-
PDF
- Split View
-
Views
-
Cite
Cite
Vito Pende, Giulia Fiori, Giorgio Lucandri, Flaminia Genualdo, Sara Lucchese, Francesco Falbo, Andrea Biancucci, Paolo Mazzocchi, Massimo Farina, Emanuele Santoro, Management of low colorectal anastomotic leakage using negative pressure therapy with Transanal Minimally Invasive Surgery (TAMIS): description of a case and review of the literature, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad124, https://doi.org/10.1093/jscr/rjad124
Close - Share Icon Share
Abstract
Anastomotic leakage (AL) represents a major post-operative complication after low anterior resection (LAR) for rectal cancer. It is associated with increased morbidity, mortality, length of hospital stay and risk of permanent stoma. Herein we report the case of a 75-year-old male patient submitted to a minimally invasive LAR who developed an AL on the fifth post-operative day. This complication has been successfully managed by placing a Vacuum-Assisted Therapy device (Endo-SPONGE®) with an unusual Transanal Minimally Invasive Surgery (TAMIS) approach; the size of the abscess cavity was measured and the Endo-SPONGE® was cut according to the size of the fistulous defect. This procedure has been performed at regular intervals, achieving quick reduction of anastomotic defect. After the discharge from our department, the patient was addressed to adjuvant treatment. TAMIS may represent an alternative to the endoscopic approach to position an Endo-SPONGE® whenever a conservative management of an AL is required.
INTRODUCTION
Anastomotic leakage (AL) represents a major post-operative complication after low anterior resection (LAR) for rectal cancer [1], with an incidence ranging from 2 to 20% [1–3]. AL is linked to increased morbidity, mortality, length of hospital stay and risk of sepsis, and it may cause significant delay in starting post-operative adjuvant treatment. Even though several risk factors have been associated with increased risk of AL (such as overweight, neoadjuvant treatment, location of the tumor, bad tissue perfusion), this complication is still considered an unpredictable event, with significant human and economic consequences [3, 4]. The management of AL can be conservative or operative depending on different factors, including the following: extension of anastomotic defect and perianastomotic cavity, presence of defunctioning ileostomy, distance of anastomosis from the anal verge and the patient’s clinical status; according to the International Study Group of Rectal Cancer Classification (ISREC), AL can be categorised as grade A (requiring only medical treatment), B (requiring endoscopic/interventional radiology) or C (requiring laparotomy/laparoscopic surgery) [5, 6]. Herein we report the case of a patient submitted to LAR for rectal cancer, who developed AL on the fifth post-operative day; the leakage has been successfully managed by positioning an advanced medication with a Vacuum-Assisted Therapy (Endo-SPONGE®), using an unusual Transanal Minimally Invasive Surgery (TAMIS) approach.
CASE PRESENTATION
A 75-year-old Caucasian man was referred to our department on May 2022 because of a positive fecal occult blood test; subsequent colonoscopy showed an endoluminal substenosing lesion, located at sigmoid-rectal junction and extended distally for 5 cm. The tumoral bulk appeared centrally ulcerated and occupied more than three-fourth of the rectal circumference. The panel of biopsies resulted positive for well-differentiated adenocarcinoma. An angio-CT scan confirmed the presence of a sigmoid-rectal wall thickening, extended distally for about 6 cm, with significative narrowing of colonic lumen. Lateral spread appeared limited to the muscolaris propria, whereas the mesorectal component was unaffected; the presence of T2 lesion at preoperative diagnostic work-up was confirmed by MRI while neither hepatic nor pulmonary metastasis were detected. Tumor markers were within normal range. At physical examination, the patient appeared overweight (BMI 30.5), with no other significative comorbidity. Pre-operative staging led the Multidisciplinary Tumor Board to authorise a surgical approach. The patient underwent laparoscopic low anterior rectal resection with total mesorectal excision, with transanal end-to-end stapled colorectal anastomosis (7 cm from the anal verge) and ileostomy. Histological report of resected specimen confirmed the diagnosis of a G2 rectal adenocarcinoma, staged as pT3 pN1a R0, whereas the quality of mesorectal excision was graded as 3 (complete mesorectal fascia) according to Quirke classification. On the fifth post-operative day, the patient developed an increase in body temperature (37.8°C), in WBC count (10 × 103/uL) and in CRP plasmatic levels (6.63 mg/dL), as well as a corpuscular discharge from perianastomotic drainage; at physical examination, the patient showed a moderate tenderness on lower left abdomen with no clear signs of peritonitis. Early abdominal angio-CT scan showed a 15-mm discontinuity on the posterior wall of colorectal anastomosis, with perirectal fluid and extraluminal gas collection (Fig. 1). Low-flow endoscopic exploration confirmed the anastomotic wall defect in the right postero-lateral side, connected to a cavity filled with necrotic tissue (Fig. 2). Given the presence of ileostomy and perianastomotic surgical drainage and the absence of peritonitis signs with proper control of patient’s hemodinamics, we opted for a non-surgical treatment. On the sixth post-operative day, the patient underwent an Endo-SPONGE® device placement into the AL cavity, performed with TAMIS approach [7]. With the patient in lithotomy position, a GelPOINT® path transanal access platform was positioned; laparoscopic insufflation pressure was set at 10 mmHg. The right posterolateral anastomotic wall defect was visualised (Fig. 3), then the AL cavity was carefully measured (3 cm × 4 cm), washed with saline solution and explored up to the tip of surgical drainage. The polyurethane sponge was positioned under laparoscopic vision and then connected to the vacuum suction system, set at −40 mmHg. The Endo-SPONGE® device was replaced every 72 h for 2 weeks, then every 96 h for another 10 days; size and shape of the device were modified and gradually reduced according to the decreasing size of the cavity. Control CT scan and rectosigmoidoscopy confirmed the almost complete obliteration of the AL cavity. The Endo-SPONGE® device and the abdominal drainage were removed on the 25th post-operative day and the patient was then discharged without further complications. The patient has been addressed to adjuvant treatment protocol; a 3-month control CT scan showed neither distant metastases nor residual perirectal cavity. Once adjuvant treatment is completed, patient will be enrolled for colorectal anastomotic check and closure of ileostomy.
