-
PDF
- Split View
-
Views
-
Cite
Cite
Makoto Miyamae, Ryotaro Urabe, Kunihiro Nakai, Usefulness of perforating branches of the deep femoral artery and vein as recipient vessels during free-flap reconstruction for extensive defects of the thigh, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad683, https://doi.org/10.1093/jscr/rjad683
Close - Share Icon Share
Abstract
The perforating branches of the deep femoral artery and vein are considered useful recipient vessels during free-flap reconstruction for extensive defects extending from the knee to the mid-thigh or from the lateral to the posterior region of the thigh. Despite being located deep between the adductor longus and magnus muscles, they can be easily identified, allowing for a sufficient surgical field for the vascular anastomosis. Approximately four perforators from the deep femoral artery can be found on the posterior aspect of the thigh, easily identified by dissecting the semitendinosus and biceps femoris muscles. The calibre and length of the perforators were suitable for vascular anastomosis. In this study, we present three cases of free-flap reconstruction for extensive thigh defects using perforating branches of the deep femoral artery and vein as recipient vessels.
Introduction
Free-flap reconstruction is required when extensive tissue defects occur in the thigh after resecting malignant soft tissue tumours or decubitus ulcers in the trochanteric area. However, unlike for head and neck reconstruction [1, 2], there are no standard recipient vessels for femoral reconstruction [3, 4]. Appropriate recipient vessels should be selected by considering various factors, such as the location and extent of the defects, the presence or absence of infection or injury, flap placement, and intraoperative position. Here, we investigated free-flap reconstruction using perforating branches of the deep femoral artery and vein as recipient vessels for extensive thigh defects.
Case report
Case 1
A 59-year-old man noticed a bulge in the front of his right thigh 5 months before visiting our department. Magnetic resonance imaging (MRI) revealed a mass measuring 160 × 90 × 80 mm in the proximal thigh, 110 × 40 × 30 mm in the middle thigh, 110 × 70 × 50 mm in the distal anterior region, and 45 × 25 × 25 mm in the distal posterior region of the thigh, and was diagnosed with recurrent dedifferentiated liposarcoma.
The patient underwent extensive tumour resection (femoral and quadriceps and sartorius muscle resection, and partial resection of the adductor muscle) and total femoral replacement (Fig. 1a). Reconstruction using an 11 × 36 cm free latissimus dorsi myocutaneous flap was performed for the skin defect on the front of the thigh (Fig. 1b). The deep femoral artery and vein were identified between the adductor longus and adductor magnus muscles, which were not affected by the surgery. The second perforating branches of the deep femoral artery and vein were used as the recipient vessels. The thoracodorsal artery and vein, responsible for supplying blood in the latissimus dorsi myocutaneous flap, were anastomosed to the second perforating branches of the deep femoral artery and vein (Fig. 1c). The postoperative course was uneventful.
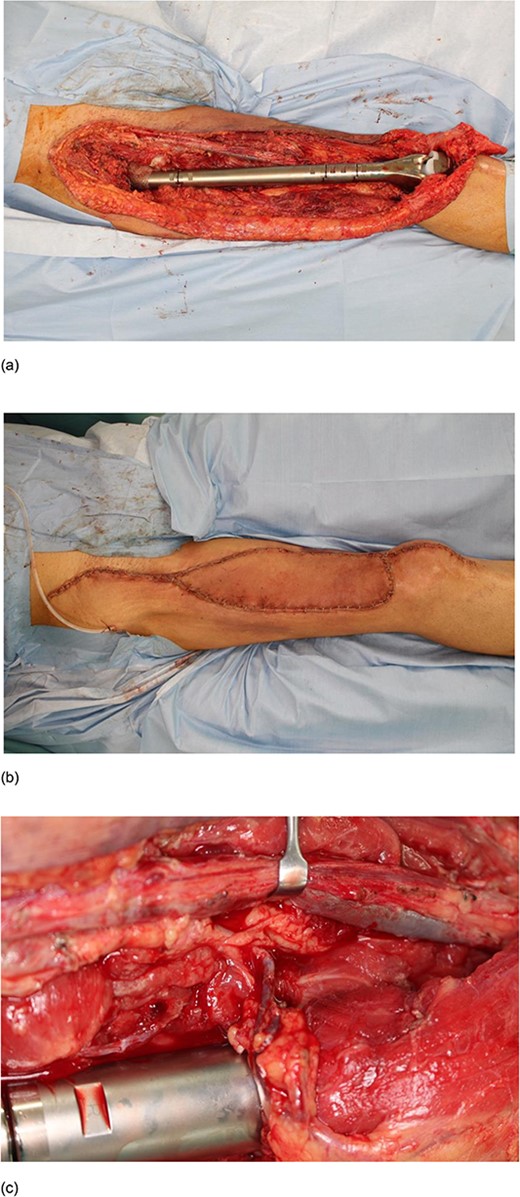
Intraoperative photographs of Case 1. A 59-year-old man underwent extensive tumour resection of the front of the thigh and reconstruction by free latissimus dorsi myocutaneous flap. (a) The skin defect on the front of the thigh after the extensive tumour resection. (b) Skin coverage after the reconstruction by free latissimus dorsi myocutaneous flap. (c) The thoracodorsal artery and vein, which feed the latissimus dorsi myocutaneous flap, were anastomosed to the second perforating branches of the deep femoral artery and vein, respectively.
