-
PDF
- Split View
-
Views
-
Cite
Cite
Meshack Mushobozi Brighton, Victor Meza Kyaruzi, Charles Nhungo, Hassan Mwakimako, Mohamed Salim, Ramadhani Khamisi, Ally Mwanga, Successful open surgery repair of isolated right diaphragmatic rupture in 1-year-old patient at Muhimbili National Hospital: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad255, https://doi.org/10.1093/jscr/rjad255
Close - Share Icon Share
Abstract
Diaphragmatic ruptures rarely occur in isolation, a pathology in paediatric that is difficult to diagnose and can lead to serious complications if left untreated. We present a rare case of isolated right diaphragmatic rupture with liver herniation that was successfully repaired, along with a literature review. A 1-year-old female child was admitted at Emergency Department after being involved in a motor traffic crash as a passenger. Based on clinical presentation and radiological findings, we diagnosed a diaphragmatic rapture, laparotomy was performed in which we found a right isolated diaphragmatic rupture, which was repaired primarily. After re-evaluations, the patient was discharged day 16 postoperative. It is essentially important to evaluate the level of organ damage thoroughly for making a timely informed decision in management paediatric chest trauma.
INTRODUCTION
Diaphragmatic rupture is one of the uncommon surgical conditions in paediatrics that is challenging to diagnose and can have detrimental complications if not well addressed. The majority of paediatric who sustained diaphragmatic traumas exhibit dyspnoea, abdominal pain, sometimes simply no symptoms. To appropriately diagnose and treat this diaphragmatic rupture, clinicians must have a high index of suspicion [1].
Traumatic diaphragmatic rupture frequently occurs in conjunction with other, potentially fatal injuries, necessitating rapid medical attention.
Herein we present the case of a 1-year-old female child who had sustained isolated right diaphragm rupture after blunt thoracic trauma following a motor traffic crash as a passenger that was diagnosed 5 days after the injury while in the ward for treatment.
CASE REPORT
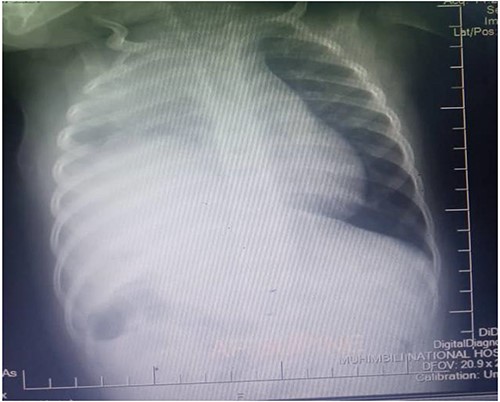
A one-year-old female child was admitted in Emergency Department after being involved in a motor traffic crash as a passenger where she sustained injury to the right leg and blunt head-thoracic-abdominal trauma. After resuscitation and supportive therapy, she underwent plain chest x-ray, which showed reduced right lung volume with elevated right hemidiaphragm and right upper zone opacity. The cardiac silhouette was obliterated in the right.
Thus, the tube thoracostomy with under water seal drainage was performed and supportive oxygen therapy was initiated accordingly. In the second day postadmission, the respiratory symptoms resolved and she was weaned off oxygen and other supportive therapies were reduced. Later a whole-body CT scan was performed and admitted in Paediatric Surgery ward in Muhimbili National Hospital. The CT scan revealed a hypodense fluid collection on the right hemithorax, 33HU associated with ipsilateral pulmonary atelectatic changes, discontinuity of the right hemidiaphragm with intrathoracic herniation of the liver that appeared to be normal in size. Nevertheless, the child was in good condition, without respiratory distress or bowel obstruction.
Laboratory examination revealed haemoglobin of 9.574 g/dl, white blood cells 7.115/L, platelet count 333.0 G/L, urea 2.7 mmol/L, creatinine 37.7 μmol/L, glucose 7.12 mmol/L, K 4.9 mmol/L and CRP 91.5.
Figure 1 shows the plain chest radiography demonstrating the right lung atelectasis with elevated right hemidiaphragm and obliterated cardiac silhouette taken before laparotomy.
Figures 2 and 3 axial views of thoraco-abdominal CT image taken before laparotomy revealing a ruptured diaphragm of a 1-year-old post trauma patient with reduced right lung volume of expansion.
