-
PDF
- Split View
-
Views
-
Cite
Cite
Phyu C Thant, Anurag Gupta, Agenesis of gallbladder—an unexpected absence in laparoscopy, Journal of Surgical Case Reports, Volume 2023, Issue 4, April 2023, rjad214, https://doi.org/10.1093/jscr/rjad214
Close - Share Icon Share
Abstract
Gallbladder agenesis is a very rare condition, majority of which are normally diagnosed intraoperatively because of low index of suspicion and high rate of false positive results for cholecystitis on ultrasound imaging. We present a case of a 25-year-old man who presented with a right upper quadrant pain, whose ultrasound suggests a contracted gallbladder with gallstones. He was treated as an acute on chronic cholecystitis and booked for laparoscopic cholecystectomy. Intraoperatively, there was no gallbladder to be seen and decision was made to abandon procedure and avoid further exploration. Post-operative magnetic resonance cholangiopancreatography confirmed the congenital agenesis of gallbladder. It is important to have awareness of this condition, and possible further imaging modalities should be used if the ultrasound suggests a shrunken or contracted gallbladder that is not easily visible to avoid the risk of undergoing an unwarranted surgery.
INTRODUCTION
Gallbladder agenesis is a rare congenital anatomical variation, with an incidence rate of 10–65 per 100 000. It is three times more common in females than males [1, 2]. Whilst half of the patients with this anomaly are asymptomatic, the other half typically presents with symptoms akin to biliary colic or cholecystitis [1, 3]. Upper abdominal ultrasound is a first-line imaging for the diagnosis of cholelithiasis with a sensitivity of 97%, but in gallbladder agenesis, the sensitivity decreases to 61% [2, 4] and erroneous report of cholelithiasis or shrunken gallbladder suggestive of chronic cholecystitis is often made. Magnetic resonance cholangiopancreatography (MRCP) is the investigation of choice for the pre-operative diagnosis of gallbladder agenesis [4]. However, the combination of low index of suspicion for this rare condition and inaccurate ultrasound findings means that the correct diagnosis of gallbladder agenesis is often determined intraoperatively during an attempted laparoscopic cholecystectomy.
We present the first case of gallbladder agenesis reported in South Australia noted during laparoscopy for the presumed pre-operative diagnosis of cholecystitis.
CASE REPORT
A 25-year-old man presented to the hospital with 1-day history of right upper abdominal pain with a similar episode a week prior. He was otherwise fit and healthy with no other medical or surgical history. In the emergency department, he was haemodynamically normal, and he had right upper quadrant abdominal tenderness. His blood tests show normal inflammatory markers and normal liver function tests (LFTs). He had an ultrasound of the upper abdomen, which reported a difficult visualization of the gallbladder that was nearly completely contracted around calcific stones. There was no definite wall hyperaemia but appears thickened, and probe tenderness was present (see Fig. 1). He was diagnosed with acute on chronic cholecystitis and antibiotics were commenced. Symptoms improved so he was subsequently discharged with plan for an elective laparoscopic cholecystectomy in the next 2 weeks.
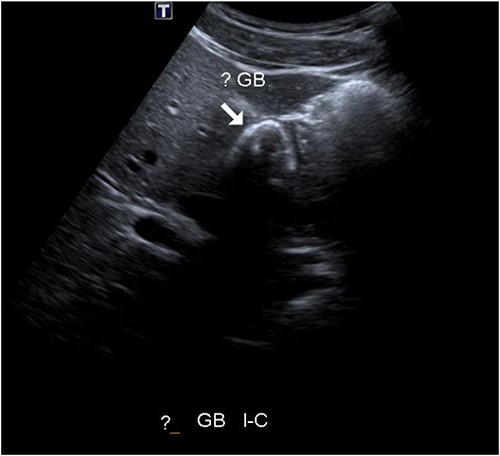
Abdominal ultrasound showing potential contracted gallbladder.
Intraoperatively, there was no gallbladder seen (Fig. 2). The examination of right and left subhepatic space, and portal region was done. The anatomy looked unremarkable other than the absence of a gallbladder. Another surgeon was called into theatre for a second opinion who agreed with the findings or lack thereof; hence the intended operation was abandoned and only a diagnostic laparoscopy was completed.
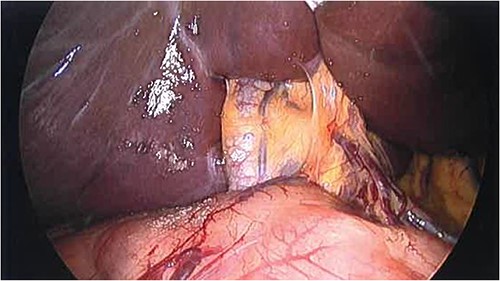
Intraoperative finding of the absence of gallbladder and cystic duct—common bile duct noted entering the liver.
The patient was discharged home on recovery and planned for outpatient MRCP and repeat LFTs. MRCP showed no gallbladder or cystic duct identified consistent with congenital agenesis (Figs 3 and 4). CBD was mildly dilated to 9 mm but tapers appropriately to the ampulla with no evidence of biliary stricture or choledocholithiasis. The repeat LFTs were normal.
