-
PDF
- Split View
-
Views
-
Cite
Cite
Jamil Suleiman, Mujaheed Suleman, Patrick Amsi, Peter Minja, Jay Lodhia, Giant pedunculated lipofibroma of the thigh, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad153, https://doi.org/10.1093/jscr/rjad153
Close - Share Icon Share
ABSTRACT
Pedunculated lipofibroma is a rare form of nevus lipomatous cutaneous superficialis. They are usually solitary lesions found around the thighs, buttocks and trunk; thought to have a predilection for pressure areas. There are two types of lipofibromas; sessile or pedunculated. They are mostly asymptomatic but can cause symptoms as they grow larger affecting daily activities. Treatment is not indicated in smaller lesions, except for cosmetic purposes. Herein we present this rare benign lesion with an unusually large size.
INTRODUCTION
Pedunculated lipofibroma, also known as a solitary form of Nevus lipomatosus cutaneous superficialis, is a relatively rare form of benign connective tissue proliferation that develops as a result of ectopic adipose tissue in the dermis [1]. Lipofibromas usually appear as large, solitary, slow growing, skin colored, compressible, pedunculated to dome shaped, nodules or plaques and occur on the buttocks, upper thighs and non-pelvic areas, such as the axillae, arms, knees, ears and scalp [1].
We report here on a case of a giant pedunculated lipofibroma of the thigh on an adult Tanzanian lady.
CASE PRESENTATION
A 43-year-old female presented to our surgical clinic with a 2-year history of inguinal swelling that progressively increased in size over time. The swelling was associated with excoriations on both sides that were in contact with her thighs on walking. Over time, the swelling grew large enough to hang from a stalk attached to her inguinal area with two ulcers on either side of the swelling with no discharge or pain. She visited several peripheral hospitals with no relief or cure and was then referred to our Institute for further management.
On examination, she was nutritionally well, not pale, with vitals within normal range and was saturating at 99% on room air. On local examination, there was a large pedunculated mass arising from the inguinal region ⁓4 cm from the right labia majora, measuring 30 × 20 cm, with regular margins, skin overlying the swelling had excoriation marks, and two ulcers on either side of the mass ⁓3 × 3 cm each with regular margins and granulating bases. The mass was firm and mobile from the stalk, with no tenderness on palpation (Fig. 1). Examination of other systems was essentially normal.
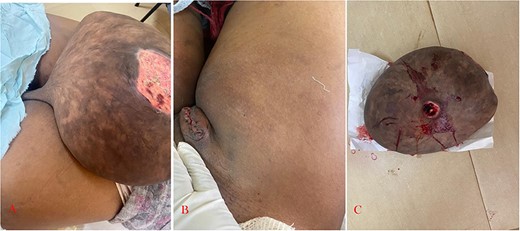
(A) Clinical photograph showing giant lipofibroma arising from the inguinal region with a stalk. (B) Post complete excision. (C) Resected (giant) lipofibroma.
Her laboratory findings revealed a normal leukocyte count of 8 × 109/L, a hemoglobin of 14 g/dl and a normal platelet count of 389 × 109/L. After counseling, the mass was resected whole with its stalk under local anesthesia and submitted for histopathology analysis (Fig. 1). Microscopically, the histological sections showed lobules of mass with fat tissue and adjacent skin ulceration. The mass formed predominantly by lobules of fat tissue was compressing the adjacent dermis. There were groups and strands of mature adipocytes comprising small eccentric nuclei with minimal atypia seen extending between collagen bundles of the dermal layer of the skin, features suggestive of lipofibroma (Fig. 2).
