-
PDF
- Split View
-
Views
-
Cite
Cite
Jason Kreinces, Alicia I Robbins, Daniel E Kim, Cecal bascule in pregnancy: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad287, https://doi.org/10.1093/jscr/rjad287
Close - Share Icon Share
Abstract
A 36-year-old female at 36 weeks’ gestation presented with right upper quadrant abdominal pain. She had no prior surgeries. Her pregnancy had been uncomplicated up until her presentation. Abdominal ultrasound was negative for cholecystitis or cholelithiasis, and the appendix was not visualized. During the second day of her hospital course, an abdominal magnetic resonance imaging (MRI) was performed revealing dilated small intestine with air-fluid levels and an inverted-appearing, prominent cecum. She was urgently taken to the operating room for cesarean section followed by abdominal exploration. After delivery of the child, a cecal bascule was found, with a severely distended cecum. To our knowledge, this is the first report of a cecal bascule diagnosed by MRI, and the first diagnosis of cecal bascule in a pregnant patient requiring surgical intervention. We discuss the pathophysiology, diagnosis and treatment of cecal bascule and review the current literature of reported cases.
INTRODUCTION
Cecal bascule is the acute folding of the cecum in an anterior and cephalad direction onto the ascending colon [1, 2]. A closed loop obstruction is created between the ileocecal valve and the point of inflection at the ascending colon [3]. Distension of the cecum leads to capillary and venous obstruction followed by necrosis and perforation. The incidence of cecal bascule is estimated at 0.1% of all intestinal obstructions [4, 5]. We report a case of a 36-year-old woman who presented at 36 weeks’ gestation who was diagnosed with a cecal bascule requiring emergent resection. The incidence and appropriate treatment of cecal bascule during pregnancy is unknown. Therefore, we reviewed the literature for the management of cecal bascule associated with pregnancy. We also compared the pathophysiology, diagnosis and treatment of cecal bascule with that of cecal volvulus.
CASE REPORT
A 36-year-old female at 36 weeks’ gestation presented to the emergency department with right upper quadrant abdominal pain. She had no past medical nor surgical history. She had two prior pregnancies with uncomplicated vaginal deliveries. She reported colicky right upper quadrant abdominal pain that began on the evening prior to admission. The pain radiated to her back but was not associated with food intake. She had an episode of nausea with vomiting. She denied fever, chills, headache, dysuria, nor change in bowel movements. Her pregnancy had been uncomplicated up until her presentation.
Her vital signs on admission were temperature 36.6°C, heart rate of 52, blood pressure 125/76 mmHg and respiratory rate of 16. Laboratory tests were abnormal for a white blood cell count of 11.1 × 1000/μL and alkaline phosphatase of 172 U/L. On physical examination, her gravid uterus was appropriately at the level of her epigastric region. There was moderate tenderness at the right middle and right upper quadrants without peritoneal signs. An abdominal ultrasound (US) was negative for cholecystitis or cholelithiasis, and the appendix was not visualized.
On hospital day 2, the patient became obstipated, and her abdominal exam had notable distension with persistent right upper quadrant tenderness. An abdominal magnetic resonance imaging (MRI) was performed revealing dilated small intestine with air-fluid levels and an inverted-appearing, prominent cecum (Figs. 1 and 2). The patient was diagnosed with an acute abdomen from probable cecal volvulus versus appendicitis and was urgently taken to the operating room for cesarean section (c-section) to facilitate abdominal exploration. After delivery of the child, a cecal bascule was found, with a severely distended cecum (Fig. 3). Because the cecum and ascending colon were deserosalized, a right hemicolectomy with primary ileocolic anastomosis was performed. The patient had return of bowel function on post operative day 5 and was discharged home on day 7.
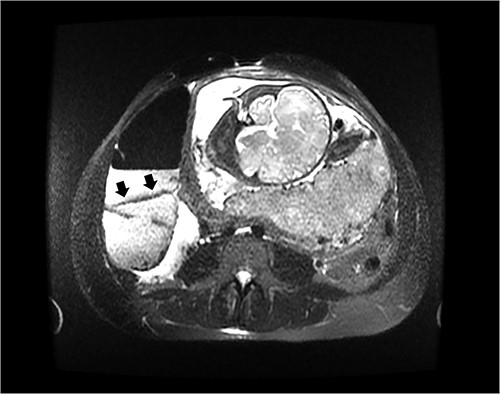
Axial image of an abdominal MRI on a 36-week pregnant patient with a dilated cecum anteriorly displaced to the ascending colon. Arrows mark the point of inflection.
