-
PDF
- Split View
-
Views
-
Cite
Cite
Erica Hian Kim Ngiam, Denise Fok, Nadia Sim, Allen Wong, Jiajun Feng, Tan Pearlie, Hui Wen Chua, Grace Chan, Yee Onn Kok, A case of cutaneous psoriasis vulgaris achieving complete remission post major breast reconstructive surgery, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad148, https://doi.org/10.1093/jscr/rjad148
Close - Share Icon Share
Abstract
Psoriasis is a debilitating chronic inflammatory systemic condition largely affecting the skin. Major surgery is relatively contraindicated due to the propensity for triggering psoriatic flares and koebnerization of the surgical scars. We detail an interesting case of complete psoriasis remission following a right nipple-sparing mastectomy with sentinel lymph node biopsy with vascular augmented pedicled transverse rectus abdominal myocutaneous (TRAM) flap in a patient with systemic psoriasis vulgaris and arthropathy. Intra-operatively, majority of the psoriatic plaques were excised or de-epithelized and used as part of the ipsilateral TRAM flap. Post-operatively, koebnerization did not occur and her psoriasis was cured completely even after cancer chemotherapy. One of several hypotheses include excision with de-epithelization of most of the psoriatic plaques reduces disease and inflammatory burden leading to complete remission. Perhaps, surgery could one day play a supporting role to existing treatment options to achieve psoriasis remission.
INTRODUCTION
Psoriasis is a debilitating chronic inflammatory systemic condition largely affecting the skin. Although this condition is largely driven by T lymphocytes, the complex interactions involve innate and adaptive immune cells and resident skin cells. Known environmental triggers and associations include trauma and major surgery is relatively contraindicated due to the propensity for triggering psoriatic flares and koebnerization of the surgical scars [1].
To the best of our knowledge, there have been no reports of psoriasis remission achieved immediately after major surgeries. There are only limited case reports of targeted surgical excision and use of dermabrasion which successfully removed psoriatic plaques with minimal recurrence [2–4]. However, these methods are not widely accepted in current clinical practice due to existing established medical therapies in achieving systemic control of disease and the lack of data supporting the efficacy of surgical treatment of psoriasis.
CASE REPORT
We detail complete psoriasis remission in a 67-year-old Chinese female diagnosed with chronic systemic psoriasis vulgaris and arthropathy on long standing oral steroids and ciclosporin. She underwent right nipple-sparing mastectomy with sentinel lymph node biopsy for T2N0M0 right breast cancer and breast reconstruction with vascular augmented pedicled transverse rectus abdominal myocutaneous (TRAM) flap. Contrary to conventional belief, koebnerization did not occur and her psoriasis was cured completely in the 6 weeks and 2 months follow-up, even after cancer chemotherapy commenced.
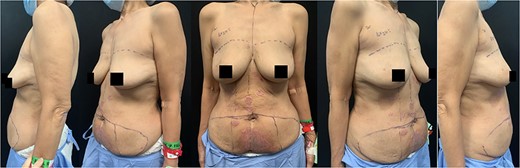
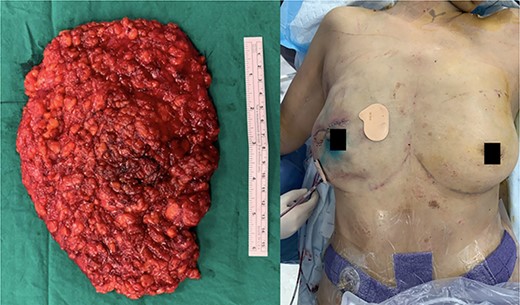
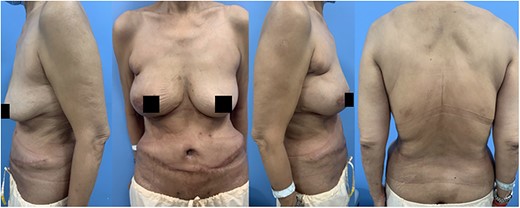
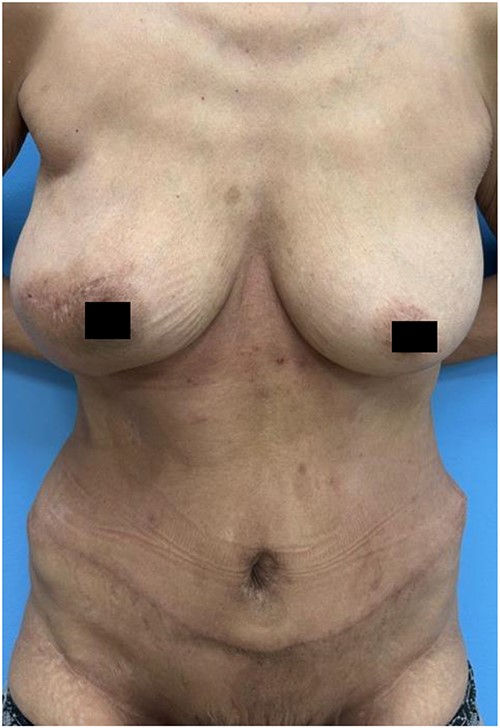
Pre-operatively, her steroids and ciclosporin had been discontinued for 10 days in concert with her rheumatologist and breast surgeon, as per multidisciplinary care. She had multiple erythematous psoriatic plaques centered mostly on the breasts and abdomen (Fig. 1). Intra-operatively, majority of the psoriatic plaques were excised or de-epithelized and used as part of the ipsilateral TRAM flap (Fig. 2). On post-op day 5, the patient underwent right breast monitoring skin paddle excision. During the inpatient recovery, the remnant psoriatic plaques had gradually disappeared or converted to hyperpigmented non-erythematous, non-scaly lesions (Figs 3 and 4). These changes were maintained even in the 1 year post operative follow-up (Fig 5). Her joints remained quiescent. Inflammatory markers (C-Reactive Protein), a marker used to assess disease remission, down-trended and became flat post-op day 27 (Table 1).