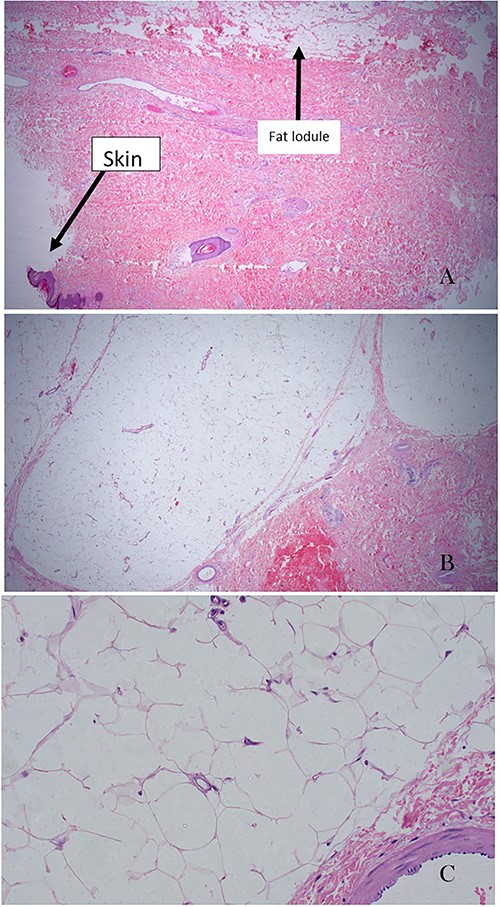
(A) Ulcerated skin and the lobules of mass with fat tissue (×20 magnification). It is also showing ulceration on the adjacent skin. (B) Lobules of fat tissue compressing the adjacent dermal collagenous tissue. There are groups and strands of mature adipocytes extending between collagen bundles of the dermal layer of the skin (×20 magnification). (C) High-power field of adipose tissue with mature adipocytes and without atypia. Adipocytes have small eccentric nuclei with minimal atypia in a perivascular space (×200 magnification).
She was then followed after 3 months in our outpatient clinic where the wound had healed well with no swelling in the excision area suggesting no recurrence.
DISCUSSION
Lipomas are the most common benign soft-tissue tumors and have many subtypes including lipofibroma, angiolipoma, myxoid lipoma, spindle cell lipoma, pleomorphic lipomas and intramuscular lipoma [2]. Lipofibroma is a rare benign hamartomatous condition first described by Hoffmann and Zurhelle in 1921. Clinically, there are two principal presentations; the classic form appears as a cluster group of soft, smooth papules or nodules, at birth and develops during the first three decades of life, most commonly seen on the pelvic girdle, with a predilection for the gluteal region. The second form comprises a solitary, domed, sessile papule, which usually develops in adult life, as described in the index case [3]. In 1975, Mehergan et al. proposed the term pedunculated lipofibroma for the latter given its distinctive clinicopathological features [4]. Pedunculated lipofibromas can clinically also be confused with other benign papilloma, including acrochordons, seborrheic keratoses, nevocellular nevi, verrucae, neurofibromas, fibroepithelioma of Pinkus and eccrine poroma, differentiated histologically as they are seen as isolated groups of ectopic mature adipocytes within the reticular dermis [1, 5]. Lipomas are termed giant when they exceed 10 cm in size, as in the index case, or 1000 g in weight [6].
The pathogenesis of pedunculated lipofibroma is unclear, although several theories have hypothesized that the deposition of adipose tissue in the dermis is due to degenerative changes in the dermal collagen and elastic tissue, displacement of subcutaneous adipose tissue into the dermis and origination and differentiation from the walls of dermal vessels [7].
While the etiology of lipomas is unclear, some studies have shown a genetic link, whereby about two-thirds of lipomas demonstrate genetic abnormalities. In addition to the possibility of a genetic link, another theory presents the idea that there is a direct positive correlation between trauma to an area of soft tissue and lipoma production [5]. In addition to the risk factors listed above, other possible connections that may lead to lipomas are obesity, alcohol abuse, liver disease, as well as glucose intolerance.
Pedunculated lipofibromas are not life-threatening but may occasionally ulcerate such as in the case reported, or cause other cosmetic or functional inconvenience to the patient and the giant ones may hamper activities of daily living [8, 9]. Surgical excision is the definitive management method for such types of lesions, and recurrence has not been reported. Cryotherapy and diode laser surgery have also been reported as alternative treatments for pedunculated lipofibromas [1, 10].
Lipofibromas are rare benign growths mostly seen over the upper thighs, buttocks and trunk. They are slow-growing lesions and can be confused with other benign papillomas hence diagnosis can be confirmed by histopathologic findings. The preferred treatment of lipofibroma is surgical excision and cryotherapy can be another viable option.
ACKNOWLEDGMENTS
The authors would like to thank the patient for permission to share her medical information to be used for educational purposes and publication.
CONFLICT OF INTEREST STATEMENT
The authors declare they have no competing interests.
FUNDING
No funding or grant support.
AUTHORS’ CONTRIBUTIONS
JS, MS and JL conceptualized and drafted the manuscript. PM reviewed the medical records and PA reviewed and reported the histology. All authors have read and approved the final script.
INFORMED CONSENT
Written informed consent was obtained from the patient for publication for this case report; additionally, accompanying images have been censored to ensure that the patient cannot be identified. A copy of the consent is available on record.
REFERENCES
Yadav U, Garg A, Devgan A, Sheoran A, Dutta M, Gupta A, et al.