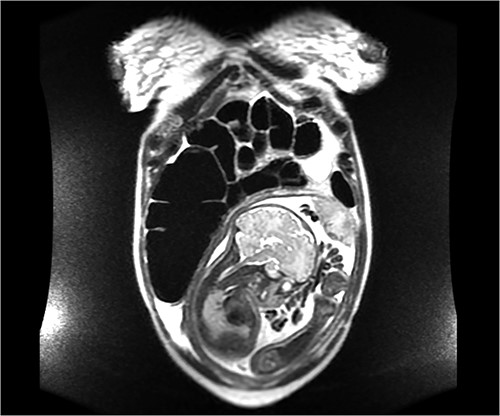
Coronal image of the same MRI showing a dilated cecum displaced superiorly, consistent with a cecal bascule.
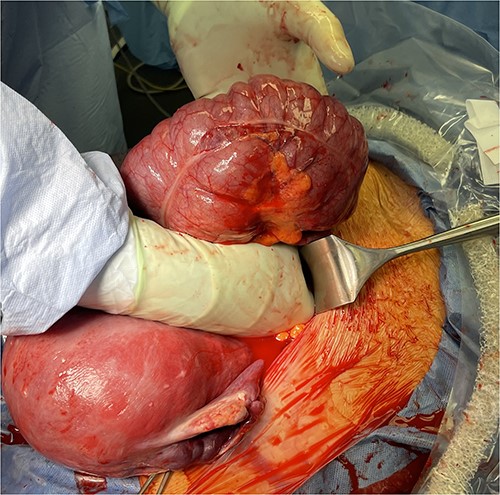
Dilated and deserosalized cecum after reduction of the cecal bascule. The uterus immediately after cesarean section lies to the lower left.
METHODS
Literature review was performed in search of reported cases of pregnant patients with cecal bascule. Three online databases, Web of Science, CINAHL and Ovid, were queried on 22 February 2023 for the keywords: pregnancy, cecum and bascule or volvulus. Volvulus was included since cecal bascule is often grouped under cecal volvulus. The queries included all publication years and all languages. Additional references pertaining to cecal bascule in pregnant patients were identified from the index articles and examined. Google translate was used for articles in other languages.
RESULTS
The initial literature search produced 82 citations. Abstracts were reviewed and the list narrowed to 50 relevant articles. Full texts were examined to confirm cases of cecal bascule and rule out cases of volvulus. In total, 48 studies were eliminated for the reasons listed in Figure 4. References cited in the full texts were screened and two additional cases of cecal bascule were included for a total of four cases pertinent to our study.
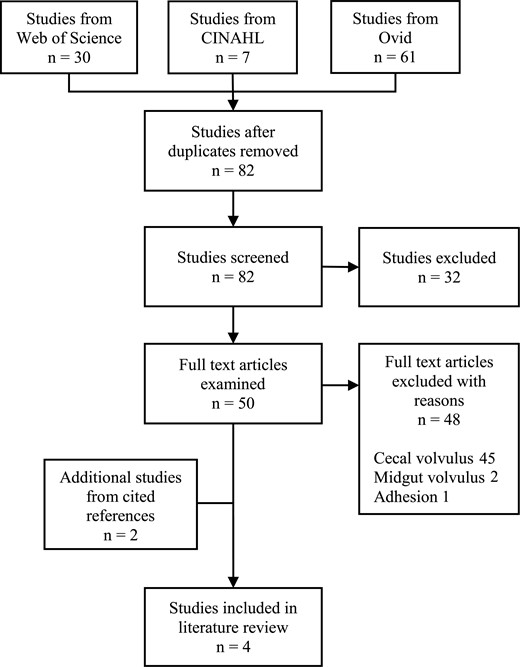
Flow diagram in search for cecal bascule cases associated with pregnancy.
