-
PDF
- Split View
-
Views
-
Cite
Cite
Khoi A Nguyen, Double free flaps for complex oromandibular defects with two teams of head and neck reconstructive surgical oncologists, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad394, https://doi.org/10.1093/jscr/rjad394
Close - Share Icon Share
Abstract
From December 2019 to July 2021, double free flaps were used by two teams of head-and-neck reconstructive surgical oncologists in 10 patients with large composite mandibulofacial defects following malignant tumor (n = 8) and osteoradionecrosis (n = 2) ablation. Our report included 10 patients. All of our patients were reconstructed by two free flaps, a combination of an anterolateral thigh flap (n = 8) or a radial forearm flap (n = 2) with an osteocutaneous fibula flap. The survival rate of these flaps was 100%. The mean operative time was 597 ± 41.7 min (range 545–660 min). There were no patients with major complications. Most of our patients had accepted functional and cosmetic results of both recipient site and donor site after a median follow-up of 22.5 months. Two teams of reconstructive surgical oncologists may shorten the operative time and reduce the rate of major complications.
Main Points:
Huge complex oromandibular defects may require the use of double free flap reconstruction.
Double free flaps were used by two teams of head-and-neck reconstructive surgical oncologists.
This approach may shorten the operative time and reduce the rate of major complications.
INTRODUCTION
The composite oromandibular defects from extensive surgical resection of advanced tumors can involve oral lining, soft tissue, bone, external skin. Reconstruction of such defects with satisfactory functional and cosmetic quality requires free tissue transfer and remains a challenge. In the cases of extensive composite resections, the defects exceed the coverage of a single free flap. There are several ways to overcome this, including simultaneously using two free flaps [1–4].
Many choices of flap combinations have been reported [5–8]. Most of these include one free osteocutaneous flap and one free myocutaneous or cutaneous flap. In this study, the free fibular osteocutaneous flap was used to provide bone for the mandible. A simultaneous anterior lateral thigh flap or radial forearm flap was used to provide intraoral lining and/or skin for the outer or soft tissue bulk.
CASE SERIES
This is a case series report. Between December 2019 and July 2021, 10 patients with extensive complex oromandibular defects underwent double flap reconstruction. We used a fibular osteocutaneous free flap for mandibular defects and oral lining, a free radial forearm flap (RFFF) or an anterior lateral thigh flap (ALT) for external face, intraoral lining and soft-tissue volume reconstruction. A two-team approach was key to these surgeries. Although the first team ablated the tumor and the cervical lymph nodes, the second harvested the fibular flap. The first team preserved and prepared the recipient vessels (facial and superior thyroid artery; the external jugular, retromandibular, facial or common facial veins, and lingual veins). Once the osteocutaneous flap was in place, the vessels were anastomosed, the second team simultaneously harvested another free flap (anterior lateral thigh flap or radial forearm flap). We performed the classic anastomosis technique, trisecting the vessel circumference with simple sutures. The flaps were monitored based on color (pink, white, marble, blue), flow (checked by handheld Doppler probe or capillary refill), temperature (warm, cold) and turgor (normal, none, tight) every 3 h for the first 48 h, then every 12 h for 5 d.

Case no. 6. (A) Intraoperative photograph of a 48-year-old man demonstrating tumor of lower–alveolar ridge invasing through the right cheek skin. Biopsy revealed the mass to be a squamous cell carcinoma. (B) The defect involved the right buccal mucosa, the mouth floor, the right mandible from the midline to the angle area and the external face skin. (C–D) Total reconstruction of all defect components was achieved with a left fibula osteoseptocutaneous flap and a left anterolateral thigh fasciocutaneous flap and (E) 6 months post-reconstruction.