Case 2
A 53-year-old man noticed a bulge inside his left thigh that had been present for 4 months before his visit. MRI revealed a 10 × 10 × 19 mm mass on the medial distal thigh, and was then diagnosed with sarcoma. He underwent extensive tumour resection (partial resection of the gracilis, semitendinosus, semimembranosus, sartorius, and adductor muscles) (Fig. 2a). We used a 19 × 32 cm free latissimus dorsi myocutaneous flap to reconstruct the skin defect from the medial thigh to the medial knee joint (Fig. 2b). The deep femoral artery and vein were identified between the adductor longus and adductor magnus muscles. Subsequently, the terminal branches of the deep femoral artery and vein were carefully selected as the recipient vessels. The thoracodorsal artery and vein, responsible for supplying blood in the latissimus dorsi myocutaneous flap, were anastomosed to the terminal branches of the deep femoral artery and vein (Fig. 2c).
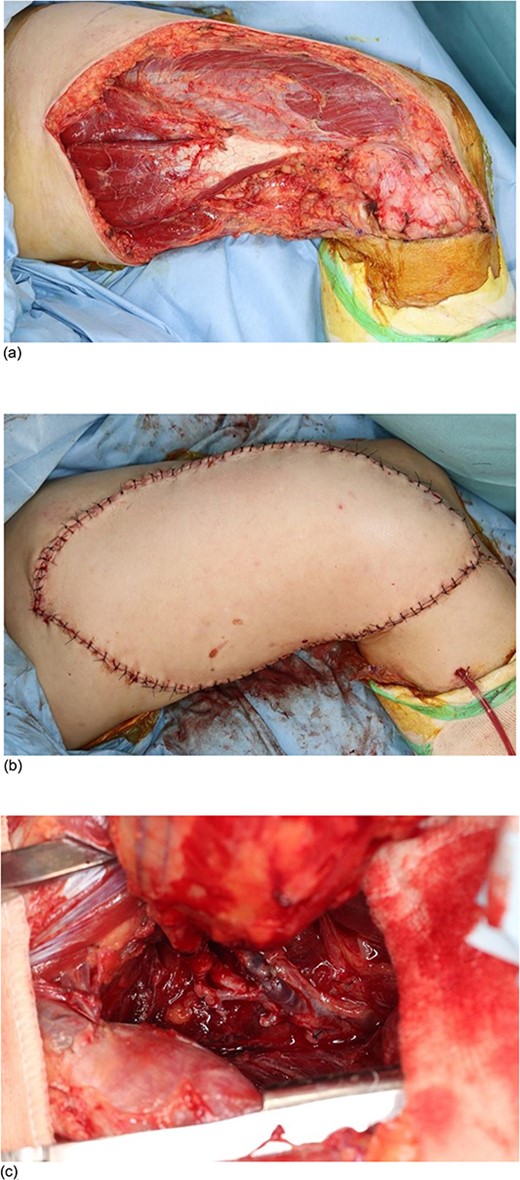
Intraoperative photographs of Case 2. A 53-year-old man underwent extensive tumour resection of the medial distal thigh and reconstruction by free latissimus dorsi myocutaneous flap. (a) The skin defect from the medial thigh to the medial knee joint after the extensive tumour resection. (b) Skin coverage after the reconstruction by free latissimus dorsi myocutaneous flap. (c) The thoracodorsal artery and vein, which feed the latissimus dorsi myocutaneous flap, were anastomosed to the terminal branches of the deep femoral artery and vein.
The postoperative course was uneventful.
Case 3
A 73-year-old man presented with a decubitus ulcer on the left greater trochanter. Despite initial conservative treatment, the lesions rapidly worsened. The ulcer was 16 × 16 cm and extended below the gluteus maximus muscle.
The patient underwent debridement of the left greater trochanteric ulcer (Fig. 3a). Reconstruction was performed using a 19 × 32 cm free latissimus dorsi myocutaneous flap to address the skin defect on the lateral thigh (Fig. 3b). Due to the suspected damage caused by the infection, the inferior gluteal, superficial circumflex iliac, and lateral circumflex femoral arteries were considered compromised. To identify suitable recipient vessels, an additional skin incision was made caudal to the skin defect, revealing the second and third perforators passing through the adductor magnus muscle between the biceps femoris and semimembranosus/semitendinosus muscles. As the second perforator appeared narrow and potentially damaged, the third perforating branches of the deep femoral artery and vein were used as the recipient vessels. Finally, the thoracodorsal artery and vein responsible for supplying blood in the latissimus dorsi myocutaneous flap were anastomosed to the third perforating branches of the deep femoral artery and vein (Fig. 3c). Postoperatively, part of the flap margin became necrotic but healed after performing debridement and re-suturing. The patient’s postoperative course was uneventful thereafter.