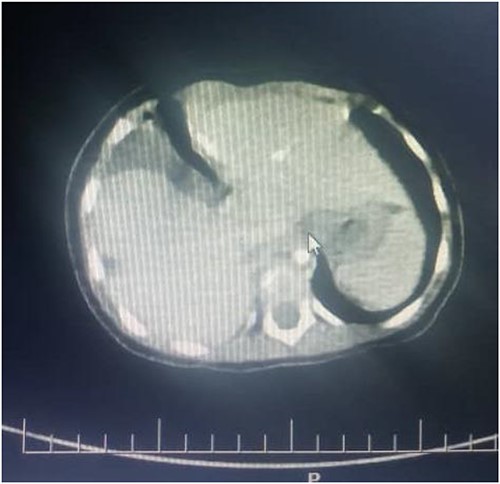
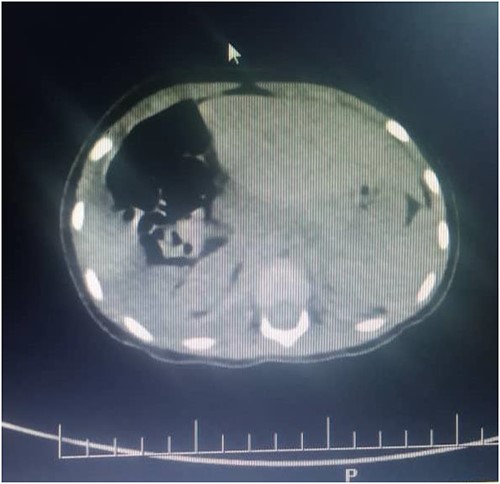
Figure 4 shows a control plain chest radiography taken after the right hemidiaphragmatic repair, it describing adequate right lung volume of expansion, with normal hemidiaphragmatic dome and obvious cardiac silhouette.

Surgical technique
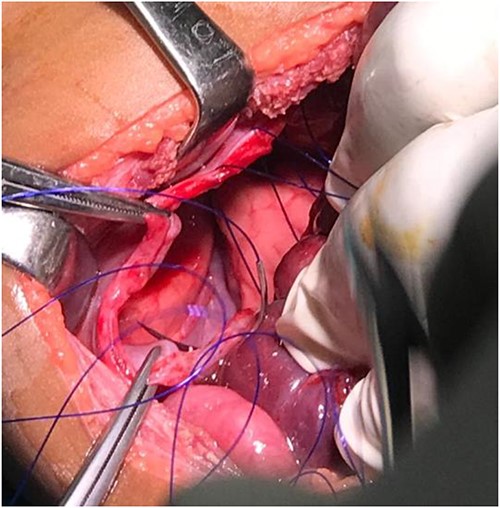
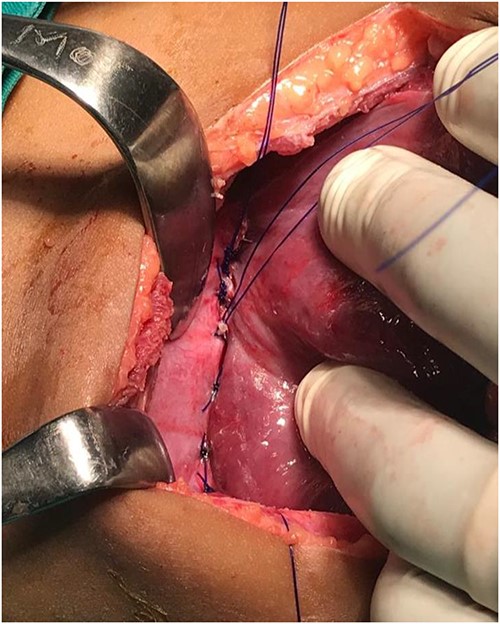
We performed exploratory laparotomy with Kocher incision 2 cm below the right costal margin abdomen opened by layers. The right lobe of the liver, transverse colon as well as part of small bowel were found herniating to the right hemithorax through a wide diaphragmatic defect around 10 cm in the greatest dimension, the liver was not injured but subcapsular haematoma of the right kidney. Thus, the hernia was reduced by gentle traction back of the right lobe of the liver and bowels to peritoneal cavity, exposing the right lung on the background. Furthermore, we visualized the right hemithorax through the bigger defect and found no signs of lung or large vessels injury or haemorrhage. 20Fr chest drainage in the right hemithorax was inserted to evacuate the pneumothorax and fluid collections. Thus, we repaired the defects with non-absorbable polypropylene suture (Prolene 2-0) in an interrupted fashion. No prosthetic mesh was used to cover the defects since the diaphragm did not show any sign of weakness. In the end, we achieved haemostasis. Later the patient was admitted to Paediatric ICU for close monitoring, intensive treatment and support. The post-operative rounds were regular and in day 7 postoperative, she was transferred back to paediatric surgery ward. After re-evaluations and lab values normalization, the patient was discharged day 16 postoperative (Figs 5-7).
