-
PDF
- Split View
-
Views
-
Cite
Cite
Yuki Julius Ng, Aaron Ling, Loke Jian Nam, Priscamy Siaman Tylors, Aminnur Hafiz Bin Maliki, Sharifah Ashrina Wan Ali, A case of acute motor sensory axonal neuropathy variant of Guillain Barre syndrome and anaphylaxis reaction as a complication from hyaluronic acid breast enhancement from an unlicensed beautician, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad254, https://doi.org/10.1093/jscr/rjad254
Close - Share Icon Share
Abstract
Guillain Barre syndrome (GBS) as a complication of hyaluronic acid (HA) exposure is an extremely rare occurrence. We report a case of GBS, acute motor sensory axonal neuropathy (AMSAN) variant, after a HA breast enhancement procedure. A 41-year-old lady underwent a HA breast enhancement procedure from an unlicensed beautician and developed anaphylaxis followed by bilateral breast abscess and neurological deficits involving both motor and sensory components. The AMSAN variant of GBS was diagnosed from the cytoalbuminologic dissociation and nerve conduction study. Her GBS and breast abscess were managed with plasmapheresis and bilateral mastectomy. In this case, GBS was highly suspected to be caused by HA with possible impurities. To the author’s knowledge, the association between HA and GBS has not been reported or known, and further studies are required to establish this association. To prevent mortality and morbidity, breast enhancement procedures should be performed by trained professionals with properly vetted products.
INTRODUCTION
Hyaluronic acid (HA) breast fillers are increasingly popular as they are generally safe, effective and performed as minimally invasive procedures [1]. The increased usage of HA fillers subsequently increased adverse effects such as swelling, bruising and infection [2]. These complications are reportedly higher when the procedure was done by an unlicensed beautician [3]. Breast abscess is the most common complication from an unlicensed beautician and Pseudomonas aeruginosa is the commonest isolated pathogen from the abscesses [4]. Guillain Barre syndrome (GBS) as a complication from breast fillers or P. aeruginosa has not been well described in the literature. We described a rare case of breast abscess secondary to P. aeruginosa infection post-HA breast filler, which was complicated with anaphylaxis and GBS.
CASE REPORT
A 41-year-old lady of Chinese ethnicity with previously no known medical illness was brought into the emergency department for anaphylactic shock post-breast enhancement procedure. She had a history of HA enhancement 3 months before this admission. For this admission, she visited another unlicensed beautician for breast enhancement with 250 ml of HA (Estee Pharma Taiwan) in each breast. Half an hour later, our patient experienced a sudden onset of dizziness, shortness of breath, swelling and tenderness over both breasts and was then sent to the hospital. Upon her arrival, she was speaking in phrases, her blood pressure was 75/35 mmHg, tachycardic with 103 beats per minute, SpO2 of 92%, respiratory rate of 34 with poor pulse volume and cold peripheries. Her anaphylaxis was managed with adrenaline infusion (0.5 mcg/kg/min), chlorphenamine (10 mg) and hydrocortisone (200 mg); her vitals stabilized and she was prophylactically intubated and admitted into the intensive care unit for ventilatory support. The timeline of her disease progression is illustrated in (Figure 1).
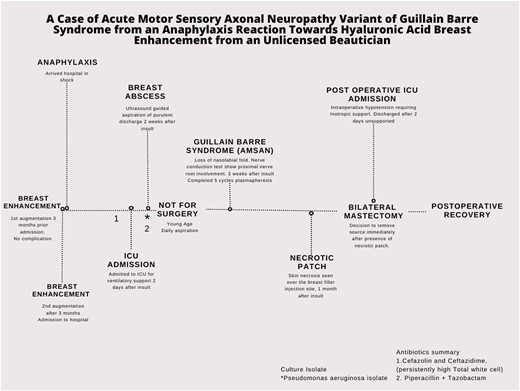
Initial bilateral ultrasound did not suggest the presence of abscesses. During her admission, 2 weeks after the breast filler, she developed a new onset bilateral breast pain. Examination showed bilateral breast swelling with erythema, warm to touch and tender on palpation with raised white cell count up to 38 × 103/μL. Ultrasound-guided aspiration demonstrated purulent discharge with a positive culture of P. aeruginosa, which was sensitive to tazobactam and piperacillin (Tazocin) bilaterally, and she was diagnosed with bilateral breast abscess which preceded sepsis. Her breast abscess was initially treated with ultrasound-guided aspiration and Tazocin; mastectomy was not considered because she was young. Three weeks after her admission, our patient developed bilateral loss of nasolabial folds, with dysarthria and proximal muscle group weakness. Neurological exam showed all proximal limb muscle weakness, areflexia over bilateral lower limbs and bilateral facial nerve palsy.
