-
PDF
- Split View
-
Views
-
Cite
Cite
Joshua C Hurwitz, Christine E Kolwitz, David Y Kim, Patrizio Petrone, David K Halpern, Robotic-assisted completion cholecystectomy with repair of cholecystoduodenal fistula, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad251, https://doi.org/10.1093/jscr/rjad251
Close - Share Icon Share
Abstract
Post-cholecystectomy syndrome (PCS) is a well-documented complication of incomplete cholecystectomy. The etiology is often post-surgical chronic inflammation from unresolved cholelithiasis, which is secondary to anatomical abnormalities, including a retained gallbladder or a large cystic duct remnant (CDR). An exceedingly rare consequence is retained gallstone fistulization into the gastrointestinal tract. We present a case of a 70-year-old female with multiple comorbidities 4 years status-post incomplete cholecystectomy, who developed PCS with cholecystoduodenal fistula secondary to retained gallstone in the remnant gallbladder, with CDR involvement, treated via robotic-assisted surgery. Reoperation in PCS has been traditionally performed via laparoscopic approach with recent advances made in robotic-assisted surgery. However, we report the first documented case of PCS complicated by bilioenteric fistula repaired with robotic-assisted surgery. This highlights the value of robotic-assisted surgery in complicated cases, where one must contend with post-surgical anatomic abnormalities and visualization difficulties. Subsequent investigation is necessary to objectively quantify the safety and reproducibility of our approach.
INTRODUCTION
Post-cholecystectomy syndrome (PCS) is a known potential sequela of cholecystectomy, particularly in cases complicated by difficult anatomy and pathology that make gallbladder identification and proper dissection difficult. Up to 5% of patients experience PCS, presenting with symptoms that tend to mimic their initial presentation before cholecystectomy. Etiologies of PCS include biliary stricture, retained calculi, remnant gallbladder or cystic duct remnant (CDR). A CDR is a remnant duct greater than 1 cm, and in the presence of gallstones, it can be involved in PCS. A CDR without associated lithiasis is usually asymptomatic [1]. Beyond PCS, one possible sequela of gallbladder remnant inflammation is retained gallstone fistulization into the gastrointestinal tract [2].
We present a case of PCS due to remnant gallbladder with associated CDR, complicated by cholecystoduodenal fistula secondary to retained gallstone. The patient was treated via robotic-assisted surgery.
CASE REPORT
This is the case of a 70-year-old female with a history of hypothyroidism, hiatal hernia, irritable bowel syndrome and obstructive sleep apnea, with a surgical history of open small bowel resection due to endometriosis 46 years prior, total abdominal hysterectomy 40 years prior and laparoscopic cholecystectomy 4 years prior at an outside institution. She presented with colicky right upper quadrant abdominal pain similar to previous gallbladder attack. She was hemodynamically stable and afebrile. Labs were notable for leukocytosis, with a count of 14.9 k/ml and neutrophilia of 87%. Hepatic enzymes and bilirubin levels were unremarkable. A computed tomography (CT) scan of abdomen/pelvis demonstrated a 2.2 × 1.9 cm peripherally enhancing tubular/cystic structure in the gallbladder fossa, containing air and fluid, contiguous with postsurgical clips (Fig. 1). Surrounding fluid and fatty infiltration were observed. Findings raised the possibility of a dilated CDR with superimposed infection. No intrahepatic ductal dilatation was observed. The patient was discharged on oral Augmentin 875–125 mg bid and scheduled for interval surgical intervention, 10 days later.
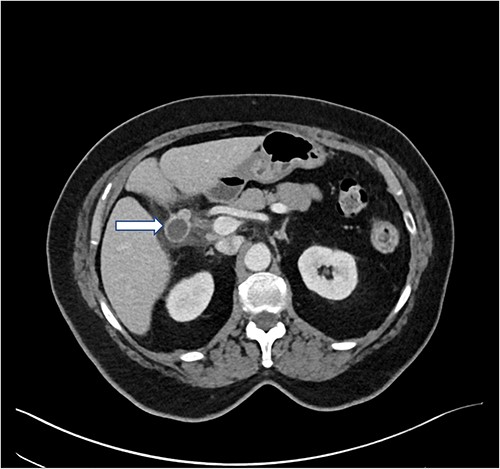
Preoperative CT abdomen/pelvis with IV contrast. In the gallbladder fossa, a 2.2 × 1.9 cm peripherally enhancing tubular/cystic structure is observed (arrow), dilated with air and fluid and contiguous with postsurgical clips, status post cholecystectomy. Moderate surrounding fluid and fatty infiltration are observed. The findings raised the possibility of a dilated remnant cystic duct with superinfection, abscess or less likely, biloma. Neither intrahepatic duct nor common bile duct dilatation was observed. There was concern for probable adjacent secondary duodenitis. Minimal pelvic ascites was observed.
