-
PDF
- Split View
-
Views
-
Cite
Cite
Dylan S Tully, Janaka Balasooriya, James Lim, Rare dual surgical pathology at emergency laparotomy: a case report of concurrent small bowel obstruction and appendicitis, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad110, https://doi.org/10.1093/jscr/rjad110
Close - Share Icon Share
Abstract
Dual surgical pathology at emergency laparotomy is an uncommon finding outside of trauma scenarios. There is a scarcity of case reports of concomitant small bowel obstruction and appendicitis at laparotomy, likely in part because of advancements in investigative tools, diagnostic processes and the ready availability of medical care, which is demonstrated by harrowing statistics from developing nations where these factors are lacking. However, despite these advancements, initial diagnosis of dual pathology can be difficult. We report a case of concurrent small bowel obstruction and occult appendicitis discovered at emergency laparotomy in a previously well female with a virgin abdomen.
INTRODUCTION
A finding of dual surgical pathology at emergency laparotomy is rare. Small bowel obstruction is a common finding at laparotomy; however, laparotomy for appendicitis is performed in only 1.8% of presentations of appendicitis in western societies [1]. A finding of the two pathologies at emergency laparotomy occurs infrequently.
CASE REPORT
A 58-year-old female with a virgin abdomen reported 2 weeks of intermittent but persistent generalised abdominal pain with associated non-bloody diarrhoea, lethargy, nausea and anorexia without vomiting. It began as lower abdominal pain but this component had resolved. Diarrhoea and flatus ceased 1 day prior to presentation.
She presented as a transfer from a peripheral hospital tachycardic, hypotensive and tachypnoeic. Her abdomen was distended, diffusely tender with maximal tenderness in the left upper quadrant. Bloods showed white cell count of 39.2 × 10^9/L, C-reactive protein 307 mg/L and Lactate 2.8 mmol/L.
A non-contrast computed tomography scan (CT) of the abdomen and pelvis (contrast shortage) demonstrated a small bowel obstruction with bowel wall thickening in the ileum and associated free fluid, and transition point within the left lower quadrant. Retrospectively it appears the CT demonstrates the adhesion of both the sigmoid colon and transverse colon to a structure in the right iliac fossa (Fig. 1).
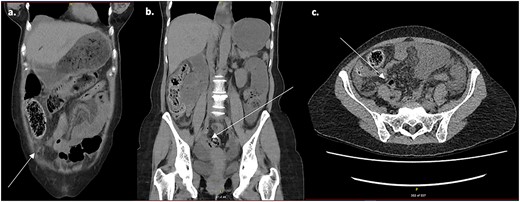
Non-contrast CT scan of the abdomen and pelvis. (a) Axial slice demonstrating transverse colon adhered to structure in right iliac fossa. (b, c) Coronal and axial slices demonstrating sigmoid colon adhered to structure in right iliac fossa.
She underwent emergency laparotomy, finding a closed loop small bowel obstruction involving 50 cm of proximal small bowel because of an omental adhesion between transverse colon and sigmoid colon (Fig. 2). The bowel was viable.
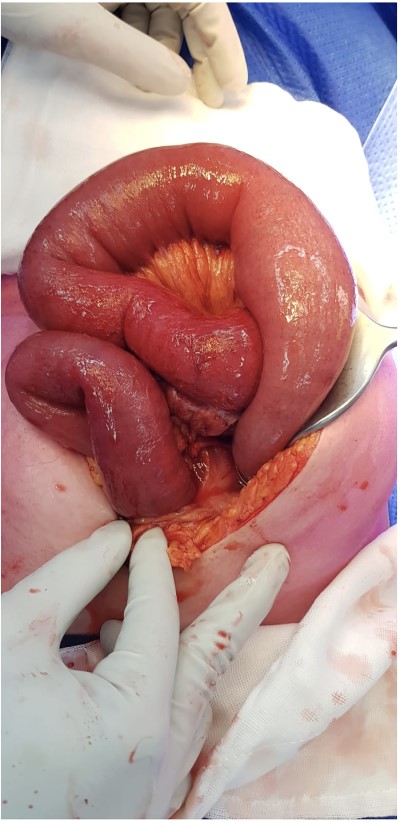
Approximately 50 cm of proximal small bowel involved in closed loop obstruction.
