-
PDF
- Split View
-
Views
-
Cite
Cite
Alison Zhu, Charis Tan, Graham Meredith, Richard Chard, Minimally invasive surgical resection of a large primary pulmonary hydatid cyst: a thoracoscopic approach, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad090, https://doi.org/10.1093/jscr/rjad090
Close - Share Icon Share
Abstract
Pulmonary hydatid disease is a rare parasitic disease in Australia with few reported cases. The mainstay of treatment in pulmonary hydatid disease is surgical resection followed by medical treatment with benzimidazoles to reduce the risk of recurrence. We present a case of successful resection of a large primary pulmonary hydatid cyst via minimally invasive video-assisted thoracoscopic surgery approach in a 65-year-old gentleman with incidental hepatopulmonary hydatid disease.
INTRODUCTION
Pulmonary hydatid disease is a rare parasitic disease in Australia with few reported cases. Humans serve as intermediate hosts for the causal parasite, Echinococcus granulosus, with the liver and the lungs being most affected. Patients with hydatid cysts are asymptomatic in most cases with risk of damage when cysts exceed 20 cm in diameter with a higher risk of cyst rupture. The goals of treatment in hydatid disease are achieving complete elimination of the parasite, preservation of healthy tissue and prevention of recurrence particularly by avoiding spillage of cystic fluid and dissemination of the cyst contents [1, 2].
The mainstay of treatment in pulmonary hydatid disease is surgical resection followed by medical treatment with benzimidazoles to reduce the risk of recurrence [3]. Surgical approach is often by posterolateral thoracotomy for management of large pulmonary hydatid cysts to allow removal of the cyst without rupture and maximize the preservation of healthy tissue. However, it remains an invasive procedure for patients [4]. With the development of thoracoscopic techniques, video-assisted thoracoscopic surgery (VATS) has been used to minimize the risks of open surgery.
CASE REPORT
A 65-year-old gentleman presented to the emergency department with a 2-week history of lethargy, dyspnoea and non-productive cough. He had no fevers, chills or weight loss and denied any sick contacts. He had recently returned from Samoa 1 month prior where he had worked for two years on a farm with cows, pigs and chickens, with no direct exposure to these animals. He was an ex-smoker, having quit 30 years prior and had no previous history of pneumonia, tuberculosis or COVID-19 infection. He frequently consumed sashimi but did not consume raw or undercooked meat. He had a background history of ureteric stents for renal colic and was otherwise well with no regular medications.
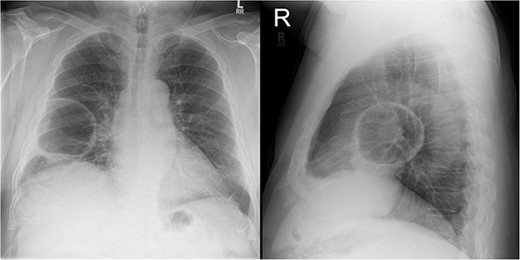
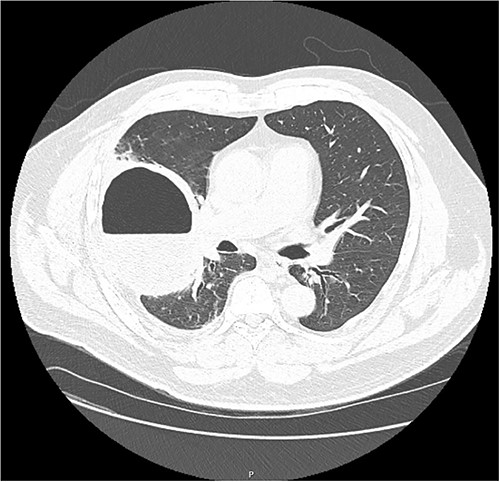
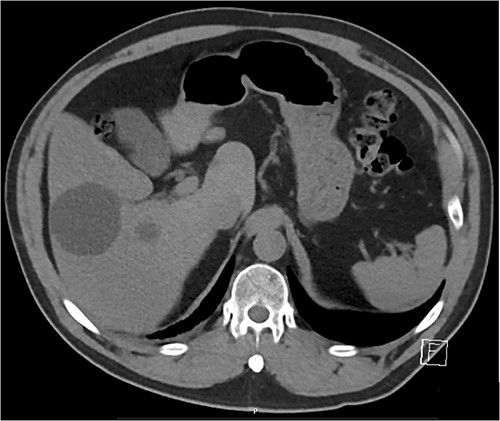
On examination, he appeared well, with no oxygen requirement and reduced air entry in the right mid to lower chest. A chest X-ray (Fig. 1) showed a large cavitating lesion in the right lower zone with a chest computed tomography (CT; Fig. 2) confirming a large lung lesion measuring 100 mm × 80 mm × 100 mm with surrounding ground glass changes. Tests for SARS-CoV-2 and hydatid serology returned positive. He proceeded to have a bronchoscopy and bronchoalveolar lavage that was negative for aspergillus, galactomannan, mycobacterial and fungal cultures, cryptococcus, respiratory viral panel and cytology. A CT abdomen (Fig. 3) revealed multiple hepatic cysts with the largest measuring 59 mm in size in the right lobe. Given the findings of lung and liver lesions, he was commenced on albendazole for presumed extra-hepatic hydatid disease and referred to the cardiothoracic team for resection of the pulmonary hydatid cyst.