Investigation
Cerebrospinal fluid protein was 1.46 g/l (reference range: 0.15–0.45 g/l). Nerve conduction study (Tables 1–3, Fig. 2) suggested motor and sensory with axonal involvement. Her anti-ganglioside panel was negative. Computed tomography and magnetic resonance imaging of the brain was normal.
| Nerve/Sites . | Recording Site . | Onset Latency (ms) . | Peak Latency (ms) . | NP Amplitude (μV) . | PP Amplitude (μV) . | Segments . | Distance (cm) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|---|
| Right Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.6 | 3.23 | 43.5 | 66.4 | Wrist - Index | 15 | 58 |
| Left Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.14 | 3.02 | 51.5 | 75.1 | Wrist - Index | 14 | 66 |
| Right Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.82 | 2.55 | 38.3 | 56.9 | Wrist - Dig V | 12 | 66 |
| Left Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.88 | 2.6 | 30.2 | 47.7 | Wrist - Dig V | 14 | 75 |
| Right Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.56 | 2.14 | 29.2 | 27.8 | Forearm - Wrist | 10 | 64 |
| Left Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.3 | 1.93 | 49.6 | 46.2 | Forearm - Wrist | 10 | 77 |
| Right Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.71 | 3.59 | 4.7 | 5.6 | Calf - Ankle | 14 | 52 |
| Left Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.19 | 2.86 | 3.1 | 7.3 | Calf - Ankle | 12 | 55 |
| Right Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.12 | 2.5 | 3.3 | 4.7 | Lat Leg - Ankle | 12 | 56 |
| Left Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.08 | 2.46 | 7.4 | 8.3 | Lat Leg - Ankle | 12 | 58 |
| Nerve/Sites . | Recording Site . | Onset Latency (ms) . | Peak Latency (ms) . | NP Amplitude (μV) . | PP Amplitude (μV) . | Segments . | Distance (cm) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|---|
| Right Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.6 | 3.23 | 43.5 | 66.4 | Wrist - Index | 15 | 58 |
| Left Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.14 | 3.02 | 51.5 | 75.1 | Wrist - Index | 14 | 66 |
| Right Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.82 | 2.55 | 38.3 | 56.9 | Wrist - Dig V | 12 | 66 |
| Left Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.88 | 2.6 | 30.2 | 47.7 | Wrist - Dig V | 14 | 75 |
| Right Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.56 | 2.14 | 29.2 | 27.8 | Forearm - Wrist | 10 | 64 |
| Left Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.3 | 1.93 | 49.6 | 46.2 | Forearm - Wrist | 10 | 77 |
| Right Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.71 | 3.59 | 4.7 | 5.6 | Calf - Ankle | 14 | 52 |
| Left Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.19 | 2.86 | 3.1 | 7.3 | Calf - Ankle | 12 | 55 |
| Right Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.12 | 2.5 | 3.3 | 4.7 | Lat Leg - Ankle | 12 | 56 |
| Left Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.08 | 2.46 | 7.4 | 8.3 | Lat Leg - Ankle | 12 | 58 |
All sensory study were within normal limits.
| Nerve/Sites . | Recording Site . | Onset Latency (ms) . | Peak Latency (ms) . | NP Amplitude (μV) . | PP Amplitude (μV) . | Segments . | Distance (cm) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|---|
| Right Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.6 | 3.23 | 43.5 | 66.4 | Wrist - Index | 15 | 58 |
| Left Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.14 | 3.02 | 51.5 | 75.1 | Wrist - Index | 14 | 66 |
| Right Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.82 | 2.55 | 38.3 | 56.9 | Wrist - Dig V | 12 | 66 |
| Left Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.88 | 2.6 | 30.2 | 47.7 | Wrist - Dig V | 14 | 75 |
| Right Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.56 | 2.14 | 29.2 | 27.8 | Forearm - Wrist | 10 | 64 |
