-
PDF
- Split View
-
Views
-
Cite
Cite
Tegan J Kay, Peter J Gallagher, A case of acute pancreatitis and enterocutaneous fistula formation following extended right hemicolectomy, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad122, https://doi.org/10.1093/jscr/rjad122
Close - Share Icon Share
Abstract
Acute pancreatitis (AP) is a rare complication in the post-operative period and the incidence following colorectal surgery is unknown. Although benign hyperamylasaemia following colonic resection is a documented phenomenon, clinically significant AP in the post-operative setting is poorly described in the literature and little is understood about the underlying pathophysiology. Additionally, while gastrointestinal fistulae are a well-recognized complication of bowel surgery, nil previous reports discuss the possible contribution of post-operative AP to their development. We present a case of AP complicated by enterocutaneous fistula following extended right hemicolectomy and describe the possible mechanisms leading to these conditions.
INTRODUCTION
Acute pancreatitis (AP) is an infrequent complication following abdominal surgery [1]. Although benign hyperamylasaemia following colonic resection is a documented phenomenon [2], clinically significant AP in the post-operative setting is poorly reported and the incidence is unknown. While gastrointestinal fistulae are a well-recognized complication of bowel surgery, nil previous reports discuss the possible contribution of post-operative AP to their development. We present a case of AP complicated by enterocutaneous fistula (ECF) following extended right hemicolectomy.
CASE REPORT
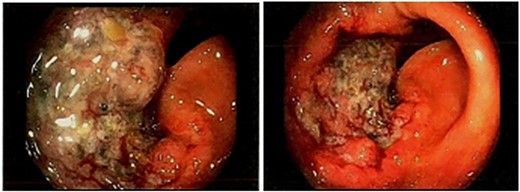
An 89-year-old male underwent an elective right hemicolectomy for transverse colon T3N0MX adenocarcinoma, diagnosed following colonoscopy (Fig. 1). Intraoperative findings revealed a distal synchronous mass in the transverse colon, and a classical extended right hemicolectomy was performed without the need for retroperitoneal mobilization.
The post-operative course was initially uncomplicated, however, the patient developed new onset atrial fibrillation and fever on Day 3. A computed tomography (CT) of abdomen/pelvis demonstrated post-operative ileus without evidence of infection. Total parenteral nutrition was commenced. Due to worsening upper abdominal pain and failure to clinically progress, additional biochemical testing on Day 8 revealed a lipase of 3363 units/litre. A repeat CT of the abdomen/pelvis demonstrated mild peripancreatic fluid without evidence of necrosis along with persistent post-operative ileus (Fig. 2). An ultrasound (US) revealed cholelithiasis with evidence of cholecystitis or choledocholithiasis. Conservative management of AP with analgesia, fluids and electrolytes was initiated.
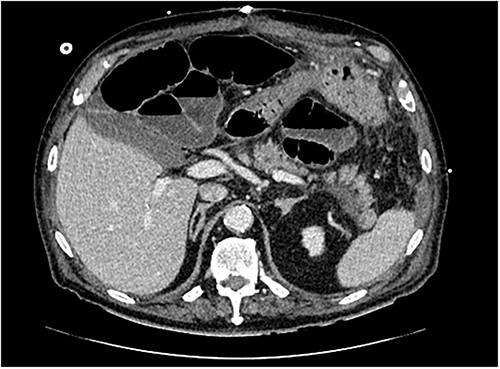
Transverse section of CT abdomen/pelvis performed on post-operative day 8, illustrating peripancreatic fluid and post-operative ileus.
On Day 13, an ECF through the laparotomy wound was noted. Due to the emergence of sepsis with high volume output, the patient returned to theatre on Day 16. At laparotomy, the small bowel was oedematous, fragile and densely adherent to the anterior abdominal wall with adhesions. There was extensive retroperitoneal fat necrosis. The ileocolic anastomosis was intact, however, there was enteric fluid from an ill-defined leak from the distal small bowel. Due to friability of the bowel, the decision was made to create an end ileostomy with mucous fistula (Abcarian fistula). Two large bore drains were placed along the pancreatic bed. Post-operatively, sepsis improved with the ECF controlled. Unfortunately, the patient’s admission was prolonged with refractory high stoma output despite codeine, loperamide and octreotide. He remained in hospital with plans for stoma reversal, however, developed central line-related sepsis and died 12 weeks following the initial operation.