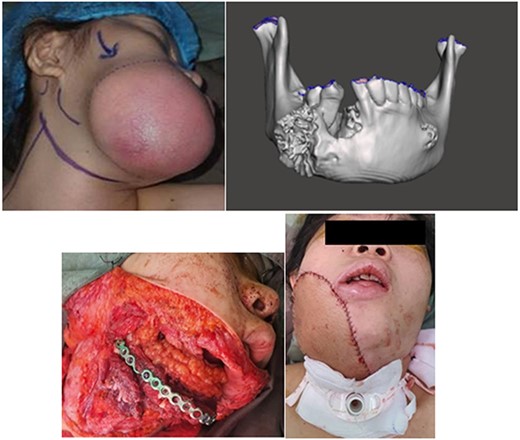
Case no. 3. (A) Preoperative photograph of a 18-year-old woman demonstrating tumor eroding through the right cheek skin. (B) CT image showing a tumor of the right mandibular bone. Biopsy revealed the mass to be a osteosarcoma. (C) Intraoperative photograph showing fibular osteocutaneous free flap used for the reconstruction of the mandibular defect as well as to provide lining for the intraoral defect. (D) The anterolateral thigh musculocutaneous free flap is used to cover the exposed fibular free flap and the external cheek defect.
Collected data included patient demographics, primary tumor site, types of post-ablative surgical defects, free-flap donor sites, operative time, surgical complications, cosmetic and functional outcomes. Data on the surgical defect involved different anatomical structures including mucosa, skin and bone. The bone defect was classified using the ‘HCL classification’ (H: hemimandibular, C: central, L: lateral) as described by Jewer et al. [3]. Complications—any unexpected surgical-related events occurring after the procedure at either donor or recipient sites—were categorised as minor or major. The patients with major complications received exploratory surgery to save the flaps. Functional results were evaluated for all 10 patients by three physicians and/or nursing staff, and each patients’ scores then averaged (rounding to the nearest whole number). The following data were recorded for all patients: speech intelligibility, quality of oral feeding, mouth opening and cosmetic outcomes at 1 and 6 months post-operatively. We used the typical postoperative Oral Function and Facial Aesthetics (OFFA) scale [9].
Our case series report included 10 patients: 5 female and 5 male. Their mean age was 41.4 ± 17.98 years (ranging from 15 to 60 years). Their double free flap reconstructions were a combination of an osteocutaneous fibula free flap with an anterolateral thigh flap (n = 8) or a radial forearm flap (n = 2). Out of our case series, five patients with squamous cell carcinoma (SCC) of the lower alveolar ridge received postoperative chemoradiotherapy (66 to 70 Gy with weekly cisplatin at a dose of 40 mg/m2) (Fig. 1). Three patients with mandibular osteosarcoma received postoperative chemotherapy (Fig. 2). The final two patients were diagnosed with mandibular osteoradionecrosis (3 and 5 years after radiotherapy for tonsil and nasopharyngeal carcinoma) (Table 1).
| Case number . | Sex . | Age . | Staging . | Site . | Pathology . | Type of bone defects . | Flap combination . |
|---|---|---|---|---|---|---|---|
| 1 | Female | 15 | T2N0M0G2 | Mandible | Osteosarcoma | LC | FFF + ALT |
| 2 | Female | 16 | T2N0M0G2 | Mandible | Osteosarcoma | L | FFF + RFFF |
| 3 | Female | 18 | T2N0M0G3 | Mandible | Osteosarcoma | HC | FFF + ALT |
| 4 | Female | 45 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | HC | FFF + ALT |
| 5 | Female | 47 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
| 6 | Male | 48 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 7 | Male | 55 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + RFFF |
| 8 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 9 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 10 | Male | 60 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
| Case number . | Sex . | Age . | Staging . | Site . | Pathology . | Type of bone defects . | Flap combination . |
|---|---|---|---|---|---|---|---|
| 1 | Female | 15 | T2N0M0G2 | Mandible | Osteosarcoma | LC | FFF + ALT |
| 2 | Female | 16 | T2N0M0G2 | Mandible | Osteosarcoma | L | FFF + RFFF |
| 3 | Female | 18 | T2N0M0G3 | Mandible | Osteosarcoma | HC | FFF + ALT |
| 4 | Female | 45 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | HC | FFF + ALT |