| Left Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.3 | 1.93 | 49.6 | 46.2 | Forearm - Wrist | 10 | 77 |
| Right Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.71 | 3.59 | 4.7 | 5.6 | Calf - Ankle | 14 | 52 |
| Left Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.19 | 2.86 | 3.1 | 7.3 | Calf - Ankle | 12 | 55 |
| Right Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.12 | 2.5 | 3.3 | 4.7 | Lat Leg - Ankle | 12 | 56 |
| Left Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.08 | 2.46 | 7.4 | 8.3 | Lat Leg - Ankle | 12 | 58 |
| Nerve/Sites . | Recording Site . | Onset Latency (ms) . | Peak Latency (ms) . | NP Amplitude (μV) . | PP Amplitude (μV) . | Segments . | Distance (cm) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|---|
| Right Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.6 | 3.23 | 43.5 | 66.4 | Wrist - Index | 15 | 58 |
| Left Median - Digit II (Antidromic) | ||||||||
| Wrist | Index | 2.14 | 3.02 | 51.5 | 75.1 | Wrist - Index | 14 | 66 |
| Right Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.82 | 2.55 | 38.3 | 56.9 | Wrist - Dig V | 12 | 66 |
| Left Ulnar - Digit V (Antidromic) | ||||||||
| Wrist | Digit V | 1.88 | 2.6 | 30.2 | 47.7 | Wrist - Dig V | 14 | 75 |
| Right Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.56 | 2.14 | 29.2 | 27.8 | Forearm - Wrist | 10 | 64 |
| Left Radial - Superficial (Antidromic) | ||||||||
| Forearm | Wrist | 1.3 | 1.93 | 49.6 | 46.2 | Forearm - Wrist | 10 | 77 |
| Right Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.71 | 3.59 | 4.7 | 5.6 | Calf - Ankle | 14 | 52 |
| Left Sural - (Antidromic) | ||||||||
| Calf | Ankle | 2.19 | 2.86 | 3.1 | 7.3 | Calf - Ankle | 12 | 55 |
| Right Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.12 | 2.5 | 3.3 | 4.7 | Lat Leg - Ankle | 12 | 56 |
| Left Superficial peroneal - (Antidromic) | ||||||||
| Lat Leg | Ankle | 2.08 | 2.46 | 7.4 | 8.3 | Lat Leg - Ankle | 12 | 58 |
All sensory study were within normal limits.
| Nerve/Sites . | Muscle . | Latency (ms) . | Amplitude (μV) . | Segments . | Distance (cm) . | Latency Difference (ms) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|
| Upper Limb | |||||||
| Right Median - Abductor pollicis brevis (APB) | |||||||
| Wrist | APB | 3.06 | 8.5 | Wrist - APB | 8 | ||
| Elbow | APB | 6.98 | 4.8 | Elbow - Wrist | 19 | 3.92 | 48.5 |
| Left Median - APB | |||||||
| Wrist | APB | 2.83 | 10.9 | Wrist - APB | 8 | ||
| Elbow | APB | 6.58 | 10.8 | Elbow - Wrist | 23 | 3.75 | 61.3 |
| Right Ulnar - Abductor Digiti Minimi (ADM) | |||||||
| Wrist | ADM | 2.54 | 5 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6.12 | 4.6 | B. Elbow - Wrist | 22 | 3.58 | 61.4 |
| A. Elbow | ADM | 7.71 | 5.2 | A. Elbow - B. Elbow | 10 | 1.58 | 63.2 |
| ADM | A. Elbow - Wrist | 32 | 5.17 | 61.9 | |||
| Left Ulnar - ADM | |||||||
| Wrist | ADM | 2.4 | 6.4 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6 | 6.6 | B. Elbow - Wrist | 23 | 3.6 | 63.8 |
| A. Elbow | ADM | 7.63 | 6.8 | A. Elbow - B. Elbow | 10 | 1.63 | 61.5 |
| ADM | A. Elbow - Wrist | 33 | 5.23 | 63.1 | |||
| Right Radial - Extensor Indicis Proprius (EIP) | |||||||
| Forearm | EIP | 2.92 | 1.5 | Forearm - EIP | |||
| Elbow | EIP | 4.9 | 1.7 | Elbow - Forearm | 13 | 1.98 | 65.7 |
| Spiral Gr | EIP | 4.69 | 1.6 | Spiral Gr - Elbow | 9 | −0.21 | 432 |
| Left Radial - EIP | |||||||
| Forearm | EIP | 3.04 | 2.0 | Forearm - EIP | |||
| Elbow | EIP | 4.83 | 2.0 | Elbow - Forearm | 11 | 1.79 | 61.4 |
| Spiral Gr | EIP | 5.88 | 1.9 | Spiral Gr - Elbow | 8 | 1.05 | 76.8 |
| Lower Limb | |||||||
| Right Tibial - Abductor Hallucis (AH) | |||||||
| Ankle | AH | 3.94 | 7.3 | Ankle - AH | 8 | ||
| Knee | AH | 11.38 | 6.6 | Knee - Ankle | 35 | 7.44 | 47.1 |
