-
PDF
- Split View
-
Views
-
Cite
Cite
Raeda Taj, Sean Perez, Lily J Jih, Christina Huynh, Jennifer Berumen, Michael Bouvet, Primary extrahepatic biliary neuroendocrine tumor: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad277, https://doi.org/10.1093/jscr/rjad277
Close - Share Icon Share
Abstract
Extrahepatic biliary neuroendocrine tumors (EBNETs) are extremely rare and difficult to diagnose. The vast majority are diagnosed postoperatively on histological evaluation of surgical specimens. Workup and treatment principles are largely based on retrospective series and case reports. Complete surgical resection is the gold standard treatment for these lesions. Here we present a case of a 77-year-old male with a biopsy-proven EBNET incidentally discovered during evaluation for fatty liver disease. Further workup did not show any other suspicious lesions. Resection of the tumor and multiple Roux-en-Y hepaticojejunostomy was performed. Final pathology revealed grade 1, well-differentiated neuroendocrine tumor. This is the third case reported in the literature with a confirmed preoperative EBNET diagnosis based on endoscopic biopsy results. This case highlights the feasibility of preoperative diagnosis of EBNETs and emphasizes the importance of complete surgical resection.
INTRODUCTION
Gastrointestinal neuroendocrine tumors (NETs) are rare neoplasms that arise from Kulchitsky (enterochromaffin) cells. Those cells are found in highest proportion in the small intestine, and rarely within the hepatobiliary tract [1]. Extrahepatic biliary neuroendocrine tumors (EBNETs) are among the rarest primary sites of NETs with a reported incidence of 0.32%, and only 150 cases reported in the literature since its description in 1959 with a 1.7:1 female-to-male ratio [2, 3].
The vast majority are diagnosed postoperatively on histological and immunohistochemical (IHC) evaluation of the specimen. Indeed, many reported cases proceed to surgical intervention with the presumed diagnosis of cholangiocarcinoma, a much more common malignancy of the extrahepatic biliary duct. Surgery is the standard treatment of care and offers prolonged disease-free survival [4, 5]. Here we describe the clinical course, workup and surgical approach of a patient with an incidental finding of EBNET. Interestingly, the diagnosis was made preoperatively.
CASE REPORT
A 77-year-old male with a history of hypertension and hypothyroidism underwent imaging for possible fatty liver disease and was found to have a 3 cm porta hepatis mass causing mild intrahepatic biliary ductal dilation on Magnetic Resonance Elastography (Fig. 1). A multi-phase computed tomography (CT) obtained and showed an isolated 2.8 cm hyperenhancing nodular mass in the liver hilum (Fig. 2). The patient did not have any symptoms, such as jaundice, vomiting, flushing or diarrhea. Physical examination and all biochemical markers were normal, including liver function tests and serum tumor markers (alpha-fetoprotein and carcinoembryonic antigen 19–9). No serologic evidence of hepatitis B or C virus infection was found.
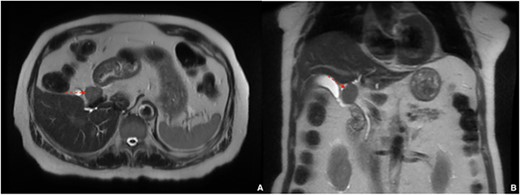
Magnetic resonance elastography showing 3 cm porta hepatis mass causing mild intrahepatic biliary ductal dilation; (A) axial view, (B) coronal view.
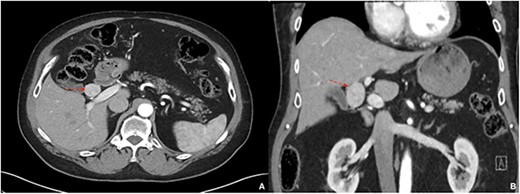
A multi-phase CT showing a 2.8 cm hyperenhancing nodular mass in the liver hilum; (A) axial view, (B) coronal view.