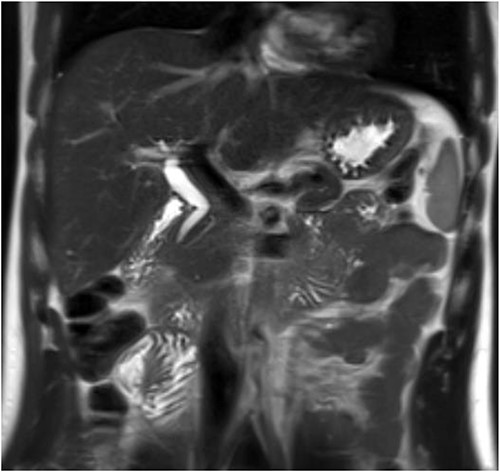
Post-operative MRCP confirming congenital gallbladder agenesis.
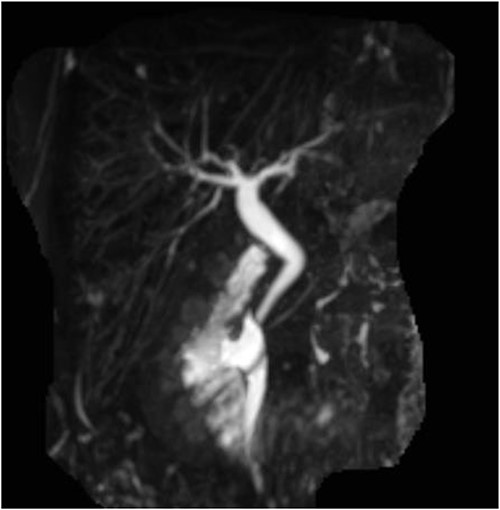
Post-operative MRCP confirming congenital gallbladder agenesis.
He was reviewed in outpatients following these investigations. He remained well postoperatively with no further symptoms. He was discharged from surgical follow-up.
DISCUSSION
Around 70% of gallbladder agenesis is a sporadic congenital malformation [5]. The rest are associated with other congenital malformations, with limited reports of familial hereditary links. Presentation of gallbladder agenesis has been divided into three groups as per Bennion et al. [6]: (i) symptomatic group presenting with symptoms of biliary colic making up 50%, (ii) asymptomatic group where gallbladder agenesis is found incidentally on autopsy making up 35%, and (iii) in neonates with multiple foetal anomalies making up 15%.
The symptoms reported consist of right upper quadrant pain (90%), nausea and vomiting (66%), fat intolerance (37%), dyspepsia (30%) and jaundice (35%) [1, 7]. The underlying mechanism of the biliary colic symptoms in gallbladder agenesis is thought to be from dysfunction of sphincter of Oddi and biliary dyskinesia [3]. As in our case, biochemical parameters are usually normal in cases of gallbladder agenesis [8].
Abdominal ultrasound is the initial investigation used when suspicious for biliary pathology because of its high sensitivity in diagnosing gallstones; however, its accuracy depends on operator experience and patient’s body habitus [2]. In gallbladder agenesis, false positive results are most frequently reported as ‘shrunken’, ‘contracted’ or ‘constricted’ gallbladder with hyperechoic shadowing suggestive of gallstones [8]. These can be attributed to bowel gas artefact, inflamed periportal tissue or subhepatic folds [2, 9].
Further imaging should be performed in these scenarios to achieve a more accurate diagnosis as per a suggested diagnostic algorithm by Malde [9]. Hepatobiliary iminodiacetic acid scan, computer topography scan and endoscopic retrograde cholangiopancreatography can be used for the diagnosis of gallbladder agenesis. However, non-visualization of the gallbladder can often be attributed to cystic duct obstruction, anatomical variation or technical errors, and therefore, generally proceed to surgery where the diagnosis is made [9]. MRCP is the imaging of choice for diagnosing gallbladder agenesis because of being non-invasive and providing detailed examination of the biliary tract. Even if the condition is diagnosed intraoperatively, MRCP (or other imaging as described above if contradicted) is suggested post-operatively to exclude an ectopic gallbladder [4].
Multiple recent case reports and reviews suggest that when the diagnosis of gallbladder agenesis is made during attempted laparoscopic cholecystectomy, it is advised to abort the procedure rather than risk complications from a prolonged open exploration for an ectopic gallbladder [1, 3, 4, 10, 11].
It has been noted that the majority of patients had resolution of symptoms after nontherapeutic surgery, such as in our case [1]. The reason for this is unclear—one hypothesis is lysis of periportal and right hypochondrial adhesions [7], though our patient did not have any previous abdominal surgeries, nor any congenital adhesions noted. Once gallbladder agenesis is confirmed and the patient remains symptomatic, conservative management with smooth muscle relaxants should be done, followed by sphincterotomy if this fails [9].
In conclusion, lack of awareness of congenital gallbladder agenesis by clinicians and relatively high rate of false positive result suggestive of shrunken gallbladder on initial ultrasound imaging means that correct diagnosis is still being made intraoperatively during an unnecessary surgery. When this occurs, it is important to prevent risk of complications of iatrogenic injury by avoiding prolonged exploration in search for an ectopic gallbladder. Hence, we present this case to add to the literature to increase the awareness of gallbladder agenesis and suggest further pre-operative imaging for confirmation of diagnosis to avoid unnecessary procedures.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
Ethical approval was waived by the authors’ institution.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal on request.



