-
PDF
- Split View
-
Views
-
Cite
Cite
Se In Park, Jae Won Lee, Joo Ho Zhiang, Yeon Seung Chung, Moon Jae Chung, Sung Hyun Kim, Mixed neuroendocrine-non-neuroendocrine carcinoma (MiNEN) in gallbladder with liver metastasis of neuroendocrine carcinoma component: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad132, https://doi.org/10.1093/jscr/rjad132
Close - Share Icon Share
Abstract
Mixed neuroendocrine-non-neuroendocrine neoplasms of the gallbladder are rare with a lack of established standardized therapeutic strategies. We report a case of gallbladder mixed neuroendocrine-non-neuroendocrine neoplasm with liver metastasis of neuroendocrine carcinoma. A patient who underwent radical cholecystectomy for gallbladder adenocarcinoma was detected with increasing liver mass, and hepatectomy was performed. Pathological report revealed neuroendocrine carcinoma. To find primary origin, pathological review of the old specimen from previous cholecystectomy with a slightly different perspective was conducted, where the neuroendocrine component was positively dyed. In conclusion, though it might be impossible to review every pathological result in cases with ambiguous findings, reviewing the previous specimen can be a useful option in diagnosis.
INTRODUCTION
Neuroendocrine tumor (NET) of the gallbladder (GB) is rare, accounting for ~2% GB cancers. GB is also a rare location for primary NET, known for 0.5% of all NETs according to the Surveillance Epidemiology and End Results registry [1]. Furthermore, mixed neuroendocrine-non-neuroendocrine tumor (MiNEN) is a rarer type than NET in GB, consisting of two histologic components, a neuroendocrine and non-neuroendocrine components.
Primary NET in the liver is even rarer, with <200 cases reported since the first report in 1958. It is currently known to account for 0.3% of all NET cases [2]. Primary hepatic NET is rarely diagnosed owing to its rare nature. Once NET is detected in the liver, it is usually considered a result of metastatic tumor, and thorough work-up is usually performed to locate the origin of the NET. It is reported that of all the NETs found in the liver, >80% were results of metastasis, emphasizing the importance of diagnostic work-up to find the origin site [3].
In this paper, we present a case of a patient who was diagnosed pathologically with a NET of the liver after undergoing surgery. In search of the origin site, pathologic review of the previously removed GB that was diagnosed with GB adenocarcinoma was performed, and pathologic diagnosis was revised as MiNEN.
CASE PRESENTATION
A 51-year-old woman presenting with epigastric and substernal pain, with a 3 cm-sized GB polyp found using an ultrasonic exam, was referred to the outpatient department for further evaluation. Enhanced computed tomography (CT) showed 3.5 cm sized enhancing villous mass in the GB with two tiny attenuating lesions in segment V and segment VI of the liver that were too small to characterize. To obtain more information about the tumor, outpatient follow-up of tumor markers and further imaging studies were conducted. Tumor markers were within normal range for CEA: 1.15 ng/ml (reference: 0–5 ng/ml) and CA 19–9 of 13.1 ng/ml (reference: 0–34 ng/ml).
For further information, magnetic resonance imaging (MRI) and positron emission tomography (PET)-CT scan were performed, and MRI also revealed a 3.5 cm sized enhancing villous mass in GB body, suggesting GB cancer (Fig. 1A). Two tiny low attenuating lesions in segment V and VI of the liver were likely to be cysts, suggesting non-malignancy. PET-CT revealed increased fludeoxyglucose (FDG) uptake in the GB body mass, which was suspected to be malignant, and discernible FDG uptake was not found in the liver.
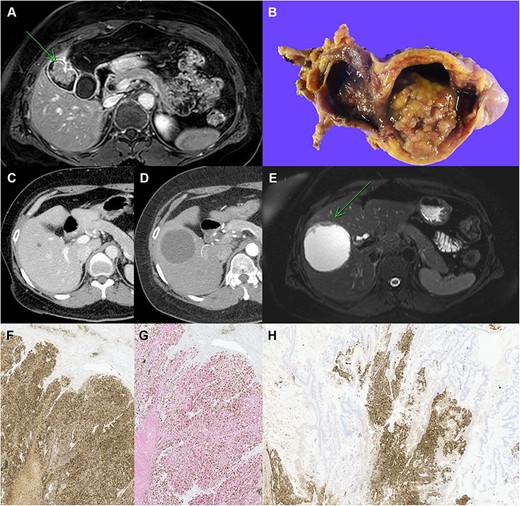
Clinicopathological images of the patient. (A) Preoperative MRI showing GB cancer, (B) gross specimen of GB with papillary tumor, (C, D) follow-up imaging showing the increased size of cystic lesion in the liver, (E) MRI showing cystic mass in segment V with enhancing mural nodule and wall thickening, (F) immunohistochemical staining with chromogranin A, (G) synaptophysin (red) and Ki-67 (brown) double staining in neuroendocrine carcinoma of the liver, (H) chromogranin A staining in the GB tumor, which reveals neuroendocrine component (original magnification: ×100).