Initial access was obtained via a Hasson entry at the umbilicus. In total, four robotic ports were placed in the normal fashion for robotic cholecystectomy. The robot (DaVinci XI) was docked over the patient’s left side and set up with two left-hand instruments: one tip-up fenestrated grasper and the other a force bipolar, both used primarily for retraction throughout the case. Dissection was carried out via the right hand with a combination of the monopolar curved scissors and permanent cautery hook, changing between the two instruments as needed. Dissection began at the gallbladder fossa where chronic inflammatory phlegmon was encountered. Indocyanine green (ICG) cholangiography was used to help with visualization of the common bile duct. A formal trans-cystic cholangiogram was performed to confirm anatomy and demonstrated no evidence of intraductal calculi. The cystic duct was clipped, divided, and gently retracted anteriorly. The remnant gallbladder was separated from the surrounding structures. At this time, it was clear that a fistula between the infundibulum of the remnant gallbladder and the duodenum was present. The fistula was divided and resected. The duodenotomy was repaired with interrupted 3–0 silk sutures and buttressed with a piece of omental fat. The total operating time was 4 h.
Postoperatively, the patient was admitted for management with nasogastric tube and bowel rest. She was discharged home on postoperative day 4 on a regular diet in good condition.
DISCUSSION
Patients with cholecystoenteric fistulization present with varied symptoms. If the biliary system is decompressed, some may be completely asymptomatic. Others may present with jaundice, pain, fever or intestinal obstruction from gallstone ileus. Using CT with contrast, the correct diagnosis of bilioenteric fistula can sometimes be delineated prior to diagnostic laparoscopy. Imaging can demonstrate pneumobilia or the fistula itself; air in the biliary tree is the hallmark finding [2]. The most common type of bilioenteric fistula is a cholecystoduodenal fistula (75–80% of cases) [3]. Chronic inflammation is necessary in pathogenesis, and nearly all cases involve gallstone penetration through the enteric wall [4]. Even with suspected CDR involvement, surgery is the first-line definitive treatment as alternative approaches such as ERCP do not allow for diversion of the fistula and excision of the CDR. Laparoscopic completion cholecystectomy is the predominant approach [5, 6].
Though less common than traditional laparoscopic surgery, robotic-assisted surgery has been well documented as an effective approach to complete cholecystectomy. In a retrospective cohort study of 26 patients who underwent robotic-assisted completion cholecystectomy, the mean operative time was 142 min, and the median length of stay was 1 day with one readmission. Three patients experienced minor (Clavien-Dindo ≤ II) complications [7]. In a case series of robotic-assisted completion cholecystectomy, all three patients initially presented with gangrenous cholecystitis treated with subtotal cholecystectomy to avoid iatrogenic damage to the common bile duct. As a result of anticipated complexity of completion cholecystectomy, the DaVinci robot was used. The median operating time was 153 min, and the median length of stay was 1 day without complications [8].
Moreover, Van Manen et al. [9] demonstrate the utility of the robotic-assisted approach in completion cholecystectomy with CDR involvement, particularly when using ICG to visualize the CDR, as was done in our case. Due to inherent technical and anatomical difficulties, the robotic approach proved safest and most effective. Completion cholecystectomy necessitates delineation of potentially distorted anatomy in the setting of adhesions and postoperative changes, and a robotic approach maximizes the surgeon’s visualization and facility.
PCS complicated by cholecystoduodenal fistula is an exceedingly rare pathology that requires precise treatment given the precarious nature of necessary operative intervention in a delicate anatomic location. PCS treatment is well documented: traditionally performed via laparoscopic approach and more recently treated with robotic-assisted surgery. However, to our knowledge, PCS complicated by cholecystoduodenal fistula repaired with a robotic-assisted approach has not been reported in the literature. Thus, our case details the progress that has been made as we maximize the utility of our technology. With a robotic-assisted approach, greater motility enhances the surgeon’s dexterity, and ICG visualization of the anatomy allows for confirmation of structures as well as investigation of a CDR, all contributing to better patient outcomes. Further studies are necessary to document the safety and reproducibility of robotic-assisted surgical procedures for treatment of this rare sequelae of cholecystectomy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The data that support the findings of this study are available on request.
References
- cholecystectomy
- pathologic fistula
- biliary calculi
- comorbidity
- cystic duct
- laparoscopy
- postcholecystectomy syndrome
- repeat surgery
- safety
- surgical procedures, operative
- gallbladder
- gastrointestinal tract
- chronic inflammation
- robotic surgery
- causality
- cholecystoduodenal fistula
- cholelithiasis
- diversion procedure