| Left Tibial - AH | |||||||
| Ankle | AH | 3.9 | 6.5 | Ankle - AH | 8 | ||
| Knee | AH | 11.98 | 4.8 | Knee - Ankle | 36 | 8.08 | 44.5 |
| Right Peroneal - Tibialis Anterior (Tib Ant) | |||||||
| Fib head | Tib Ant | 3.88 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 5.23 | 0.4 | Pop Fossa - Fib Head | 8 | 1.35 | 59.1 |
| Left Peroneal - Tib Ant | |||||||
| Fib head | Tib Ant | 3.83 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 4.63 | 0.5 | Pop Fossa - Fib Head | 8 | 0.79 | 101.1 |
| Right Peroneal - Extensor Digitorum Brevis (EDB) | |||||||
| Ankle | EDB | 4.15 | 0.6 | Ankle - EDB | 8 | ||
| B. Fib head | EDB | 11.5 | 0.8 | B. Fib Head - Ankle | 32 | 7.35 | 43.5 |
| A. Fib head | EDB | 12.33 | 0.9 | A. Fib Head - B. Fib Head | 8 | 0.83 | 96.0 |
| Left Peroneal - EDB | |||||||
| Ankle | EDB | NR | NR | Ankle - EDB | 8 | ||
| B. Fib head | EDB | B. Fib Head - Ankle | NR | ||||
| A. Fib head | EDB | A. Fib Head - B. Fib Head | |||||
| Nerve/Sites . | Muscle . | Latency (ms) . | Amplitude (μV) . | Segments . | Distance (cm) . | Latency Difference (ms) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|
| Upper Limb | |||||||
| Right Median - Abductor pollicis brevis (APB) | |||||||
| Wrist | APB | 3.06 | 8.5 | Wrist - APB | 8 | ||
| Elbow | APB | 6.98 | 4.8 | Elbow - Wrist | 19 | 3.92 | 48.5 |
| Left Median - APB | |||||||
| Wrist | APB | 2.83 | 10.9 | Wrist - APB | 8 | ||
| Elbow | APB | 6.58 | 10.8 | Elbow - Wrist | 23 | 3.75 | 61.3 |
| Right Ulnar - Abductor Digiti Minimi (ADM) | |||||||
| Wrist | ADM | 2.54 | 5 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6.12 | 4.6 | B. Elbow - Wrist | 22 | 3.58 | 61.4 |
| A. Elbow | ADM | 7.71 | 5.2 | A. Elbow - B. Elbow | 10 | 1.58 | 63.2 |
| ADM | A. Elbow - Wrist | 32 | 5.17 | 61.9 | |||
| Left Ulnar - ADM | |||||||
| Wrist | ADM | 2.4 | 6.4 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6 | 6.6 | B. Elbow - Wrist | 23 | 3.6 | 63.8 |
| A. Elbow | ADM | 7.63 | 6.8 | A. Elbow - B. Elbow | 10 | 1.63 | 61.5 |
| ADM | A. Elbow - Wrist | 33 | 5.23 | 63.1 | |||
| Right Radial - Extensor Indicis Proprius (EIP) | |||||||
| Forearm | EIP | 2.92 | 1.5 | Forearm - EIP | |||
| Elbow | EIP | 4.9 | 1.7 | Elbow - Forearm | 13 | 1.98 | 65.7 |
| Spiral Gr | EIP | 4.69 | 1.6 | Spiral Gr - Elbow | 9 | −0.21 | 432 |
| Left Radial - EIP | |||||||
| Forearm | EIP | 3.04 | 2.0 | Forearm - EIP | |||
| Elbow | EIP | 4.83 | 2.0 | Elbow - Forearm | 11 | 1.79 | 61.4 |
| Spiral Gr | EIP | 5.88 | 1.9 | Spiral Gr - Elbow | 8 | 1.05 | 76.8 |
| Lower Limb | |||||||
| Right Tibial - Abductor Hallucis (AH) | |||||||
| Ankle | AH | 3.94 | 7.3 | Ankle - AH | 8 | ||
| Knee | AH | 11.38 | 6.6 | Knee - Ankle | 35 | 7.44 | 47.1 |
| Left Tibial - AH | |||||||
| Ankle | AH | 3.9 | 6.5 | Ankle - AH | 8 | ||
| Knee | AH | 11.98 | 4.8 | Knee - Ankle | 36 | 8.08 | 44.5 |
| Right Peroneal - Tibialis Anterior (Tib Ant) | |||||||
| Fib head | Tib Ant | 3.88 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 5.23 | 0.4 | Pop Fossa - Fib Head | 8 | 1.35 | 59.1 |
| Left Peroneal - Tib Ant | |||||||
| Fib head | Tib Ant | 3.83 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 4.63 | 0.5 | Pop Fossa - Fib Head | 8 | 0.79 | 101.1 |
| Right Peroneal - Extensor Digitorum Brevis (EDB) | |||||||
| Ankle | EDB | 4.15 | 0.6 | Ankle - EDB | 8 | ||
| B. Fib head | EDB | 11.5 | 0.8 | B. Fib Head - Ankle | 32 | 7.35 | 43.5 |
| A. Fib head | EDB | 12.33 | 0.9 | A. Fib Head - B. Fib Head | 8 | 0.83 | 96.0 |
| Left Peroneal - EDB | |||||||
| Ankle | EDB | NR | NR | Ankle - EDB | 8 | ||
| B. Fib head | EDB | B. Fib Head - Ankle | NR | ||||
| A. Fib head | EDB | A. Fib Head - B. Fib Head | |||||
Bilateral peroneal and tibial motor studies showed small amplitudes.
