-
PDF
- Split View
-
Views
-
Cite
Cite
Vinay Goyal, Mohanad Elshiekh, Kyle Drinnon, Yanna Puckett, Small bowel ischemia secondary to gastric pacemaker wires—a case report, Journal of Surgical Case Reports, Volume 2023, Issue 4, April 2023, rjad174, https://doi.org/10.1093/jscr/rjad174
Close - Share Icon Share
Abstract
Gastric stimulator has been used as a surgical option for patients with gastroparesis refractory to medical management. Only one previous report of small bowel gangrene secondary to gastric pacemaker wires has been reported in the literature. Our patient was a 38-year-old woman with a history of systemic lupus erythematosus and history of total colectomy who underwent an uneventful open gastric pacemaker placement for idiopathic gastroparesis. Four months after the initial placement of the pacemaker, she presented to the emergency department with acute abdominal pain and was found to have gangrene of 140 cm of small bowel secondary to looping of gastric pacemaker wires around small bowel mesentery. She underwent uneventful small bowel resection and anastomosis with an ileorectal anastomosis. This case highlights the need for a high index of suspicion for this catastrophic complication in patients with gastric pacemakers.
INTRODUCTION
Gastroparesis is a gastric motility disorder. Gastric pacemaker is a surgical option available for patients who have failed dietary modifications and medications [1]. Our technique for open gastric stimulator placement involves, implantation of two electrical leads into the anterior gastric wall near the greater curvature, 10 cm proximal to the gastric antrum through an upper midline incision. These wires from stomach are carried intraperitoneally in the supracolic compartment and exited through the abdominal wall in the right upper abdomen. The wires are then connected to the battery placed in a subcutaneous pocket in the right upper quadrant keeping them in supra colic compartment all along. Excess wires are coiled under the battery leaving no redundancy in the wires intraperitoneally.
CASE REPORT
Our patient was a 38-year-old woman with a history of systemic lupus erythematosus (SLE) who underwent an uneventful open gastric stimulator placement for idiopathic gastroparesis. Past surgical history was significant for a total colectomy with ileo-rectal anastomosis for lupus colitis and she was on oral steroids for SLE at the time of the pacemaker insertion. Three months later, she presented with complaints of frequent flipping of the battery in the subcutaneous pocket and underwent a revision of the pocket. One month after this pocket revision (4 months after the initial placement of the pacemaker), she presented to ER with acute abdominal pain for 3 days associated with nausea and vomiting. On physical examination, her abdomen was tender to palpation over the epigastrium with guarding. Laboratory studies revealed a very low white-cell count of 1118 per cubic millimeter (normal 4000–11 000) and an elevated serum lactate level of 5.6 mmol per liter (normal 0.5–2.2). CT revealed diffuse bowel dilation with thickening, mesenteric fat stranding and air-fluid levels and the gastric pacemaker wires appeared wrapped around the small bowel mesentery (Fig. 1). She became acutely hypotensive and required fluid resuscitation and vasopressors. Patient underwent emergency laparotomy after initial fluid resuscitation. A long segment of the ileum was noted to be ischemic secondary to the gastric stimulator wires forming a 360-degree loop around the base of the mesentery (Fig. 2). Gangrenous bowel was resected starting from a point 150 cm distal to the ligament of Treitz all the way to her ileo-rectal anastomosis. A total of 140 cm long segment of distal small bowel was resected and the gastric stimulator was explanted. Patient’s small bowel was left in discontinuity. She was taken back to the OR 48 h later for a second look where the bowel looked healthy and a hand sewn anastomosis was performed between the small bowel and the rectal stump. Patient was left with a total length of 150 cm of small bowel that was connected to the rectum. Patient had an uneventful recovery and was discharged from the hospital. Over the next 2 years, patient went on to develop signs and symptoms of short gut syndrome that failed medical management. She is currently being worked up for a small bowel transplant.
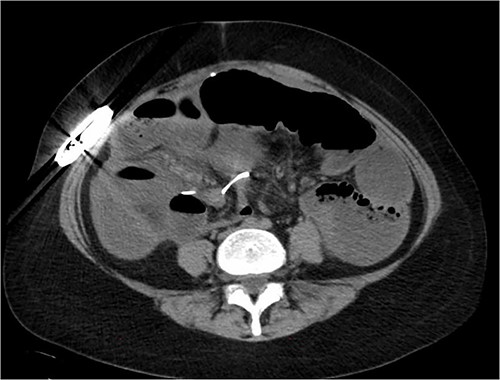
CT image showing dilated small bowel with gastric stimulator wire seen looping around one of the small bowel loops suggesting possible strangulation.
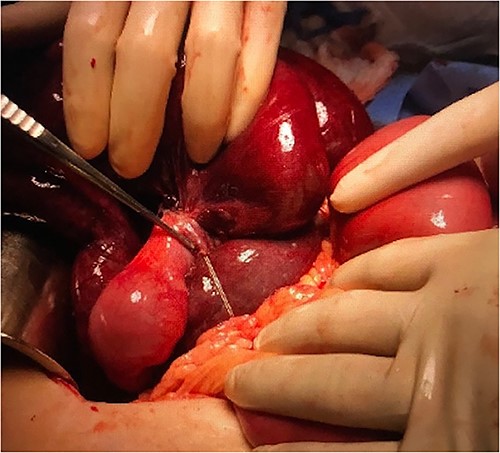
Gangrenous bowel with gastric pacemaker wire wrapped around the base of the mesentery.
DISCUSSION
In the literature, we found only one case report of a similar outcome in 2015 from Sweden by Lederhuber et al. [2], where a 59 years old female presented 8 years after gastric stimulator placement and was found to have bowel strangulation by gastric pacemaker wires. Interestingly, their patient had presented multiple times with abdominal pain, nausea and vomiting for 2 years prior to her presentation with bowel strangulation and was misdiagnosed as ileus and gastroparesis each time. In contrast, our patient did not have warning symptoms before this catastrophic event.
As per our knowledge, this is the second reported case of this particular complication. It is not possible to determine risk factors or causation based on just two cases but we hypothesize that there were two factors in our patient that increased her odds of getting this outcome. First, history of total colectomy that makes supra colic compartment easily accessible to the small bowel. We think that transverse colon and mesocolon act as a barrier between the pacemaker wires (supracolic) and small bowel (infracolic). A lack of this barrier would have allowed wires to form a loop around the small bowel mesentery more easily. Lack of colon also contributed to the development of short gut syndrome subsequently. Second, history of lupus and steroid use played a role in lack of scarring. In fact, in all the three procedures that our patient underwent, we found a complete absence of intraperitoneal adhesions and scarring around the battery and the wires in the subcutaneous pocket. We think a complete lack of scarring in the subcutaneous battery pocket allowed the excess wire to drop back inside the peritoneal cavity to provide sufficient redundant length to form a noose around the base of the mesentery.
Gastric stimulator is one of the options for management of refractory gastroparesis but as with any surgical intervention, it carries risk of complications. Small bowel strangulation secondary to pacemaker wires looping around the mesentery is one such rare but catastrophic complication. Risk of this complication should be discussed with patient while considering the gastric pacemaker insertion and this procedure is best avoided in patients with a history of total colectomy given higher risk of short gut syndrome in these patients. A high index of suspicions is very important in the management of this complication in a timely fashion.
CONFLICT OF INTEREST STATEMENT
None of the authors have any conflict of interest to report.
FUNDING
None.