DISCUSSION
AP is rare in the post-operative period [1]. Although a well-recognized complication of biliary and pancreatic surgery [3], it may also occur following anatomically remote operations such as cardiac [4], gynaecologic [5] and spinal surgery [6]. The specific incidence of AP following bowel resection is unknown, however, with an incidence as high as 1.8% following abdomino-vascular surgery [7], cases are likely under-recognized. Given post-operative AP is associated with prolonged parenteral nutrition and possibly longer hospitalization [7], clinicians should be aware of this complication following colorectal surgery so that early management can be initiated.
Due to the rarity of post-operative AP following bowel resection, the underlying pathophysiology can only be hypothesized. Benign hyperamylasaemia is known to occur in 18.7% of patients undergoing elective colorectal surgery [2]. However, few develop clinical pancreatitis and there is no significant difference in the operative course between those with mildly elevated versus normal amylase levels [2]. For those patients who develop clinically significant AP, several possible mechanisms have been proposed. Rarely, iatrogenic pancreatic injury may occur, particularly if there is retroperitoneal bleeding or a bulky splenic flexure tumour [8]. Pressure on the pancreas from extended retraction may also cause direct injury [9]. Griffith et al. found hyperamylasaemia to be associated with extended right hemicolectomies, particularly when the right and middle colic arteries were ligated [2]. They postulated this to be secondary to temporary occlusion of the main pancreatic duct or pancreatic trauma when placing traction on the root of the transverse mesocolon, thereby increasing risk of AP [2]. Indirectly, intraoperative hypoperfusion may lead to ischaemic damage and inflammation of the pancreas [10]. Anaesthetic medications must also be considered, with a recent study showing an association between the use of propofol and post-operative AP [11].
In this case, the patient developed atypical upper abdominal pain a week following surgery with a lipase of 3363 units/litre, which is a diagnostic for AP as per the revised Atlanta Classification [12]. Abdominal US demonstrated cholelithiasis, however, his bilirubin and liver function were normal, making choledocholithiasis an unlikely aetiology. Nil other established risk factors for AP were identified. Given the extended right hemicolectomy involved ligation of the both the right and middle colic vessels as well as mobilization of the splenic flexure, this likely contributed to the development of AP as per the mechanism described above by Griffith et al. [2] Although rare, post-operative AP is likely under-recognized, given colorectal surgery frequently involves these surgical techniques. Patients who develop atypical pain or failure to progress in the post-operative period should be investigated for AP, particularly following extended right hemicolectomy.
While ECFs are a recognized complication of colorectal surgery with an incidence of 4.3% [13], we postulate that the development of post-operative AP in this patient has a significant contribution to ECF formation. Although the relationship between post-operative AP and ECF has not previously been described, colonic fistulas are a well-documented complication of necrotising pancreatitis [14, 15]. Aldridge et al. hypothesize that the formation of colonic fistulas in this setting are secondary to the release of pancreatic enzymes into the peritoneal space via the transverse mesocolon and small bowel mesentery, resulting in fistulisation of the bowel wall [15]. Our intraoperative findings of extremely fragile bowel with evidence of retroperitoneal necrosis support this theory and highlights a similar mechanism likely contributes to ECF development following post-operative AP. As well as increasing the risk of ECF formation, post-operative AP likely results in technically challenging surgical intervention due to the detrimental effect of pancreatic enzymes on bowel wall fragility.
CONCLUSION
AP is likely an under-recognized complication following bowel resection. Post-operative AP should be suspected in patients with atypical abdominal pain or failure to progress so that expedient investigation and management may be initiated. AP in this setting likely contributes to the development of ECF and may make surgical intervention technically challenging.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The data that support the findings of this study are available on request from the corresponding author.