The patient underwent elective surgical resection of the hydatid cyst via right-sided VATS. He was positioned in left lateral decubitus with thoracoscopy performed under general anaesthesia with single-lung ventilation with a double-lumen endobronchial tube. Three 10 mm ports were inserted in the fourth mid-axillary intercostal space, the sixth mid-axillary intercostal space and the seventh intercostal space laterally. The cyst was identified, aspirated and irrigated with 10% hypertonic saline as scolicidal agent. Due to the size of the hydatid cyst, cystotomy and capitonnage was deemed not feasible via VATS approach and we proceeded to staple resection en-bloc using GIA staples to prevent formation of a bronchopleural fistula. A single apical chest drain was inserted intra-operatively. Paravertebral blocks were administered under vision and the right lung was inflated under vision with no visible air leak. The ports were removed and closed with absorbable vicryl to the subcutaneous layer and monocryl in subcuticular to the skin. The patient was then extubated in the operating theatre prior to transfer to recovery with an opioid patient-controlled analgesia.
The patient was admitted to the ward post-operatively with the drain remaining until post-operative day 19 due to prolonged air leak. Histopathology returned with clear margins and the patient was discharged home on oral albendazole with follow-up arranged with cardiothoracic surgery, respiratory and infectious diseases specialists. On his most recent follow up at 3 months post-operatively, his VATS wounds have healed well, and he has no symptoms to report. He was continued on oral albendazole for a further month while awaiting repeat hydatid serology.
DISCUSSION
Hydatid disease is a zoonotic parasitic infection that is endemic in sheep- and cattle-raising regions of the world such as in South America, India, the Mediterranean, Australia, New Zealand and the Middle East. The clinical manifestation of hydatid disease is dependent on the site and size of the cyst. Pulmonary hydatid cysts are often asymptomatic until they grow to a size that can cause symptoms, such as dyspnoea, non-productive cough and chest pain [5].
Surgical management of pulmonary hydatid disease involves cystotomy or cystectomy to facilitate removal of the germinative membrane, followed by either evacuation of the cystic contents and capitonnage, or complete resection. In 1993, Becmeur and colleagues were the first to describe the thoracoscopic approach to surgical management of pulmonary hydatid cysts in children [6]. This minimally invasive approach has since been adopted for use in the surgical management of adult hydatid disease with published studies reporting success with cysts of a mean diameter of 7 cm with benefits including reduced operative duration, lower post-operative analgesia requirement, shorter hospital length of stay and improved cosmesis [7, 8]. However, resection by the VATS approach remains limited in the surgical management of larger hydatid cysts due to the increased risk of incomplete removal of the germinative membrane or gross contamination of the thoracic cavity with cystic fluid. Previous case studies have suggested VATS to be utilized for smaller hydatid cysts of less than 5 cm in diameter [9, 10].
This case describes the successful surgical resection of a large primary pulmonary hydatid cyst of 10 cm in diameter via the minimally invasive VATS approach.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
FUNDING
The authors received no financial support for publication of this article.
DATA AVAILABILITY
All data underlying the results are available as part of the article and no additional sources of data are required.