| . | Three months pre-operatively . | Post-op day 15 . | Post-op day 27 . | Two months follow-up . |
|---|---|---|---|---|
| C-reactive protein (mg/L) | 1.0 | 10.1 | 1.2 | 1.2 |
| . | Three months pre-operatively . | Post-op day 15 . | Post-op day 27 . | Two months follow-up . |
|---|---|---|---|---|
| C-reactive protein (mg/L) | 1.0 | 10.1 | 1.2 | 1.2 |
| . | Three months pre-operatively . | Post-op day 15 . | Post-op day 27 . | Two months follow-up . |
|---|---|---|---|---|
| C-reactive protein (mg/L) | 1.0 | 10.1 | 1.2 | 1.2 |
| . | Three months pre-operatively . | Post-op day 15 . | Post-op day 27 . | Two months follow-up . |
|---|---|---|---|---|
| C-reactive protein (mg/L) | 1.0 | 10.1 | 1.2 | 1.2 |
DISCUSSION
This unexpected phenomenon sheds new light on what is commonly known to be an exacerbating factor for psoriasis flares. Perhaps one can look into immunological responses to surgery and correlate that to the pathogenesis in psoriasis. Existing literature reviews have suggested the role of regulatory B cells and its secretion of anti-inflammatory cytokine interleukin (IL)-10 in reducing disease symptoms [5]. Incidentally, IL-10 is also thought to be a major role player in the counter-inflammatory response to surgery; this relation could potentially explain this phenomenon [6]. Existing hypothesis of higher incidence of CD4+ and CD8+ T-cell apoptosis post-operatively in current literature serves as an alternative explanation [6, 7]. However, these immunological responses could likely only account for the phenomenon witnessed in this case report in the short time frame following surgery as these immune-mediated fluctuations would have returned to patient’s baseline levels over the days following surgery. It could then be that the excision and de-epithelization of the majority of psoriatic plaques intra-operatively reduced the disease and inflammatory burden, contributing to complete remission for the longer term.
CONCLUSION
Further study into correlating the systemic responses mounted after a major reconstruction and the pathophysiology of psoriasis could potentially lead to novel therapeutic strategies and reshape the plastic surgeon’s approach when operating on a patient with psoriasis. Perhaps, surgical techniques like de-epithelization or excision of entire psoriatic plaques could one day play a supporting role to existing treatment options to achieve psoriasis remission especially in patients who are resistant to medical therapy. Given the risk of triggering further psoriatic flares when surgery is performed for these patients, it might be pertinent to engineer a screening process such as bedside dermabrasion over a small skin surface covered with psoriatic plaque followed by a period of response monitoring to filter out patients who might develop an adverse outcome from surgery.
AUTHORS’ CONTRIBUTIONS
First author: Obtaining case details, literature reviews and writing the report. Rest of co-authors: Clinical and discussion input.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
Footnotes
†This case report had been presented as a poster presentation during Plastic and Aesthetic Surgery Meeting 2022, Singapore.
References
- joint disorders
- chemotherapy regimen
- psoriasis
- reconstructive surgical procedures
- sentinel lymph node biopsy
- surgical procedures, operative
- abdomen
- breast
- skin
- myocutaneous flap
- psoriasis vulgaris
- breast reconstruction with tram flap
- scar, surgical
- excision
- complete remission
- tram flap
- nipple-sparing mastectomy
- disease remission