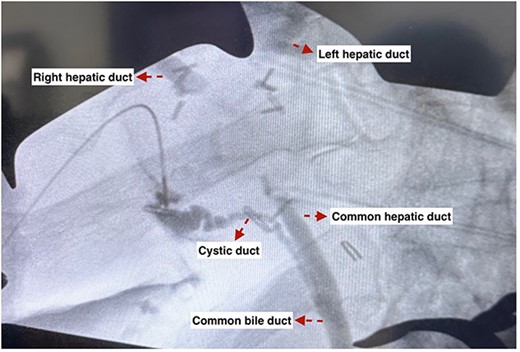
He underwent endoscopic ultrasound (EUS) and fine needle aspiration (FNA) of the mass with an experienced gastroenterologist, with pathology demonstrating round to oval tumor cells with fine stippled chromatin and moderate cytoplasm. IHC demonstrated positivity for chromogranin, synaptophysin, OSCAR and AE1/AE3. The specimen was negative for CDX2 and TTF-1. Ki-67 showed <1% proliferation activity. Overall, consistent with an NET (Fig. 3), a positron emission tomography (PET)/ CT 68Ga-Dotatate scan was performed to evaluate for other possible primary tumors but only demonstrated the previously seen 3 cm porta hepatis mass with extremely intense radiotracer uptake (SUV max 76.7) and no other suspicious lesions. His case was discussed at a multidisciplinary tumor board with the ultimate recommendation being surgical resection.
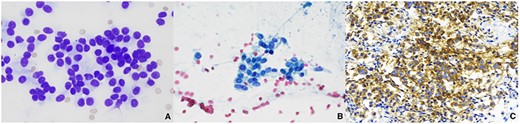
FNA of extrahepatic biliary mass revealed a well-differentiated NET; (A) cluster of monotonous cells in rosettes, Diff-Quick, 600x; (B) uniform round to oval cells with salt and pepper chromatin and moderate amounts of granular cytoplasm, Papanicolaou, 600x; (C) tumor cells were diffusely positive for synaptophysin, 400x.
He underwent tumor resection with the excision of extrahepatic bile ducts via right subcostal incision with cholecystectomy and multiple Roux-en-Y hepaticojejunostomy. The tumor was firm, encasing the common hepatic duct and extending proximally to the right and left hepatic ducts (Fig. 4). An intraoperative cholangiogram was performed and demonstrated tumor involvement of the common hepatic duct up to the right and left hepatic ducts (Fig. 5). The tumor was resected and the patient had three right bile duct openings (anterior, posterior and accessory) (Figs 6 and 7). Therefore, three separate Roux-en-Y hepaticojejunostomy anastomoses were created for the left hepatic duct, right anterior and posterior, and right accessory duct. The patient had an uneventful postoperative course and was discharged on postoperative Day 7. The resected specimen revealed a 2.8 × 2.2 × 1.9 cm tan-brown firm mass, with IHC showing tumor cells diffusely positive for OSCAR, CD56, chromogranin and synaptophysin with a Ki-67 proliferative index of 1%, consistent with a grade 1, well-differentiated NET (Fig. 8). The right and left hepatic duct margins and clearly identifiable parenchymal margin were negative for malignancy. The case was presented at tumor board with recommendations for annual magnetic resonance imaging surveillance.
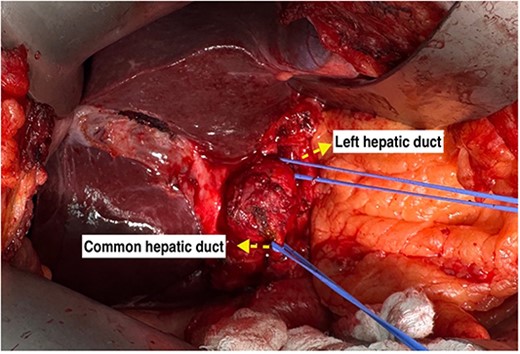
Extrahepatic tumor encasing the common hepatic duct and extending to the right and left hepatic ducts.