| Nerve/Sites . | Muscle . | Latency (ms) . | Amplitude (μV) . | Segments . | Distance (cm) . | Latency Difference (ms) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|
| Upper Limb | |||||||
| Right Median - Abductor pollicis brevis (APB) | |||||||
| Wrist | APB | 3.06 | 8.5 | Wrist - APB | 8 | ||
| Elbow | APB | 6.98 | 4.8 | Elbow - Wrist | 19 | 3.92 | 48.5 |
| Left Median - APB | |||||||
| Wrist | APB | 2.83 | 10.9 | Wrist - APB | 8 | ||
| Elbow | APB | 6.58 | 10.8 | Elbow - Wrist | 23 | 3.75 | 61.3 |
| Right Ulnar - Abductor Digiti Minimi (ADM) | |||||||
| Wrist | ADM | 2.54 | 5 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6.12 | 4.6 | B. Elbow - Wrist | 22 | 3.58 | 61.4 |
| A. Elbow | ADM | 7.71 | 5.2 | A. Elbow - B. Elbow | 10 | 1.58 | 63.2 |
| ADM | A. Elbow - Wrist | 32 | 5.17 | 61.9 | |||
| Left Ulnar - ADM | |||||||
| Wrist | ADM | 2.4 | 6.4 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6 | 6.6 | B. Elbow - Wrist | 23 | 3.6 | 63.8 |
| A. Elbow | ADM | 7.63 | 6.8 | A. Elbow - B. Elbow | 10 | 1.63 | 61.5 |
| ADM | A. Elbow - Wrist | 33 | 5.23 | 63.1 | |||
| Right Radial - Extensor Indicis Proprius (EIP) | |||||||
| Forearm | EIP | 2.92 | 1.5 | Forearm - EIP | |||
| Elbow | EIP | 4.9 | 1.7 | Elbow - Forearm | 13 | 1.98 | 65.7 |
| Spiral Gr | EIP | 4.69 | 1.6 | Spiral Gr - Elbow | 9 | −0.21 | 432 |
| Left Radial - EIP | |||||||
| Forearm | EIP | 3.04 | 2.0 | Forearm - EIP | |||
| Elbow | EIP | 4.83 | 2.0 | Elbow - Forearm | 11 | 1.79 | 61.4 |
| Spiral Gr | EIP | 5.88 | 1.9 | Spiral Gr - Elbow | 8 | 1.05 | 76.8 |
| Lower Limb | |||||||
| Right Tibial - Abductor Hallucis (AH) | |||||||
| Ankle | AH | 3.94 | 7.3 | Ankle - AH | 8 | ||
| Knee | AH | 11.38 | 6.6 | Knee - Ankle | 35 | 7.44 | 47.1 |
| Left Tibial - AH | |||||||
| Ankle | AH | 3.9 | 6.5 | Ankle - AH | 8 | ||
| Knee | AH | 11.98 | 4.8 | Knee - Ankle | 36 | 8.08 | 44.5 |
| Right Peroneal - Tibialis Anterior (Tib Ant) | |||||||
| Fib head | Tib Ant | 3.88 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 5.23 | 0.4 | Pop Fossa - Fib Head | 8 | 1.35 | 59.1 |
| Left Peroneal - Tib Ant | |||||||
| Fib head | Tib Ant | 3.83 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 4.63 | 0.5 | Pop Fossa - Fib Head | 8 | 0.79 | 101.1 |
| Right Peroneal - Extensor Digitorum Brevis (EDB) | |||||||
| Ankle | EDB | 4.15 | 0.6 | Ankle - EDB | 8 | ||
| B. Fib head | EDB | 11.5 | 0.8 | B. Fib Head - Ankle | 32 | 7.35 | 43.5 |
| A. Fib head | EDB | 12.33 | 0.9 | A. Fib Head - B. Fib Head | 8 | 0.83 | 96.0 |
| Left Peroneal - EDB | |||||||
| Ankle | EDB | NR | NR | Ankle - EDB | 8 | ||
| B. Fib head | EDB | B. Fib Head - Ankle | NR | ||||
| A. Fib head | EDB | A. Fib Head - B. Fib Head | |||||