| 5 | Female | 47 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
| 6 | Male | 48 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 7 | Male | 55 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + RFFF |
| 8 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 9 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 10 | Male | 60 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
FFF, free fibula flap; RFFF, radial forearm free flap; ALT, anterolateral thigh flap, type C central defect, type L lateral defect, type H lateral defect including the condyle
| Case number . | Sex . | Age . | Staging . | Site . | Pathology . | Type of bone defects . | Flap combination . |
|---|---|---|---|---|---|---|---|
| 1 | Female | 15 | T2N0M0G2 | Mandible | Osteosarcoma | LC | FFF + ALT |
| 2 | Female | 16 | T2N0M0G2 | Mandible | Osteosarcoma | L | FFF + RFFF |
| 3 | Female | 18 | T2N0M0G3 | Mandible | Osteosarcoma | HC | FFF + ALT |
| 4 | Female | 45 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | HC | FFF + ALT |
| 5 | Female | 47 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
| 6 | Male | 48 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 7 | Male | 55 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + RFFF |
| 8 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 9 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 10 | Male | 60 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
| Case number . | Sex . | Age . | Staging . | Site . | Pathology . | Type of bone defects . | Flap combination . |
|---|---|---|---|---|---|---|---|
| 1 | Female | 15 | T2N0M0G2 | Mandible | Osteosarcoma | LC | FFF + ALT |
| 2 | Female | 16 | T2N0M0G2 | Mandible | Osteosarcoma | L | FFF + RFFF |
| 3 | Female | 18 | T2N0M0G3 | Mandible | Osteosarcoma | HC | FFF + ALT |
| 4 | Female | 45 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | HC | FFF + ALT |
| 5 | Female | 47 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
| 6 | Male | 48 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 7 | Male | 55 | T4N2bM0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + RFFF |
| 8 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 9 | Male | 58 | T4N3M0 | Lower–alveolar ridge | Squamous cell carcinoma | LC | FFF + ALT |
| 10 | Male | 60 | - | Mandible | Osteo-radionecrosis | LC | FFF + ALT |
FFF, free fibula flap; RFFF, radial forearm free flap; ALT, anterolateral thigh flap, type C central defect, type L lateral defect, type H lateral defect including the condyle
The mean bone defect was 7.2 cm ± 2.5 cm (range 5–12 cm). The cutaneous defects were between 6 cm × 4 cm and 10 cm × 9 cm, the oral cavity defects from 6 cm × 4 cm to 10 cm × 12 cm. The recipient arteries for double vascular anastomosis were facial and superior thyroid artery; the drainage veins were external jugular, retromandibular, facial or common facial veins, sometimes with lingual veins. The average time taken for ablative tumor and reconstructive surgery was 613 min (range 545–680 min). The radial forearm flaps were used for a partial tongue defect and a chin skin defect (thinner defects).
The total flap survival rate was 100%. No major and only one minor complication occurred: wound infection in an anterior lateral thigh flap (case no. 10), which was treated by local wound care. Hospital admission times averaged 20 d (range 14–32 d). After discharge from the hospital, patients continued to undergo rehabilitation and follow-up (Table 2). Most of our patients (9/10) can perform all activities of daily living. One patient had an ankle stiffness 17 months after reconstruction. The duration of follow-up ranged from 15 to 33 months, with a median of 22.5 months. Four patients had local recurrence. The median time to recurrence was 8 months (3–17 months).