An intraoperative cholangiogram showing tumor involvement of the common hepatic duct up to the right and left hepatic ducts.

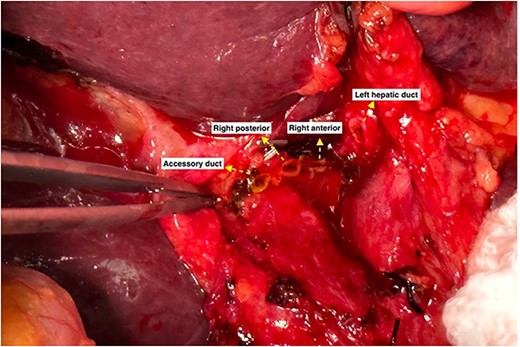
Three right bile duct openings (anterior, posterior and accessory).
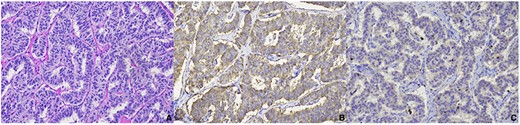
Microscopic examination of extrahepatic biliary mass resection demonstrated a well-differentiated NET; (A) monotonous tumor cells arranged in trabecular pattern, hematoxylin–eosin; (B) tumor cells were diffusely positive for chromogranin; (C) tumor cells showed Ki-67 proliferation activity of 1%; all photographs at 200x.
DISCUSSION
This is a rare case in which an EBNET was found incidentally in a relatively healthy 77-year-old gentleman undergoing a workup for fatty liver disease. Literature on this disease process is incredibly sparse and thus so are information on prognosis and recommendations on management. In contrast to the majority of previously reported EBNETs, this patient presented without signs of biliary obstruction and was entirely asymptomatic. Additionally, we were able to confidently obtain a preoperative diagnosis of NET via EUS with FNA. A PET/CT 68Ga-Dotatate scan was done to confirm no other possible primary tumors.
To date, only two EBNETs were diagnosed preoperatively based on endoscopic biopsy results [6, 7]. Difficulty in diagnosing EBNETs lies in their difficult to access location, whereas endoscopy appears to have the best results [1, 6, 7]. Diagnosis by brush biopsy has been previously described but has a high incidence of false negativity due to the largely submucosal nature of these tumors [3]. Therefore, an experienced endoscopist is crucial to obtain biopsy and in some cases may require combined surgical approach. Radu et al. [8] described a laparoscopy-assisted endoscopic retrograde pancreatography to obtain a biopsy specimen and preop diagnosis of an EBNET in a patient with a history of Roux-en-Y gastric bypass surgery.
Hepatic duct resection en bloc with the mass with hepaticojejunostomy reconstruction appears to be the most common surgical approach to EBNETs. Unique to our patient was the location of the EBNET encasing the perihilar hepatic ducts and proximal common hepatic duct. Surgical resection of this mass was complex and required an experienced surgical oncologist and a transplant surgeon to perform the meticulous hilar dissection and achieve adequate margins. In addition to the perihilar nature of the mass, the patient’s anatomy was unique in that he had three right hepatic ducts requiring multiple hepaticojejunostomy anastomoses. Despite the complexity of this operation, the patient tolerated his procedure remarkably well.
Accurate pathology review of the specimen is key in confirming the diagnosis and establishing prognosis. Chromogranin and synaptophysin appear to be the most commonly present markers on IHC. Ki-67 index is believed to be the most helpful in establishing the diagnosis with rates of <2% portending good long-term survival [3]. Additionally complete pathologic review of the specimen assists in ruling out mixed or composite tumor with non-neuroendocrine components which can suggest a more aggressive nature [9, 10].
In conclusion, we have demonstrated that preoperative diagnosis of an EBNET is possible and can help guide the remainder of preoperative workup, as well as surgical intervention. Surgical resection is feasible even for the most proximal EBNETs and may require a creative approach to hepaticojejunostomy reconstruction.
CONFLICT OF INTEREST STATEMENT
None declared.