Based on her imaging findings, laparoscopic radical cholecystectomy was planned under the impression of GB cancer. The specimen showed a 4-cm-sized papillary mass and pathologic examination confirmed well-differentiated adenocarcinoma without lymph node metastasis (T2aN0M0, Stage IIA) (Fig. 1B).
After the surgery, the patient received adjuvant gemcitabine chemotherapy and was followed-up in outpatient settings. A series of follow-up CT showed a growing cyst in the S5 liver segment (Fig. 1C and D). Therefore, MRI was performed for differential diagnosis, which showed a growing 7-cm-sized cystic mass with enhanced mural nodule and wall thickening (Fig. 1E). Right lobectomy of the liver was planned for the possibility of malignancy.
After the surgery, pathological findings of the specimen revealed neuroendocrine carcinoma (NEC) sized 8 cm. The tumor contained extensive necrosis, with mitotic index 2/10 HPF and focal glandular differentiation of < 5% (Fig. 1F). The Ki-67 index was about 70%, and the subtype of the NEC was large cell NEC (LCNEC) (Fig. 1G).
The most likely diagnosis was metastatic tumor of the liver, and thus thorough diagnostic work-up for primary tumor site was performed. Ga-68 DOTATOC PET-CT was performed; however, the site of primary origin could not be located. In extension of finding the origin of the NET, a review of the previously resected GB specimen was conducted. The review found a neuroendocrine component in the specimen, which was previously unseen. The neuroendocrine component was positive for chromogranin A, synaptophysin and CD56 in immunohistochemical staining, and the specimen was rediagnosed as MiNEN consisting of adenocarcinoma and LCNEC (Fig. 1H).
Finally, the liver NEC was identified as metastasis from the neuroendocrine component of GB MiNEN. After the second operation, the regimen was changed to etoposide plus cisplatin. The patient is currently undergoing regular follow-up after chemotherapy. There was no evidence of recurrence for 24 months from radical cholecystectomy.
DISCUSSION
The most common metastasis site of NET is the liver accounting for 82% of all patients with metastasis. In patients with liver metastasis, the primary sites are as follows: small intestine accounting for 56%, colon with 10% and liver/GB/pancreas with 10% [4]. According to Pengyan et al., 41 patients with GB MiNEN were reported; of these, 17 patients had liver metastasis [5]. To our knowledge, this is the first case of liver metastasis of GB MiNEN reported in Korea.
Since primary liver NET is rare, several diagnostic work-ups were carried out in search of the origin of the NET in the current patient. However, a possible origin was not found in the search. Pathology review of the old specimen from previous surgery, with a slightly different perspective, was carried out to search for every possibility that was possibly missed out. Previously, the patient was diagnosed immediately with the pathologic findings of adenocarcinoma. However, immunohistochemistry was performed in consideration of the possibility of containing neuroendocrine components, and thus the pathological report of the specimen was revised. In conclusion, though it might not be possible to review every pathological result in patients with ambiguous findings, it can be emphasized that reviewing the previous specimen could be a useful option in diagnosis.
Since MiNEN of the GB is rare, not much is known about its treatment after the radical surgery. According to recent knowledge, oxaliplatin plus gemcitabine combination is the chemotherapy regimen currently known to be most effective for GB adenocarcinoma. However, it showed poor response against NET of the GB. In contrast, etoposide, cisplatin and adriamycin were found to be effective against this tumor [6]. In the present case, the patient was administered adjuvant chemotherapy with gemcitabine, but after the pathologic review was done and diagnosis was revised as GB MiNEN, chemotherapy regimen was changed to cisplatin. As this type of tumor is rare and not much is known, more studies on GB MiNEN and its metastasis to the liver are required.
When GB MiNEN was accompanied by liver metastasis, it was reported that the outcome was worse. According to Pengyan Wang et al., liver metastasis is a poor prognostic factor for overall survival [5]. In case of general NET, the 5-year survival rate was 75–99% without metastasis, whereas in the case of metastasis, it was 40% [7]. If more cases are reported in the future, more accurate learning about the relationship between liver metastasis and prognosis of GB MiNEN will be possible.
In addition, it has been reported that the liver metastasis component of GB MiNEN is mainly a neuroendocrine component [5]. In this case as well, the metastasized component was the neuroendocrine component. It was consistent with previous studies that the neuroendocrine component of GB MiNEN shows a more aggressive pattern than non-neuroendocrine component [8, 9]. It is not yet known how the prognosis varies depending on whether the liver metastasis component of GB MiNEN is a neuroendocrine component or a non-neuroendocrine component. Further discussion on this is required in the future.
In conclusion, primary NET in the liver is so rare that physicians should keep in mind the possibility of metastasis when they experience NET of the liver in patients. Moreover, physicians should review previous pathologies for accurate diagnosis, if necessary.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The data are available from the corresponding author upon reasonable request.