| Nerve/Sites . | Muscle . | Latency (ms) . | Amplitude (μV) . | Segments . | Distance (cm) . | Latency Difference (ms) . | Velocity (m/s) . |
|---|---|---|---|---|---|---|---|
| Upper Limb | |||||||
| Right Median - Abductor pollicis brevis (APB) | |||||||
| Wrist | APB | 3.06 | 8.5 | Wrist - APB | 8 | ||
| Elbow | APB | 6.98 | 4.8 | Elbow - Wrist | 19 | 3.92 | 48.5 |
| Left Median - APB | |||||||
| Wrist | APB | 2.83 | 10.9 | Wrist - APB | 8 | ||
| Elbow | APB | 6.58 | 10.8 | Elbow - Wrist | 23 | 3.75 | 61.3 |
| Right Ulnar - Abductor Digiti Minimi (ADM) | |||||||
| Wrist | ADM | 2.54 | 5 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6.12 | 4.6 | B. Elbow - Wrist | 22 | 3.58 | 61.4 |
| A. Elbow | ADM | 7.71 | 5.2 | A. Elbow - B. Elbow | 10 | 1.58 | 63.2 |
| ADM | A. Elbow - Wrist | 32 | 5.17 | 61.9 | |||
| Left Ulnar - ADM | |||||||
| Wrist | ADM | 2.4 | 6.4 | Wrist - ADM | 8 | ||
| B. Elbow | ADM | 6 | 6.6 | B. Elbow - Wrist | 23 | 3.6 | 63.8 |
| A. Elbow | ADM | 7.63 | 6.8 | A. Elbow - B. Elbow | 10 | 1.63 | 61.5 |
| ADM | A. Elbow - Wrist | 33 | 5.23 | 63.1 | |||
| Right Radial - Extensor Indicis Proprius (EIP) | |||||||
| Forearm | EIP | 2.92 | 1.5 | Forearm - EIP | |||
| Elbow | EIP | 4.9 | 1.7 | Elbow - Forearm | 13 | 1.98 | 65.7 |
| Spiral Gr | EIP | 4.69 | 1.6 | Spiral Gr - Elbow | 9 | −0.21 | 432 |
| Left Radial - EIP | |||||||
| Forearm | EIP | 3.04 | 2.0 | Forearm - EIP | |||
| Elbow | EIP | 4.83 | 2.0 | Elbow - Forearm | 11 | 1.79 | 61.4 |
| Spiral Gr | EIP | 5.88 | 1.9 | Spiral Gr - Elbow | 8 | 1.05 | 76.8 |
| Lower Limb | |||||||
| Right Tibial - Abductor Hallucis (AH) | |||||||
| Ankle | AH | 3.94 | 7.3 | Ankle - AH | 8 | ||
| Knee | AH | 11.38 | 6.6 | Knee - Ankle | 35 | 7.44 | 47.1 |
| Left Tibial - AH | |||||||
| Ankle | AH | 3.9 | 6.5 | Ankle - AH | 8 | ||
| Knee | AH | 11.98 | 4.8 | Knee - Ankle | 36 | 8.08 | 44.5 |
| Right Peroneal - Tibialis Anterior (Tib Ant) | |||||||
| Fib head | Tib Ant | 3.88 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 5.23 | 0.4 | Pop Fossa - Fib Head | 8 | 1.35 | 59.1 |
| Left Peroneal - Tib Ant | |||||||
| Fib head | Tib Ant | 3.83 | 0.4 | Fib Head - Tib Ant | |||
| Pop Fossa | Tib Ant | 4.63 | 0.5 | Pop Fossa - Fib Head | 8 | 0.79 | 101.1 |
| Right Peroneal - Extensor Digitorum Brevis (EDB) | |||||||
| Ankle | EDB | 4.15 | 0.6 | Ankle - EDB | 8 | ||
| B. Fib head | EDB | 11.5 | 0.8 | B. Fib Head - Ankle | 32 | 7.35 | 43.5 |
| A. Fib head | EDB | 12.33 | 0.9 | A. Fib Head - B. Fib Head | 8 | 0.83 | 96.0 |
| Left Peroneal - EDB | |||||||
| Ankle | EDB | NR | NR | Ankle - EDB | 8 | ||
| B. Fib head | EDB | B. Fib Head - Ankle | NR | ||||
| A. Fib head | EDB | A. Fib Head - B. Fib Head | |||||
Bilateral peroneal and tibial motor studies showed small amplitudes.