| Score . | After 1 month . | After 6 months . | |
|---|---|---|---|
| . | . | n (%) . | n (%) . |
| Oral diet | 2 | 2 (20%) | 8 (80%) |
| 1 | 6 (60%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Speech intelligibility | 2 | 6 (60%) | 8 (80%) |
| 1 | 2 (20%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Mouth opening | 2 | 2 (20%) | 6 (60%) |
| 1 | 8 (80%) | 4 (40%) | |
| 0 | 0 (0%) | 0 (0%) | |
| Cosmetic outcomes | 2 | 0 (0%) | 0 (0%) |
| 1 | 8 (80%) | 10 (100%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Score . | After 1 month . | After 6 months . | |
|---|---|---|---|
| . | . | n (%) . | n (%) . |
| Oral diet | 2 | 2 (20%) | 8 (80%) |
| 1 | 6 (60%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Speech intelligibility | 2 | 6 (60%) | 8 (80%) |
| 1 | 2 (20%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Mouth opening | 2 | 2 (20%) | 6 (60%) |
| 1 | 8 (80%) | 4 (40%) | |
| 0 | 0 (0%) | 0 (0%) | |
| Cosmetic outcomes | 2 | 0 (0%) | 0 (0%) |
| 1 | 8 (80%) | 10 (100%) | |
| 0 | 2 (20%) | 0 (0%) | |
Notes: Oral diet 2—normal, 1—moderately impaired, restricted diet, 0—severely impaired or impossible and requiring maintenance of an enteral feeding tube; Speech intelligibility 2—normal, easily intelligible, 1—moderately altered, intelligible with effort, 0—severely altered or impossible and patient unintelligible for the listener; Mouth opening 2—normal, greater than 2 finger breadths, 1—moderately limited, between 1 and 2 finger breadths, 0—severely limited, less than 1 finger breadth; Cosmetic outcomes 2—good, 1—acceptable: moderate deformations, depressions or misalignment, 0—poor: severe disfigurement, major deformations, depressions or misalignment that immediately attracts attention.
| Score . | After 1 month . | After 6 months . | |
|---|---|---|---|
| . | . | n (%) . | n (%) . |
| Oral diet | 2 | 2 (20%) | 8 (80%) |
| 1 | 6 (60%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Speech intelligibility | 2 | 6 (60%) | 8 (80%) |
| 1 | 2 (20%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Mouth opening | 2 | 2 (20%) | 6 (60%) |
| 1 | 8 (80%) | 4 (40%) | |
| 0 | 0 (0%) | 0 (0%) | |
| Cosmetic outcomes | 2 | 0 (0%) | 0 (0%) |
| 1 | 8 (80%) | 10 (100%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Score . | After 1 month . | After 6 months . | |
|---|---|---|---|
| . | . | n (%) . | n (%) . |
| Oral diet | 2 | 2 (20%) | 8 (80%) |
| 1 | 6 (60%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Speech intelligibility | 2 | 6 (60%) | 8 (80%) |
| 1 | 2 (20%) | 2 (20%) | |
| 0 | 2 (20%) | 0 (0%) | |
| Mouth opening | 2 | 2 (20%) | 6 (60%) |
| 1 | 8 (80%) | 4 (40%) | |
| 0 | 0 (0%) | 0 (0%) | |
| Cosmetic outcomes | 2 | 0 (0%) | 0 (0%) |
| 1 | 8 (80%) | 10 (100%) | |
| 0 | 2 (20%) | 0 (0%) | |
Notes: Oral diet 2—normal, 1—moderately impaired, restricted diet, 0—severely impaired or impossible and requiring maintenance of an enteral feeding tube; Speech intelligibility 2—normal, easily intelligible, 1—moderately altered, intelligible with effort, 0—severely altered or impossible and patient unintelligible for the listener; Mouth opening 2—normal, greater than 2 finger breadths, 1—moderately limited, between 1 and 2 finger breadths, 0—severely limited, less than 1 finger breadth; Cosmetic outcomes 2—good, 1—acceptable: moderate deformations, depressions or misalignment, 0—poor: severe disfigurement, major deformations, depressions or misalignment that immediately attracts attention.
DISCUSSION
In the head and neck, when the ablation involves complex anatomical boundaries, it may be challenging to reconstruct the defect with single flap. A single chimeric flap, such as chimeric free fibula flap (FFF) or scapular mega flap, has been used for the oromandibular composite defects. The skin islands of FFF were just suitable for the small soft tissue defects [10]. The combined scapular and parascapular flap provided large soft tissue component [11]. But the scapular flap is usually considered secondary choices compared to the FFF or deep circumflex iliac artery free flaps because a two-team approach for oromandibular tumor resection and reconstruction is infeasible [12]. As a result, the operative durations were longer than ours [13].
