performed using a rotation scrotal skin flap from the right side. The distal hypospadias was corrected through a traditional tubularized incised plate around a 14 Ch catheter. The patient left the operating room with two scrotal dreins, an 8 Ch urethral stent and a 10 Ch suprapubic cystostomy, which were maintained for 2 weeks. Three days after the surgery, we noticed superficial skin necrosis in a part of the flap (Fig. 4). The only treatment we administered was hydration with a local antibacterial cream three times a day. One-month post-surgery, the skin flap necrosis showed significant improvement and was nearly completely resolved (Fig. 5). The patient reported good erectile function with regular tumescence and detumescence of the cavernosal bodies, normal sensitivity of the glans and overall satisfaction with the results.

Surgically altered penis with a shortened and retracted appearance, distal hypospadias and bifid scrotum.
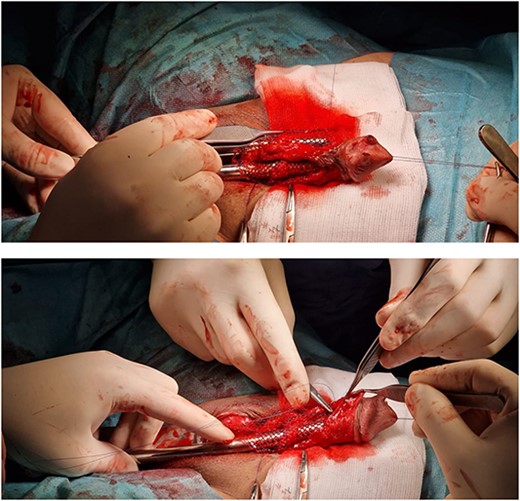
Reconstruction of the ventral side of the middle and distal cavernosal bodies using Ultrapro Mesh.
Mobilization of the urethra with a dartos flap from the right side was placed between the urethra and cavernosal bodies.

Three days after surgery: skin necrosis in the specific area of the flap.

One month post-surgery, the skin flap necrosis showed significant improvement and was nearly completely resolved.
DISCUSSION
Urologic reconstruction in repeat hypospadias surgeries presents significant challenges. Surgical reintervention should be delayed for at least 6 months after the initial repair to allow for optimal tissue healing and blood flow [4]. Our patient harbored multiple complex conditions: a recurrent ectopic urethral meatus, ventral curvature because of fibrotic tunica albuginea, unstructured corpora cavernosa and a prominent scar on the ventral side of the penis. The overall result consisted of a retracted and undersized penis with anatomical anomalies requiring a complex reconstruction using various strategies. Notably, the patient had satisfactory penile vascularization as assessed by Doppler ultrasound, and a positive response to intracavernosal prostaglandins. In our case, we implanted a small malleable prosthesis in the ventral side of the penis as long as the penile shaft, leaving the proximal corporal bodies untouched. The purpose of the implant was to act as a scaffold for the penile shaft to avoid further retraction and recurrent curvature while allowing normal erections of the corporal bodies. For this reason, we did not dilate aggressively the corpora in order to preserve the corporal arteries. The idea behind our choice is the same as postulated by Austoni et al. [6]. Their technique used soft and thin implants placed without injuring the cavernosal arteries in patients suffering from Peyronie’s disease. This approach could straighten the penis and avoid retraction while maintaining physiologic erectile tissue around the prosthesis. Polypropylene meshes have been used for many andrological conditions. They have been successfully described to increase penile girth in penile prosthetic surgery [7, 8]. Also, they have proven useful in correcting distal prosthetic migration at the glans penis level [9]. In this surgery, the mesh was necessary to cover and fix the implant because the extensive penile fibrosis and retraction prevented its positioning inside the corporal bodies. Interposing healthy vascularized tissue between the mesh and the penile spongy tissue is crucial to avoid complications such as erosion or extrusion into the penile urethra [10]. Dartos has been used as an intermediate layer similarly in other surgeries in this district [11]. This case highlights the complexity of reconstructing both the urethra and corpora cavernosa, aiming to preserve erectile function using different prosthetic devices. Our approach involving a synthetic mesh and penile prosthesis is not standard practice but an attempt to overcome the surgical difficulties unique to this case. It is essential for patients with multiple previous failed procedures to be treated by experienced reconstructive urology teams to ensure successful outcomes.
AUTHORS’ CONTRIBUTIONS
M.T., A.G. and A.Y. developed the first draft of the manuscript. All the authors revised the manuscript by refining the contents with feedback and comments. All authors have read and agreed to the published version of the manuscript.
INFORMED CONSENT STATEMENT
The patient gave written informed consent for the publication of the case history and associated images.
CONFLICT OF INTEREST STATEMENT
None declared.
DECLARATION OF ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical committee was not inquired about this case report because the patient gave full consent to the publication of his data.



