-
PDF
- Split View
-
Views
-
Cite
Cite
Ioannis Tilaveridis, Panagiotis Karakostas, Vasilios Tilaveridis, Stavros Tilaveridis, Displacement of maxillary third molar into the infratemporal fossa. A case report, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad141, https://doi.org/10.1093/jscr/rjad141
Close - Share Icon Share
Abstract
Our study aims to present a new case of maxillary third molar dislodgement into the infratemporal fossa during the effort of extraction and the surgical approach performed to retrieve the tooth. Guidelines to prevent this complication are presented. We describe a new case of maxillary third molar displacement into the infratemporal fossa following an unsuccessful surgical procedure of tooth removal by a general dentist. The location of the displaced tooth was confirmed with computed tomography (CT) scanning with a 3D reconstruction. The tooth was removed under general anesthesia through an intraoral approach. It took less than 10 min for the whole procedure to be accomplished. CT examination is of paramount importance to precisely locate the dislodged tooth. Removal can be successfully accomplished via an intraoral approach with meticulous manipulations. An incision of adequate length and a long Langebeck retractor are valuable to ensure a wide surgical field.
INTRODUCTION
Despite the advances achieved in dental science, complications during or after the third molar removal still occur. In some cases, however, more severe complications occur, which necessitate the contribution of a maxillofacial surgeon to treat. Root or tooth displacement into adjacent anatomic sites is a classic complication of third molar extraction. Root dislodgement is more common than dislodgement of the entire tooth [1, 2]. According to some authors, total dislodgement of the entire tooth into adjacent anatomical spaces is a very rare situation [3].
The anatomic sites where displaced mandibular third molars are most commonly found include the pterygomandibular, the parapharyngeal, the buccal area and the submandibular space [4–6]. The anatomic spaces involved in maxillary third molar displacement include the infratemporal and pterygopalatine fossa and the maxillary sinus. There are only a few published cases of maxillary third molar dislodgement into the infratemporal fossa during extraction in the English literature [1, 2, 7, 8].
Our study aims to present a new case of dislodgement of the entire maxillary third molar into the infratemporal fossa and to provide guidelines to prevent and treat this serious complication.
CASE REPORT
A 17-year- old male patient in good general health was referred to our Department of Oral and Maxillofacial Surgery, General Hospital Papanikolaou, Thessaloniki, Greece, with slight left facial swelling and discomfort. Patient history revealed that he had his third molars removed by a general dentist. Mandibular third molars and right maxillary third molar were removed uneventfully (Fig. 1). However, during the extraction of the left maxillary molar, the tooth disappeared from the surgical field and the attempts of the dentist to find and remove the displaced tooth remained unsuccessful.

Orthopantomograph showing the location of third molars before their removal. The left maxillary third molar was displaced into the ipsilateral infratemoral fossa.
Clinical examination revealed a slight swelling of the face without signs of local infection and without restriction in mouth opening. The displaced tooth was not palpable at the soft tissue-affected area. The radiographic was examined by use of computed tomography (CT) scan with 3D reformation. CT examination demonstrated the presence of the tooth into the ipsilateral infratemporal fossa with its lowest level of masticatory surface of the crown being at the inferior border of malar bone adjacent to the coronoid process (Fig. 2a and b). A prompt surgical removal of the dislodged tooth was recommended to the patient to avoid possible post-extraction infection.
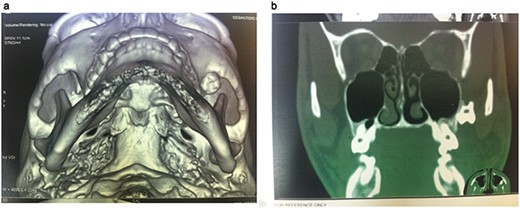
CT 3D reconstruction showing the exact location of the displaced molar into the infratemporal fossa behind the zygoma.
The patient was operated under general anesthesia for better comfort both for the patient and for the surgeon. After local anesthesia with vasoconstriction (lidocaine with adrenaline 1:100 000), an incision was made along the upper buccomaxillary sulcus (Fig. 3). With careful blunt tissue dissection, the crown of the tooth was revealed. With meticulous manipulations to avoid upward displacement of third molar, the tooth was grasped firmly with long Adson forceps and removed (Fig. 4). After copious irrigation of the surgical field, the wound was closed with interrupted resorbable sutures. Pre-operative CT imaging was proved valuable for finding the precise location of the displaced tooth during the operation and avoiding more cumbersome approaches. The surgical procedure lasted about 10 min.

Photograph showing the intraoral approach to the infratemporal fossa through a long incision into the bycco-gingival sulcus.

Photograph showing removal of the tooth with the aid of long Langebeck retractors.
The post-operative course was uneventful and the patient remained free of symptoms one year after the operation.
DISCUSSION
Complications in the third molar surgery include hemorrhage, post-operative infection, adjacent nerve injuries, osteitis or trismus [9, 10]. The incidence of complications related to the third molar surgery is moderate, about 10%. The rate of complications increases when removal is attempted by general dentists rather than by experienced maxillofacial surgeons [2].
Maxillary molars are most commonly dislodged to infratemporal fossa, due to rupture of periosteum during flap elevation and inappropriate use of elevators along with a lack of preventive measures to avoid this complication. In the reported cases, the displaced teeth were found in the soft tissue of the infratemporal fossa, below the inferior border of the lateral pterygoid muscle and near the external pterygoid plate [1, 2, 7, 8].
Orthopantomograph is usually only useful to confirm the presence of the tooth in an unnatural position. Conventional CT or cone beam CT are both extremely valuable to the surgeon to precisely locate the position of the dislodged tooth three-dimensionally [7, 9].
Maxillary third molars are usually displaced into the infratemporal fossa, although a case of maxillary third molar displacement into the pterygopalatine fossa has also been reported [10]. However, an unusual case of paradoxal dislodgement of a mandibular third molar into the infratemporal space has also been described [5].
Different surgical approaches have been proposed to retrieve the displaced, maxillary third molar. Some surgeons used extraoral hemicoronal approaches to remove the displaced tooth from infratemporal space [1], but most authors prefer intraoral approaches, as being more conservative and related to less morbidity [2, 10]. Transantral approach and resection of the coronoid process have also been proposed [8]. In our case, the displaced tooth was removed in a very short time based only on pre-operative CT imaging.
We recommend an intraoral approach through an incision made in the upper buccal sulcus. This incision is very close to the displaced tooth. However, during tissue dissection, care should be taken to avoid any excessive upwards forces to avoid further displacement of the tooth. During the dissection, a long Langenbeck retractor is of outmost importance to assure a wide surgical field and avoid coronoidectomy.
Preventive measures should be taken during the extraction of deeply impacted maxillary molars to avoid these serious complications. A critical preventive measure to avoid maxillary third molar displacement to adjacent maxillofacial spaces is the use of a long Langebeck retractor during the extraction. The end of this instrument should be inserted above the impacted molar. Adequate reflection and elevation of a broad mucoperiosteal flap is a prerequisite to place the retractor correctly. This manipulation is strongly recommended since dislodgement of the tooth into the infratemporal fossa is blocked by the end of the retractor.
CONCLUSION
To conclude, an adequate incision to ensure a wide surgical exposure and appropriate use of recommended instruments are the keys to successful removal of a displaced maxillary third molar. The surgical procedure should be performed as soon as possible to avoid serious and potential fatal complications.
Authors declare that the forthcoming manuscript is in compliance with the guideline CARE for case reports.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