| Nerve . | F Latency (ms) . | M Latency (ms) . | F - M Latency (ms) . |
|---|---|---|---|
| Right Median - APB | 30.8 | 3.3 | 27.4 |
| Right Ulnar - ADM | NR | NR | NR |
| Right Peroneal - EDB | NR | NR | NR |
| Right Tibial - AH | 46.4 | 4.1 | 42.3 |
| Left Tibial - AH | 40.9 | 3.9 | 37 |
| Left Median - APB | NR | NR | NR |
| Left Ulnar - ADM | NR | NR | NR |
| Nerve . | F Latency (ms) . | M Latency (ms) . | F - M Latency (ms) . |
|---|---|---|---|
| Right Median - APB | 30.8 | 3.3 | 27.4 |
| Right Ulnar - ADM | NR | NR | NR |
| Right Peroneal - EDB | NR | NR | NR |
| Right Tibial - AH | 46.4 | 4.1 | 42.3 |
| Left Tibial - AH | 40.9 | 3.9 | 37 |
| Left Median - APB | NR | NR | NR |
| Left Ulnar - ADM | NR | NR | NR |
F waves were absent except Right median and bilateral tibial F wave study.
| Nerve . | F Latency (ms) . | M Latency (ms) . | F - M Latency (ms) . |
|---|---|---|---|
| Right Median - APB | 30.8 | 3.3 | 27.4 |
| Right Ulnar - ADM | NR | NR | NR |
| Right Peroneal - EDB | NR | NR | NR |
| Right Tibial - AH | 46.4 | 4.1 | 42.3 |
| Left Tibial - AH | 40.9 | 3.9 | 37 |
| Left Median - APB | NR | NR | NR |
| Left Ulnar - ADM | NR | NR | NR |
| Nerve . | F Latency (ms) . | M Latency (ms) . | F - M Latency (ms) . |
|---|---|---|---|
| Right Median - APB | 30.8 | 3.3 | 27.4 |
| Right Ulnar - ADM | NR | NR | NR |
| Right Peroneal - EDB | NR | NR | NR |
| Right Tibial - AH | 46.4 | 4.1 | 42.3 |
| Left Tibial - AH | 40.9 | 3.9 | 37 |
| Left Median - APB | NR | NR | NR |
| Left Ulnar - ADM | NR | NR | NR |
F waves were absent except Right median and bilateral tibial F wave study.
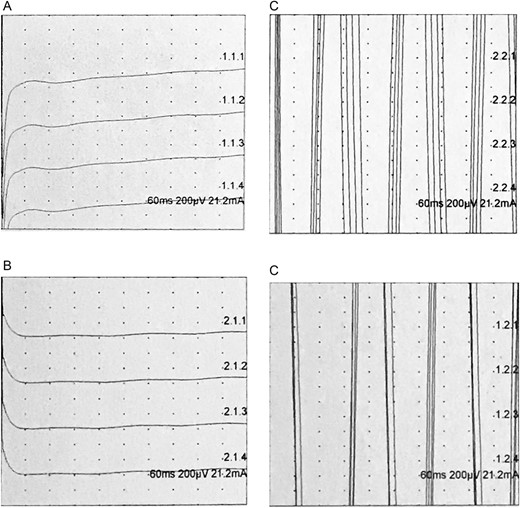
(A) Trigeminal orb oculi bilateral left ipsilateral; (B) Trigeminal orb oculi bilateral right contralateral; (C) Trigeminal orb oculi bilateral right ipsilateral; (D) Trigeminal orb oculi bilateral left contralateral; blink reflex of left R1 and R2 were absent where right R1 and R2 were unrecordable due to interference from the ventilator; this is consistent with facial neuropathy.
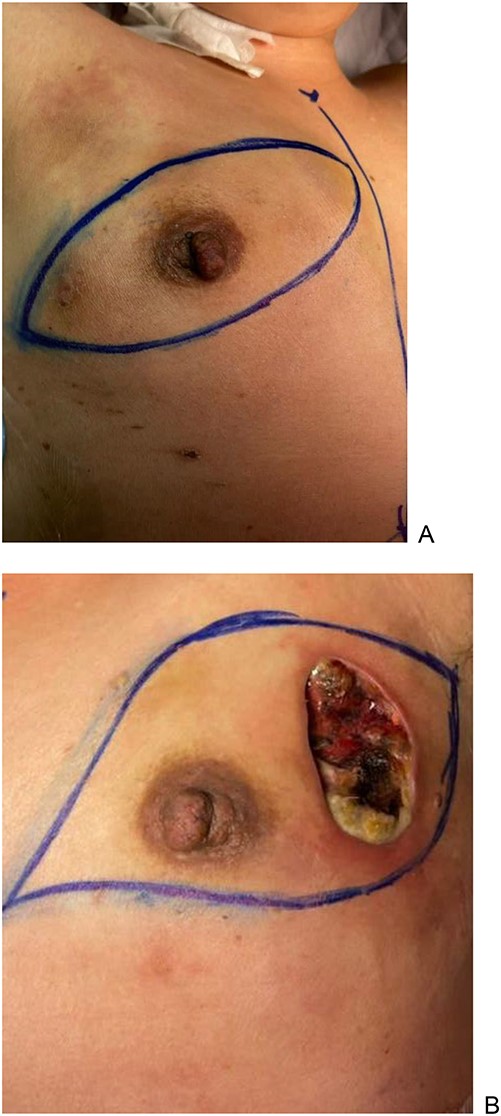
She was diagnosed with GBS, acute motor sensory axonal neuropathy (AMSAN) variant by the neuromedical team as evidenced by the cytoalbuminologic dissociation and nerve conduction study (Fig. 2). Her GBS was managed with five cycles of plasmapheresis. One month after the breast augmentation, she deteriorated clinically with worsening sepsis, formation of a necrotic patch and persistently requiring bedside aspiration; bilateral mastectomy was decided as a definitive treatment.