During the final wash an occult appendicular abscess was identified, leaving the appendix obliterated, difficult to identify (Fig. 3) and adhered to the anterior surface of the caecum. The transverse colon was adhered to the abscess. The abscess was drained, the appendix removed piecewise and the base oversewed.

Obliterated appendix with abscess contained pericaecally, after being dissected free.
The pathology demonstrated appendicitis. The patient recovered and was discharged Day 11 post-procedure with no major complications.
DISCUSSION
Outside of trauma scenarios, dual pathology at laparotomy is rare and the most often identified dual pathology reported is finding of a Meckel’s Diverticulum during operations for appendicitis or other [2].
Small bowel obstruction is a common finding, being present in half of laparotomies [3]. Although concurrent finding of sepsis is 15%, a portion of which are appendicitis [3], laparotomy finding of appendicitis is uncommon in western society, partly because of improved imaging and clinical diagnostic tools and easier access to medical care [4]. Studies from Nepal and Iraq demonstrate rates of approximately 50% for finding of appendicitis at emergency laparotomy [4, 5]. Protracted disease course because of delay in presentation, non-medical advice, misdiagnosis and mistreatment because of a lack of expertise or investigative equipment contributes to this phenomenon in developing countries [6].
Likewise, complications of appendicitis, such as appendicular abscess, are more common in such environments. In Pakistan, delayed operative management leads to complication rates of 33%, including appendicular abscess in 2–5% [7]. Abscess formation can then lead to further complications because of adhesions.
Case reports of dual surgical pathologies at laparotomy are scarce [8], and only 45 case reports exist between 1950 and 2016 of concomitant intestinal obstruction and appendicitis [9]. The most common proposed mechanism is mechanical obstruction because of interaction of the inflamed appendix with adjacent structures. The more common aetiology within this group is of an appendiceal tourniquet whereby the appendix wraps around bowel and causes an obstruction [10].
Discrepancy of CT findings with surgical findings is 6.5% for patients requiring laparotomy within 2 h of arrival [3]. Contrast better delineates intra-abdominal structures but even non-contrast CT has a diagnostic accuracy of 96–97% [11].
Several factors contribute to missed CT diagnosis of appendicitis. Proportion of intraperitoneal fat plays a role with high proportions making missed diagnosis less likely [12]. This patient had sparing amounts of intraperitoneal fat. Accurate history was also noted to be important [12], and a lack of history of right lower quadrant pain on presentation may have contributed to the missed diagnosis. Other key characteristics that pertain to accurate diagnosis include appendiceal thickening, pericaecal fat stranding and/or perforation [12], which were not present in this patient possibly because of subacute presentation.
Other causes of missed appendicitis diagnosis may be concurrent pathology that leads away from a clinical suspicion and therefore from identifying appendicitis. No study looking into this phenomenon was located during literature review; however, there have been case reports of missed appendicitis when the appendix is contained within an umbilical hernia [13]. This may a case of the simplest and first identified cause being presumed to be the only cause.
CONCLUSION
We propose that one possible scenario is appendicitis causing abscess formation, which led to the adhesion of transverse colon and sigmoid colon to the site and subsequent SBO in a tourniquet fashion, which is rare finding at emergency laparotomy.
This case demonstrates the importance of thorough assessment of the entire abdomen at emergency laparotomy to rule out the occurrence of rare antecedent causes of intestinal obstruction and the potential pitfalls of CT imaging. It is a rare case of misdiagnosis with potential contribution from non-ideal patient body habitus, advanced disease and dual pathology. It is a case of two concomitant surgical conditions at emergency laparotomy in a previously well female with a virgin abdomen.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