The four cases of cecal bascule associated with pregnancy are displayed in Table 1. Three of the cases involved the development of cecal bascule after c-section. The first patient had four prior pregnancies with three prior c-sections; she developed a cecal bascule 12 h after her fourth c-section [6]. The second patient had four prior pregnancies with one prior c-section; she developed a cecal bascule 3 days after her second c-section [7]. The third patient had two prior pregnancies, no previous surgeries and developed a cecal bascule 5 days after c-section [8]. Only one case reported cecal bascule diagnosed during pregnancy [9]. However, this case was part of a retrospective study of computed tomography (CT) scans performed on pregnant patients with abdominal pain and the demographics specific to the patient was not reported. Furthermore, the patient did not undergo surgical intervention.
Case reports of patients diagnosed with cecal bascule associated with pregnancy.
| Publish year . | Author . | Age . | Gestation age . | Prior pregnancies . | Prior surgeries . | Radiologic findings . | Intraoperative finding . | Surgery performed . |
|---|---|---|---|---|---|---|---|---|
| 2021 | Bakshi [6] | 37 | 12 h post c-section | 4 | Three c-sections | Abdominal X-ray: Obstruction or ileus. CT: Dilated and superior displacement of cecum. | Dilated, edematous cecal bascule with a localized area of necrosis. | Right hemicolectomy |
| 2010 | Salih [7] | 40 | 3 days post c-section | 4 | c-section | Abdominal X-ray and CT: Distended cecum. | Cecal bascule with necrosis and serosal tears. | Right hemicolectomy |
| 2010 | Thangasamy [8] | 42 | 5 days post c-section | 2 | None | CT: Cecum lying horizontally with cecal pole extending leftward. | Dilated cecum with small perforation. | Right hemicolectomy |
| 2007 | Lazarus [9] | 25.9* | 23 weeks* | Unreported | Unreported | US: Normal. CT: Cecal bascule. | No surgical intervention | No surgical intervention |
| Publish year . | Author . | Age . | Gestation age . | Prior pregnancies . | Prior surgeries . | Radiologic findings . | Intraoperative finding . | Surgery performed . |
|---|---|---|---|---|---|---|---|---|
| 2021 | Bakshi [6] | 37 | 12 h post c-section | 4 | Three c-sections | Abdominal X-ray: Obstruction or ileus. CT: Dilated and superior displacement of cecum. | Dilated, edematous cecal bascule with a localized area of necrosis. | Right hemicolectomy |
| 2010 | Salih [7] | 40 | 3 days post c-section | 4 | c-section | Abdominal X-ray and CT: Distended cecum. | Cecal bascule with necrosis and serosal tears. | Right hemicolectomy |
| 2010 | Thangasamy [8] | 42 | 5 days post c-section | 2 | None | CT: Cecum lying horizontally with cecal pole extending leftward. | Dilated cecum with small perforation. | Right hemicolectomy |
| 2007 | Lazarus [9] | 25.9* | 23 weeks* | Unreported | Unreported | US: Normal. CT: Cecal bascule. | No surgical intervention | No surgical intervention |
*Mean values of a retrospective cohort of pregnant patients that received CT scans for abdominal pain.
Case reports of patients diagnosed with cecal bascule associated with pregnancy.
| Publish year . | Author . | Age . | Gestation age . | Prior pregnancies . | Prior surgeries . | Radiologic findings . | Intraoperative finding . | Surgery performed . |
|---|---|---|---|---|---|---|---|---|
| 2021 | Bakshi [6] | 37 | 12 h post c-section | 4 | Three c-sections | Abdominal X-ray: Obstruction or ileus. CT: Dilated and superior displacement of cecum. | Dilated, edematous cecal bascule with a localized area of necrosis. | Right hemicolectomy |
| 2010 | Salih [7] | 40 | 3 days post c-section | 4 | c-section | Abdominal X-ray and CT: Distended cecum. | Cecal bascule with necrosis and serosal tears. | Right hemicolectomy |
| 2010 | Thangasamy [8] | 42 | 5 days post c-section | 2 | None | CT: Cecum lying horizontally with cecal pole extending leftward. | Dilated cecum with small perforation. | Right hemicolectomy |
| 2007 | Lazarus [9] | 25.9* | 23 weeks* | Unreported | Unreported | US: Normal. CT: Cecal bascule. | No surgical intervention | No surgical intervention |
| Publish year . | Author . | Age . | Gestation age . | Prior pregnancies . | Prior surgeries . | Radiologic findings . | Intraoperative finding . | Surgery performed . |
|---|---|---|---|---|---|---|---|---|
| 2021 | Bakshi [6] | 37 | 12 h post c-section | 4 | Three c-sections | Abdominal X-ray: Obstruction or ileus. CT: Dilated and superior displacement of cecum. | Dilated, edematous cecal bascule with a localized area of necrosis. | Right hemicolectomy |
| 2010 | Salih [7] | 40 | 3 days post c-section | 4 | c-section | Abdominal X-ray and CT: Distended cecum. | Cecal bascule with necrosis and serosal tears. | Right hemicolectomy |
| 2010 | Thangasamy [8] | 42 | 5 days post c-section | 2 | None | CT: Cecum lying horizontally with cecal pole extending leftward. | Dilated cecum with small perforation. | Right hemicolectomy |
| 2007 | Lazarus [9] | 25.9* | 23 weeks* | Unreported | Unreported | US: Normal. CT: Cecal bascule. | No surgical intervention | No surgical intervention |
*Mean values of a retrospective cohort of pregnant patients that received CT scans for abdominal pain.