Post-operatively, our patient recovered well, and her inflammatory markers and total white cells reduced down to baseline. She was able to ambulate and tolerate orally and was able to be discharged after physiotherapy.
Histopathological exam of specimen
Macroscopic exam of the breast specimen (Fig. 3) showed patchy necrosis with pus. Breast tissue showed fibrotic change with multiple, various-sized cysts containing viscous translucent fluid. Microscopic exam showed extensive fat necrosis, multiple microabscesses with inflammatory infiltrate extending into the skeletal muscle bundles with interstitial edema and fibrosis.
Follow-up
During her follow-up, she was able to ambulate independently without support, scoring modified rankin scale 1. She recovered well and continued with outpatient occupational therapy and physiotherapy.
DISCUSSION
GBS is the most common cause of acute inflammatory polyradiculopathy which affects ~100 000 people worldwide annually [5]. GBS usually presents within 6 weeks, but it can present from 2 days to 6 months from an immune response against pathogens, causing a molecular mimicry against gangliosides in peripheral nerves [6]. Some of the common pathogens are Campylobacter jejuni, cytomegalovirus, influenza A and B and human immunodeficiency virus [7, 8]. GBS is typically diagnosed with a clinical presentation of ascending neurological signs and symptoms with a presence of cytoalbuminologic dissociation [8]. Our NCS (Table 1) shows an absence of blink reflex, reflecting the loss of sensory and motor components. The bilateral peroneal and tibialis anterior had a reduced amplitude while maintaining normal velocity, increasing the suspicion of axonal involvement [9]. The F waves were either not recordable or normal, which supports our suspicion of GBS [9]. Our patient was diagnosed with the AMSAN variant of GBS supported by the cytoalbuminologic dissociation and the NCS.
We suspect the second HA caused the anaphylaxis reaction that further precipitated into GBS. According to the literature, adverse reaction toward HA was from 0.15 to 0.42%. Among those adverse reactions, anaphylaxis was proposed to be caused by HA that was mixed with additives or impurities [10]. Among those with adverse reactions, histological reports have shown granulomatous reactions toward HA with impurities from the purification processes; however, this is considered to be rare as the purification process has significantly improved in the current era [11]. The anaphylaxis was triggered after the second HA with a different brand, and this raised suspicion of its content with additives.
Only one case report suggested the possible cause of GBS was from P. aeruginosa; however, more studies are needed to conclude this statement [12]. The cause of GBS from P. aeruginosa was considered to be extremely rare in comparison to the potential risk of molecular mimicry against HA; therefore, we did not consider P. aeruginosa to be the cause of GBS in our patient. Clinically, GBS manifested at 3 weeks after the insult, which is well within the common timeline of presentation of within 6 weeks [6].
This case highlights the importance of the awareness of the public to choose a legitimate beautician for invasive procedures. The public health officers have the responsibility of quality controlling the products and regulating illegitimate service providers for the interest of public health following the mantra of ‘Primum non-nocere’.
CONCLUSION
Hypersensitivity and GBS as a complication of HA are extremely rare. Nonetheless, any medical procedure should be conducted by a trained and licensed body. To the author’s knowledge, GBS as a complication from HA has not been reported in the literature and requires further studies to properly establish its association and pathophysiology.
Learning points
Although extremely rare, HA can cause anaphylaxis and could be life-threatening.
HA fillers may cause GBS and increase morbidity, reducing the quality of life.
Any invasive procedures should be conducted by a licensed beautician who has undergone training. Regular checks may be required as decided by the local governing bodies to ensure strict adherence to safety regulations.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No financial support was given to this case report writing.
DATA AVAILABILITY
Data are available from YJN with the permission of the patient. The data that support the findings of this study are available from the corresponding author, YJN, upon reasonable request.