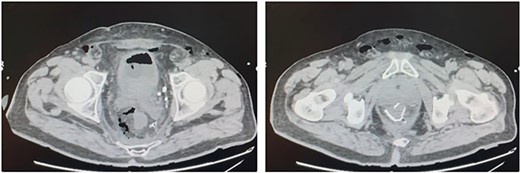
Contrast CT scan: ‘Abundant fluid-air presence in the presacral space and in the mesorectum at the level of the colo-rectal anastomosis, and a discontinuity on the posterior side of the colonic wall’.
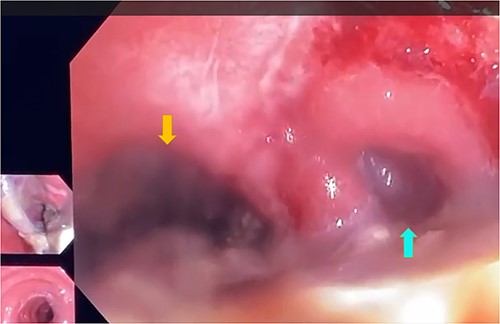
Low-flow endoscopic exploration which confirmed the presence of dehiscence of the colorectal anastomosis in the right postero-lateral colonic wall, 7 cm from the anal verge, giving access to a large cavity filled with fibrin and necrotic tissue (yellow arrow), colic lumen (blue arrow).
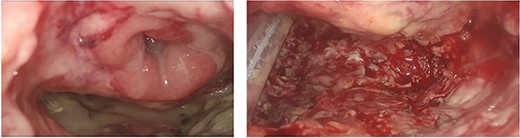
The visualisation of the right posterolateral dehiscence, the adjacent cavity (measuring 4 cm × 3 cm) with drainage by TAMIS approach.
DISCUSSION
A non-surgical approach in treating an early detected AL may be planned in case of a grade A or B ISREC AL, despite the diameter of the lesion [8, 9]. Angio-CT scan provides important informations about the blood supply of the colon and allows measurement of AL cavity, enhancing its fluid and/or gas content. Low insufflation pressure endoscopy allows direct view of the anastomotic defect and debridement of necrotic tissues, creating the optimal condition for placing a tailored sponge device [10, 11]. Endo-SPONGE® suction device gradually provides healing of parietal defect and its contiguous AL cavity [12]. Endo-SPONGE® is usually positioned by endoscopic approach; following our experience with TAMIS in treating benign and malignant endorectal tumors, we extended TAMIS application to the management of Grade B colo-rectal AL cavity. Few similar experiences are reported in current literature [13, 14]. After adequate training, TAMIS appears technically simple, allowing an optimal view of the defect and a magnified vision during surgical performance, together with a very quick patient recovery. We particularly recommend such approach in patients requiring a prompt discharge in order to start oncological adjuvant treatment. In addition to that, TAMIS approach is a valid alternative in those hospitals where endoscopic assistance is not guaranteed by a 24-h service. In conclusion, we strongly support Endo-SPONGE® suction device placed via TAMIS for treating selected patients with Grade B AL.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- surgical procedures, minimally invasive
- postoperative complications
- endoscopy
- abscess
- immunologic adjuvants
- pharmaceutical adjuvants
- length of stay
- stomas
- morbidity
- mortality
- rectal carcinoma
- low anterior resection of rectum
- medical devices
- conservative treatment
- negative pressure
- transanal minimally invasive surgery