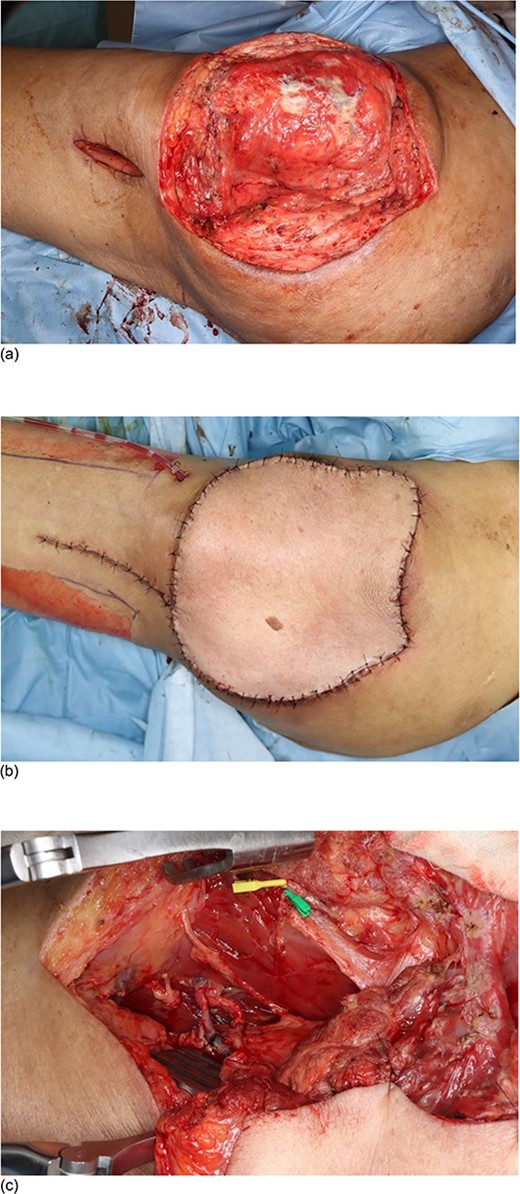
Intraoperative photographs of Case 3. A 73-year-old man underwent debridement for a left greater trochanteric ulcer and reconstruction by free latissimus dorsi myocutaneous flap. (a) The skin defect on the lateral thigh after the debridement of the ulcer. (b) Skin coverage after the reconstruction by free latissimus dorsi myocutaneous flap. (c) The thoracodorsal artery and vein, which feed the latissimus dorsi myocutaneous flap, were anastomosed to the third perforating branches of the deep femoral artery and vein.
Discussion
In our three cases, the recipient vessels for free-flap reconstruction of the thigh were the second, third, and terminal perforating branches of the deep femoral artery and vein. The defects are located on the anterior surface of the thigh, medial, and lateral sides of the thigh.
The recipient vessels used in free-flap reconstruction in the thigh include the inferior gluteal, superficial circumflex iliac, lateral circumflex femoral, descending genicular, and medial sural artery [3, 4]. Branches and perforators are used frequently [5]. The descending branch of the lateral circumflex femoral artery is easily selected because the dissection technique is the same as that used for harvesting the anterolateral thigh flap [6]. The descending genicular and medial sural arteries are often used because they are close to the knee area, where reconstructive surgery is frequently required [4, 7].
However, the deep femoral artery and vein are rarely selected as recipient vessels for free-flap reconstruction of the knee, which is the most common amongst reconstructive surgeries of the thigh, because they are far from the knee region. In patients with extensive defects extending from the knee to the mid-thigh, the deep femoral artery and vein are convenient locations to use as recipient vessels. Despite their deep location between the adductor longus and magnus muscles, they can be easily identified and may provide a sufficient surgical field for vascular anastomosis. Approximately four perforators from the deep femoral artery also run on the posterior aspect of the thigh and can be easily identified by dissecting the semitendinosus and biceps femoris muscles [8]. These perforators are of calibre and length suitable for vascular anastomosis [8]. Dissection and anastomosis of the deep femoral artery and vein were feasible in the supine position and in the lateral and prone positions.
The incidence of venous insufficiency is considerably higher when the superficial venous system is used as the recipient vein in free-flap reconstruction of the lower extremity than when the deep venous system is used [9]. Using the perforating branches of the deep femoral vein of the deep venous system as the recipient vein results in safer reconstruction.
In conclusion, the perforating branches of the deep femoral artery and vein are considered useful recipient vessels during free-flap reconstruction for extensive defects extending from the knee to the mid-thigh or from the lateral to the posterior region of the thigh.
Conflict of interest statement
None declared.
Funding
None declared.



