-
PDF
- Split View
-
Views
-
Cite
Cite
Elaine Kelly, Amy E Murphy, James Byrne, Ahmed Haidaran, An extremely rare case of multiple small bowel intussusceptions in a 20-year-old female, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad688, https://doi.org/10.1093/jscr/rjad688
Close - Share Icon Share
Abstract
Intussusception, which is characterized by the invagination of one portion of the gastrointestinal tract into an adjacent segment, is an uncommon cause of abdominal pain in adults. Given that it is typically associated with identifiable pathological abnormalities, intussusception can pose a diagnostic challenge in adults due to its rarity and nonspecific symptomatology. This report presents a unique case of multiple small bowel intussusceptions in a 20-year-old female, which emphasizes the importance of clinical suspicion and advanced imaging for an accurate diagnosis.
Introduction
Intussusception is a process by which one portion of the gastrointestinal tract invaginates into an adjacent intestinal lumen [1]. It is a rare cause of abdominal pain in adults and typically due to the presence of a well-defined pathological abnormality in the bowel, serving as a lead point [2].
Intussusception can be a challenging diagnosis in adult patients if given its rarity and presentation with nonspecific abdominal pain. A thorough history and clinical examination can often aid in the clinical suspicion of intussusception; however, abdominal imaging such as CT is often required to make the diagnosis. Therefore, it is important to keep it in mind as a rare cause of abdominal pain in adult patients.
Patients will usually be brought to theatre not only for reduction of the intussusception but also to rule out a malignant tumour serving as a lead point. In instances where a lead point cannot be identified, bowel resection is typically not required and reduction of the intussuscepted portion of bowel is sufficient [3].
Case presentation
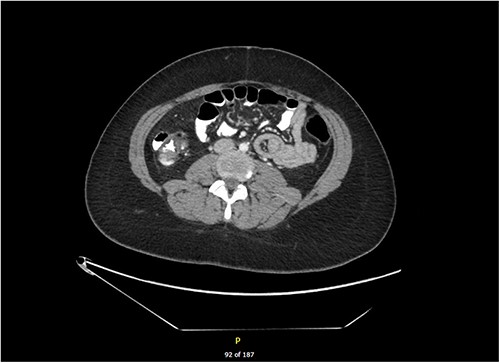
We present the case of a 20-year-old female who presented to the Emergency Department complaining of a 1-day history of sudden onset right iliac fossa pain associated with nausea and vomiting. On examination, her abdomen was soft with tenderness to palpation of the right iliac fossa and suprapubic regions. Her background history consisted of bipolar affective disorder, for which she was taking mirtazapine and aripiprazole. Bloods taken at the time of admission revealed an acute inflammatory process with white cells of 24.5 and a C-reactive protein (CRP) of 76.8. She was referred to the surgical team for work-up of acute appendicitis. She had a pelvic ultrasound to rule out any gynaecological cause of her pain, which showed normal appearance of the uterus and ovaries and was unable to visualize the appendix. She then proceeded to have a CT of her abdomen and pelvis which showed an 8 cm jejunal small bowel intussusception, with no focal bowel lesions or abnormalities within the surrounding mesentery identified (Fig. 1).
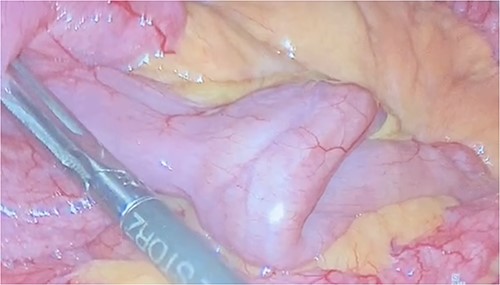
She was taken to theatre for laparoscopic intussusception reduction. A bowel walk was performed in which the small bowel was checked from the ileocaecal valve to the duodenojejunal flexure twice. Our patient was found to have six intussusceptions within the first 100 cm of jejunum with no identifiable lead point (Figs 2 and 3). The intussusceptions were all reduced laparoscopically by starting distally with a bowel grasper and pushing proximally. All reduced easily and the bowel appeared healthy with no signs of intestinal obstruction, bowel ischaemia or intraluminal pathological lesions, and the surrounding mesentery was normal. It was remarked there was some spasmodic and abnormal contraction of the bowel, which may have been a precipitating factor.

Following laparoscopic reduction, her symptoms subsided. She had an unremarkable postoperative recovery, with an inpatient stay of 2 days for monitoring and received buscopan. She was discharged home on buscopan for 1 week and oral esomeprazole for 6 weeks and will be seen in the outpatient clinic 6 weeks following discharge to determine whether further work-up is required.
Discussion
Small bowel intussusception is a rare diagnosis in adults comprising only about 5% of intussusception cases [2]. In 70%–90% of adult patients, there is often an identifiable lead point, such as a tumour or polyp. Alternatively, patients may have predisposing factors such as postoperative adhesions, underlying Crohn’s disease, or a Meckel diverticulum [4, 5].
In our case, only one of the six intussusceptions was identified on CT. There is currently only one other documented case in the literature of such a high number of concurrent intussusceptions, which describe a 25-year-old male with underlying coeliac disease found to have five intussusceptions within the small bowel [6]. In any patient presenting with multiple or recurrent intussusceptions, a diagnosis of Peutz–Jeghers Syndrome must be considered. Peutz–Jeghers Syndrome is an autosomal dominant mutation in the STK11 gene characterized by gastrointestinal polyposis, mucocutaneous pigmentation, and cancer predisposition [7]. Typically, one of the hamartomatous polyps present in the small bowel will serve as a lead point for intussusception. Our patient, however, did not have Peutz–Jeghers and had no predisposing factors or identifiable lead points contributing to intussusception.
Whilst the CT scan only revealed one of the six intussusceptions, this finding was sufficient to bring the patient to theatre for reduction, consequently allowing for discovery and reduction of all six points. Small bowel intussusception may result in small bowel obstruction or bowel ischaemia requiring resection, fortunately our patient did not have features of either. Given that our patient’s intussusceptions were found to be idiopathic, laparoscopic reduction without resection was deemed an appropriate treatment [3].
As evidenced by our case report, small bowel intussusception must be considered as a rare cause of right iliac fossa pain in adults. It also highlights the importance of performing a CT scan as a first-line investigation in patients presenting with abdominal pain, even in females of childbearing age. Abdominal CT has been found to be a superior imaging modality for the diagnosis of intussusception compared to contrast studies, ultrasonography, and endoscopy [8]. Moreover, it illustrates how vital it is to perform a thorough small bowel walk from the ileocaecal valve to the duodenojejunal flexure at least twice, such as not to miss this diagnosis and prevent progression to obstruction and ischaemia.
This case presentation describes an extremely rare phenomenon of the presence of six simultaneous intussusceptions within the proximal jejunum, deemed to be idiopathic in nature. There are currently no other similar cases documented in the literature. Intussusception, whilst uncommon, must be considered as a possible differential diagnosis in patients presenting with right iliac fossa pain due to the risk of bowel ischaemia and obstruction.
Conflict of interest statement
None declared.
Funding
None declared.