DISCUSSION
Cecal bascule is frequently classified as a subtype of cecal volvulus. However, cecal bascule is a distinct entity and inaccurate to be termed a volvulus [4, 10]. A cecal volvulus is an axial twist of the cecum, ascending colon and terminal ileum around the mesenteric pedicle [2, 11]. The cecal volvulus occurs from increased mobility of the cecum caused by a congenital lack of retroperitoneal fixation of the cecum along with a fixed point about which the bowel can rotate, typically the mesentery [12, 13]. On the contrary, the lack of retroperitoneal attachments is not required for a cecal bascule to occur [2]. The torsion of the mesentery for a cecal volvulus causes vascular insufficiency leading to gangrene [14]. In contrast, a cecal bascule does not have an axial twist. Hence, vascular occlusion and ischemic changes are rare [2, 15]. A cecal bascule can still develop gangrene from overdistention causing constriction of the venous and capillary network [3]. Because of these major differences, one study deliberately excluded cecal bascule from their review of cecal volvulus [14].
Cecal volvulus accounts for ⁓1% of all intestinal obstructions [4, 11]. Since the incidence of cecal bascule is 10% of cecal volvulus cases, we calculate that cecal bascule makes up 0.1% of intestinal obstructions [5]. Causes of intestinal obstruction during pregnancy and the puerperium include adhesions (59%), volvulus (23%), idiopathic (8%), intussusception (5%) and hernia (3%) [16]. Cecum is the site of volvulus in 20–25% of cases [16, 17]. Hence, cecal volvulus occurs one in every 1 000 000 pregnancies [18, 19]. The incidence of cecal bascule during pregnancy is unknown.
The rarity of a cecal bascule may be that the cecum flops back into anatomical position causing intermittent subacute obstructions [15]. This is evident in our patient as she had colicky pain in the right side of her abdomen during the first hospital day, before developing obstructive symptoms. This is also evident in the patient from Lazarus’ study since she did not require surgical intervention [9]. The pathogenesis of how pregnancy leads to a cecal bascule is unclear [3, 8]. We believe that in our patient, the enlarging uterus displaced a mobile cecum to such an extent that it could no longer reduce back to its anatomical position. However, just the presence of a gravid uterus does not explain why cecal bascules occurred after delivery in three of the case reports. Bakshi hypothesized that relaxation from anesthesia and the postoperative state in a patient with a mobile cecum predisposed her for a cecal bascule [6]. Thangasamy concluded that the cecal bascule developed as a complication of post cesarean ileus [8]. Salih stated that both the displacement of the cecum by the gravid uterus and the sudden change in intraabdominal pressure after cesarean section were predisposing factors [7].
A cecal bascule is difficult to diagnose because its presentation is similar to routine discomforts of pregnancy. Common symptoms of a cecal bascule and their prevalence are distension (84%), abdominal pain (61%) and vomiting (30%) [3]. Unlike a volvulus, the symptoms of a cecal bascule may occur intermittently [20]. Prompt diagnosis requires a high index of suspicion as delay leads to gangrenous necrosis or colonic perforation which results in maternal and fetal morbidity and mortality [21]. Most patients present with leukocytosis, although no other laboratory findings are consistent for cecal bascule [3].