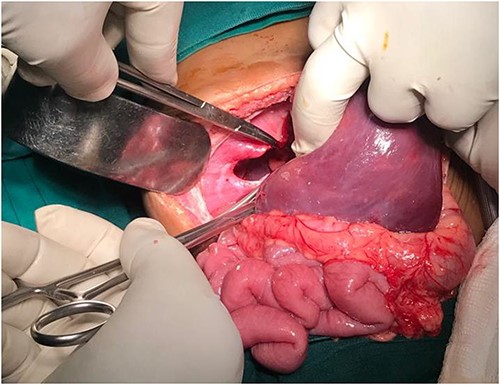
Diaphragmatic defect well appreciable after abdominal viscera retraction.
Showing the non-absorbable polypropylene suture (Prolene 2-0) in simple interrupted pattern
DISCUSSION
One of the leading causes of polytrauma worldwide, motor vehicle accidents are also a major public health concern in Tanzania, where the mortality rate from traffic-related injuries is almost twice as high as the global average [2]. Penetrating abdominal trauma, such as those caused by gunshot and stab wounds, is the main cause of diaphragmatic rupture, but it can also happen as a result of blunt abdominal trauma. However, the diagnosis might be challenging since the physical examination may be unremarkable and initial radiologic imaging may fail to detected 30–50% of diaphragmatic ruptures [3].
Currently, chest injuries account for 25% of trauma-related deaths worldwide and account for close to 10% of all trauma hospital admissions [4]. The most frequent thoracic trauma injuries, however, are pneumothorax and hemothorax, which are permanently treated in 80% of cases with tube thoracostomy. To remove an accompanying hemothorax or pneumothorax, a chest tube is inserted, taking care to prevent further harm. Since diaphragm injuries do not heal on their own, practically all patients require surgical repair [5].
The majority of right-sided injuries as well as all left-sided diaphragmatic injuries need to be repaired. The patient must be aware of the possibility of a delayed rupture in the uncommon case of a minor, right-sided tear that qualifies for expectant care. Transabdominal approaches are frequently used for surgical care, frequently after laparotomies performed for other ailments. A less invasive laparoscopic or even thoracoscopic method may be useful in patients with less severe injuries [6].
Once the herniated contents have been reduced to their normal anatomical position, the rupture in the diaphragm can be repaired using interrupted non-absorbable sutures, making the repair typically straightforward. It is recommended to leave a chest tube in place for a few days.
Laparotomy or thoracotomy incisions have been used for many years to repair diaphragmatic rupture. Open surgical treatments, however, are linked to more postoperative pain, a longer hospital stay, and the emergence of long-term issues such an incisional hernia [7, 8]. In contrast, the advantages of laparoscopy include a quicker recovery time, a lower risk of wound complications, and less postoperative pain (and hence less need for analgesics) [3]. A laparoscopy can detect various lesions in the abdominal cavity in addition to clearly illuminating both hemidiaphragms to check for diaphragmatic rupture. Furthermore, in the hands of a skilled surgeon, simultaneous laparoscopic repair of the rupture site is possible.
Despite these benefits, the success of laparoscopic repair of diaphragmatic rupture following blunt abdominal trauma is still up for debate. Most people can agree that the importance of the surgeon’s skill and careful patient selection [9, 10].
CONCLUSION
To appropriately coordinate the surgeons, it is crucial to assess the extent of organ damage. For each patient, the scheduling of the procedure and available treatments should be determined. Aggressiveness in diagnosing a condition that is amenable to surgery is very crucial for early treatment in emergency basis. The only definitive management of a diagnosed diaphragmatic rupture is surgery and it involves surgeons, radiologists, emergency physicians and nurses to be involved in management of the patient. Communication between the team members is vital for the better outcome of the patient. If a chest tube has been left in after surgery, it should be monitored for air and fluid leaks.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no any competing interest in writing and publishing the paper.
FUNDING
None.
AUTHORS' CONTRIBUTIONS
Dr. Meshack Brighton, Dr. Victor Meza Kyaruzi, study concept, literature review, writing the paper and an assistant surgeon; Dr. Charles Nhungo and Dr. Hassan Mwakimako data collection; Dr. Ally Mwanga Supervisor; and Dr. Ramadhani H.K Supervisor.
CONSENT
The surgeon informed the parent on this serious condition, which required urgent surgery. She understood and approved a surgery. She accepted the risks associated with the procedure, including morbidity and mortality. The informed consent was confirmed by signing it.
INFORMED CONSENT
Written informed consent was obtained from the parent for publication of this case report and any accompanying images.