Large tumors requiring double free flaps figure in a number of reports on reconstructions of complex defects [5, 14, 15]. A second free flap is preferred by some reconstructive surgeons, who assume that this allows better rehabilitation of three-dimensional defects [7, 8, 16]. It is apparent that the use of double free flaps simultaneously constitutes technical difficulties, increasing both operating times and patient morbidity. However, done with a pair of surgical teams, the benefits in aesthetic and functional outcomes outweigh the risks. Furthermore, healing time can be shortened, leading to earlier or timely reception of postoperative adjuvant therapy. Single-stage reconstruction is also beneficial for the cancer patient who may be receiving postoperative treatment [17–19].
For reconstructing head and neck defects, no unified clinical practice guideline for the use of double free flaps exists. However, the following indications may warrant the consideration of a double free flap reconstruction: (i) huge complex defects involving oral mucosa, soft tissue, bone, and external skin that cannot be abundantly provided with one composite flap; (ii) large external coverage and oral lining defects that cannot adequately be resurfaced with one cutaneous or myocutaneous flap; or (3) difficulty insetting a single free flap because of huge and tri-dimensional nature of the defect [1, 20]. It has been postulated (see Wei et al. [19]) that double free flaps should be limited to patients with primary cancers, not recommended for those with recurrent tumors or second primaries [1]. In contrast, it is possible to broaden the use of double free flaps, although Mo et al. do not recommend to use double free flap for patients with a short life expectancy (<6 months).
The use of two free flaps simultaneously has become our choice for reconstructing huge composite defects. Compared with a single free flap, the duration of surgery, complications and hospital stays were acceptable [20–22]. In fact, there were no significant differences in the duration of operation and complication rate in Guillemaud’s single-flap study [20]. Our two-team approach included five head and neck surgeons, so we could prepare enough recipient vessels even with radiated patients. At least, four of surgeons could raise the flaps and perform vascular anastomosis. This meant that when the first team was insetting the FFF and anastomosing the vessels, the second team was harvesting the RFFF or the ALT. Finally, the second pedicle anastomosis was performed. Each surgeon only anastomosed one or two vessels according to the difficulty levels of the procedures, so surgeons could sustain the focus and shorten the operative time; the mean was 613 min compared to 740–780 min in other studies [20, 23].
Good functional results are often reported [2, 17, 19, 20, 24, 25]. For example, the group of 39 older patients in Hanasono et al. received double free flaps for oral defects. Of these, 29 patients were feeding tube dependent prior to surgery, yet 23 resumed an oral diet following surgery [22]. The functional outcome of our patients was excellent. All patients survived and were able to resume an oral diet. Their speech was also easily comprehensible, although this could be due the moderate involvement of the tongue in these cases.
The aesthetic results were accepted, as the flaps showed insignificant contraction post-radiotherapy. However, the color and texture mismatch of the soft tissue reconstruction with either ALT or RFFF are well documented. Therefore, the highest cosmetic score is not achievable in our case series.
CONCLUSION
A two-teams-reconstructive approach may shorten the operative time and reduce the rate of major complications. Simultaneous use of double free flap and careful planning aided the reconstruction in large complex oromandibular defects. In properly selected patients, double free-flap procedures may be favored, providing appropriate tissue characteristics for defect reconstruction.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DECLARATIONS
This research was approved by the Ethics Committee On Biomedical Research (No 5994/BVUB-HĐĐĐ 12th December 2021).
Complete written informed consent was obtained from the patient for the publication of this study and accompanying images.
I, the undersigned, give my consent for the publication of identifiable details, which can include photographs and details within the text to be published in JSCR.
Dr. Nguyen has nothing to disclose.
No funding was received for this article.
This material is the author’s own original work, which has not been previously published elsewhere.
DATA AVAILABILITY
The datasets supporting the conclusions of this article are included within the article.