Another cause for the delay in diagnosis is the clinician’s hesitancy to order diagnostic radiologic imaging in pregnant patients due to the fear of harm to the fetus [22, 23]. The opinion of the American College of Obstetricians and Gynecologists is that the radiation exposure of plain X-ray, CT or nuclear medicine technology is at a dose much lower than the exposure associated with fetal harm and that the maternal benefit from early and accurate diagnosis of acute processes such as appendicitis or bowel obstruction outweighs the theoretical fetal risks [24]. Yet, US and MRI are not associated with fetal risk and should therefore be considered first when available. The utility of US for diagnosing a cecal bascule or other bowel obstruction is poor as evidenced by the normal US in the case reports by Lazarus and ours [9]. However, US is still recommended in the pregnant patient with abdominal pain because of its safety and ability to diagnose obstetric or gynecologic etiologies for pain [9]. A cecal bascule on plain abdominal X-ray is characterized by distension of the cecum, paucity of gas in the distal colon, dilated small bowel and gas shadow within the pelvis [3]. CT scan shows displacement of the cecum to the upper or central abdomen, the ileocecal valve to the right upper quadrant and a transition zone between cecum and ascending colon [3]. The sensitivity of diagnosing a cecal bascule in a nonpregnant patient by CT scan is 61% [3]. Diagnosis of cecal bascule by MRI was not found in literature. The MRI for our patient showed an anterior and superior inversion of the cecum.
No consensus exists on the treatment of a cecal bascule due to its rarity [3, 20]. As such, cecal bascules have been managed in the same manner as volvulus [20, 21]. Nonoperative management of the cecal bascule or volvulus may include nasogastric decompression, colonoscopy and contrast enema. Nasogastric decompression was successful in only one of 26 patients with cecal bascule [3]. Although Nwanguma advises an attempt at reducing the cecal bascule via colonoscopy, the success rate is only 5% [10]. No literature was found on the use of contrast enema for the reduction of a cecal bascule. For cecal volvulus, barium enema reduction is not advised due to risk of perforation and early recurrence [4, 25]. Although nonoperative treatment of a cecal bascule would be preferable in a pregnant patient, it is not recommended because of the maternal and fetal risk from the delay in diagnosis. Bakshi reported localized necrosis of the cecum upon laparotomy at 16 h after cesarean section [6]. Our patient was found with deserosalized cecum and ascending colon at 6 h after the onset of obstipation and abdominal distension. Necrosis of the cecum was found at the time of surgery in 20% of patients with cecal bascule or volvulus [26].
Resection should be the initial and definitive treatment for cecal bascule or volvulus, even if no necrosis is present, since it prevents recurrence with minimal morbidity and mortality [4, 27]. Other surgical options for cecal volvulus if the intestine is found viable are reduction alone, cecopexy and tube cecostomy. Any of these surgical procedures could potentially be accomplished laparoscopically [10, 25]. Surgical reduction alone of a cecal bascule is not advised due to a high recurrence rate exceeding 30% [10, 20]. Cecopexy and cecostomy tube are appealing since they can be performed relatively rapidly and because a cecopexy does not require opening an unprepped bowel [1, 25, 28]. Neither cecopexy nor cecostomy was found to be superior for the treatment of cecal volvulus [25]. We found no report in the literature on the surgical treatment of a pregnant patient with cecal bascule.
CONCLUSIONS
Cecal bascule is a very rare but potentially life-threatening disease during pregnancy. Symptoms include abdominal pain, distension, nausea and vomiting that are similar to that of normal pregnancy. Thus, high index of suspicion is required to pursue further evaluation. Laboratory testing may only be positive for leukocytosis. US followed by MRI are recommended, however, plain abdominal X-ray and CT scans are considered safe for the fetus. Although nonsurgical reduction of a cecal bascule is appealing in the pregnant patient, we recommend urgent surgical exploration due to the likelihood of cecal necrosis or perforation from delay in diagnosis. We recommend colonic resection since the success rate of cecopexy or cecostomy for a pregnant patient with cecal bascule is unknown. To our knowledge, this is the first report of a cecal bascule diagnosed by MRI, and the first diagnosis of cecal bascule in a pregnant patient requiring surgical intervention.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was received to assist with the preparation of this manuscript.
CONSENT STATEMENT
Written informed consent was obtained from the patient for publication of this case report.
DATA AVAILABILITY
Not applicable.
References
Copel J, El-Sayed Y, Heine RP, Wharton KR.



